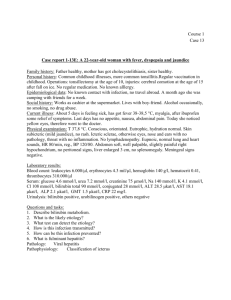
Case 1: A 40 year old man was admitted to an emergency clinic
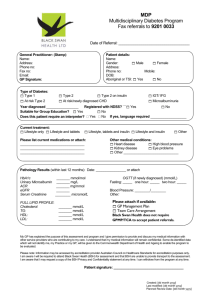
advertisement

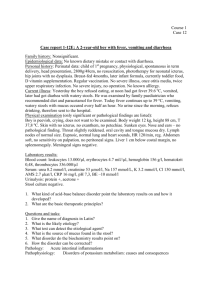
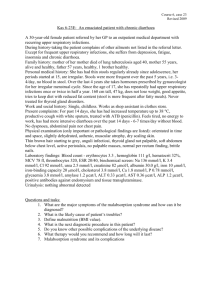
Case 1: A 40 year old man was admitted to an emergency clinic complaining of mild abdominal pain and vomiting. He stated that he had had a bout of watery diarrhea shortly after eating a spaghetti meal which was prepared by his wife. Physical exam revealed the following findings (normal values in parentheses): Heart rate: 130/min (70/min) Blood pressure: normal Respiratory rate: 30/min (15/min) Skin and mucous membranes were moist. Pupils were 2 mm in diameter (miosis) and nonreactive. Apart from being slightly lethargic, the patient had clear mentation. Abdominal auscultation revealed a hyperactive bowel; however, there was no blood in the stool. Neurological examination was normal. Auscultation of the thorax revealed increased bronchial tones with excessive bronchial secretions and wheezing. Over the next hour the patient developed severe respiratory distress, cyanosis and pulmonary edema that required intubation. He became extremely weak and muscle fasciculation began to develop. 1. Try to propose the differential diagnosis. 2. Could it be organophosphate poisoning? 3. Which signs and symptoms of organophosphate poisoning has the patient developed? 4. Which other may further develop? What are the mechanisms? 5. Could it be an attempt to kill him by spaghetti meal? 6. (What are the routes of organophosphate poisoning?) Case 2: A 35-year-old man presented with elevated blood pressure (188/112, seated) at a yearly physical exam. Previous exams noted blood pressures of 160/94 and 158/92. On questioning, he admitted episodes about twice a month of apprehension, severe headache, perspiration, rapid heartbeat, and facial pallor. These episodes had an abrupt onset and lasted 10-15 minutes. 30 min after the initial blood pressure measurement, the seated blood pressure was 178/110 with a heart rate of 90. The blood pressure after 3 min of standing was 152/94 with a heart rate of 112. The optic fundi showed moderately narrowed arterioles with no hemorrhages or exudates. Routine hematology and chemistry studies were within the reference ranges and a chest film and EKG were essentially normal. 1. What might be the reason of the attacks of high pressure in this man? 2. Are the consequences of increased secretion of epinephrine the same as o epinephrine? 3. Why does he not have any other changes (laboratory, EKG)? Might he have any? 4. What is necessary to evaluate? 5. Does the patient have some signs and symptoms between attacks? 1 6. How might be the attacks provoked? 7. Why should the surgical treatment take place as soon as possible? Case 3: A 58-year-old woman was brought to the emergency with repeated vomiting and worsening of weakness and fatigue. History: The patient was repeatedly hospitalized for asthma in the past, which was then controlled by corticoid oral spray. She has been on this medication for 5 years and has not been hospitalized since. She recently (about 3 weeks ago) ran out of the spray. Since that time she did not take any medications. Over the past week she has been feeling weak and tired and has been lightheaded when standing from sitting position. Over the past few days she developed nausea with episodes of vomiting and cramping abdomen. Physical evaluation: The patient is a middle-aged, centrally obese woman with thin limbs. She has rounded face, “buffalo hump” and purple striae over the trunk. Blood pressure 74/40, pulse 105, respiratory rate 18/min. the patient was oriented, complaining of dizziness. Laboratory findings: Na+ K+ ClUrea Bicarbonate Serum creatinin Ca2+ Glucose On admission 127 5,8 95 14,3 22 70 2,55 3,3 Standart 135 -145 mmol/l 3,5-5 mmol/l 97- 108 mmol/l 2,0 – 7,5 mmol/l 22 – 26 mmol/l 65 – 100 umol/l (žena) 2,25 -2,75 mmol/l 3,5 – 6,1 mmol/l 1. What is the most likely cause of the patient's characteristic appearance? 2. What could be the cause of the current state of this patient? 3. Why has the patient hypoglycemia ? 4. Describe the metabolism of potassium in this patient. 5. Why is urea high and creatinin almost normal? 6. What changes in her ABR do you should expect? Explain. 7. What would happen if the patient did not come to the doctor? 2