Chapters 21: The Respiratory System
advertisement

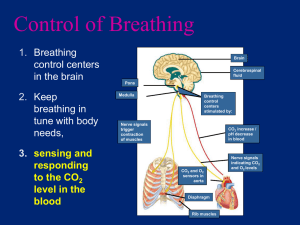
Chapter 21: The Respiratory System Objectives: 1. 2. 3. 4. 5. 6. Distinguish between conducting and respiratory zone structures List and describe several protective mechanisms of the respiratory system. Describe the makeup of the respiratory membrane, and relate its structure to its functions. Describe the gross structure of the lungs and pleura coverings. Relate Boyle’s law to the events of inspiration and expiration. Explain the relative roles of the respiratory muscles and lung elasticity in producing the volume changes that cause air to flow into and out of the lungs. 7. Explain the functional importance of the partial vacuum that exists in the intrapleural space. 8. List several physical factors that influence pulmonary ventilation. 9. Define dead space. 10. Describe, in general terms, how atmospheric and alveolar air differ in composition, and explain these differences. 11. State Dalton’s Law of partial pressures and Henry’s Law. Relate each to events of external and internal respiration. 12. Describe how oxygen is transported in the blood, and explain how oxygen loading and unloading is affected by temperature, pH, BPG and Pco2. 13. Describe carbon dioxide transport in the blood. 14. Describe the neural controls of respiration. 15. Compare and contrast the influences of lung reflexes, volition, emotions, arterial pH, and partial pressures of oxygen and carbon dioxide in arterial blood on respiratory rate and depth. 16. Compare the causes and consequences of chronic bronchitis, emphysema, asthma, and lung cancer. Conducting zone structures: deliver gases to and from respiratory zone structures. They include the upper respiratory tract, trachea, and bronchial tree up to the terminal bronchioles. They warm, moisten, and filter the air. See figure 21.3, 21.4, 21.5, 21.7, 21.11, Table 21.1 Respiratory zone structures: where gas exchange occurs. They include respiratory bronchioles, alveolar ducts, and alveoli. See figure 21.8, 21.9, Table 21.1 Boyle’s law: V1P1 = V2 P2 If pressure increases, volume decreases, or if volume increases, pressure decreases. Atmospheric pressure: 760 mmHg at sea level. Intrapulmonary pressure or Palv: pressure within the lungs, specifically the alveoli, rises and falls with breathing, but always equalizes itself with atmospheric pressure outside the body. See figure 21.12, 21.14 Intrapleural pressure or Pip: pressure within the pleural cavity surrounding the lungs; it is always about 4 mmHg less than pressure in alveoli and atmosphere; referred to as negative pressure. See figure 21.12, 21.14 Establishment of intrapleural pressure Intrapleural pressure is always negative with respect to intrapulmonary pressure, so what causes this? The lungs have a natural tendency to recoil due to elastic fibers around alveoli, and therefore occupy the smallest size possible. The lungs also contain alveolar fluid which tends to pull the alveolar walls together because of surface tension. However, the natural elasticity of the chest wall tends to pull the thorax outward to enlarge the lungs. But the strong adhesive force between the parietal and visceral pleura, with pleural fluid in between, secure them together in the same way that a drop of water holds two glass slides together. They slide past one another but are closely apposed and separating them requires extreme force. The net result of the interaction of these forces is a negative intrapulmonary pressure. Pleural fluid, though, must remain at a minimum and is removed constantly by the lymphatics. See figure 21.10, 21.12 Atelectasis: immediate lung collapse occurs when Palv and Pip equalize. Too much fluid buildup (due to inflammation) or air in the pleural cavity will result in atelectasis. Air can enter through a chest wound, or rupture of visceral pleura, allowing air from respiratory tract to enter. Common result of pneumonia Pneumothorax: presence of air in intrapleural space. Reversed by closing the “hole” and drawing air out of intrapleural space with tubes. Because each lung is in its own pleural cavity, collapse of one lung does not mean the other will collapse, too. Ventilation: a change in volume causes a change in pressure that causes flow of gases (due to Boyle’s law). Gases are always flowing from areas of high pressure to low pressure. Inspiration: if volume of chest cavity increases, pressure inside lungs decreases and air rushes in (like a bellows). Palv < Pip Quiet inspiration: the action of the diaphragm causes an increase in cavity volume. The action of the intercostals muscles lifts the rib cage and pulls sternum forward. Inspiration ends when pressure is equalized. Abdominal muscles are used in deep or forced inspiration. See figure 21.13, 21.14 Expiration: quiet expiration is passive due to relaxation of muscles and elasticity of lungs. Volume decreases and pressure increases so that air leaves. Palv > Pip Forced expiration requires abdominal wall muscles to increase intra-abdominal pressure and depress the ribcage. See figure 21.13, 21.14 Factors influencing pulmonary ventilation 1. Airway resistance: impairs ventilation through friction or drag. Small differences in pressure produce large changes in volume of gas flow. Average pressure difference is only about 2 mmHg but moves 500 ml of air. But gas flow changes inversely with resistance. Since gas flow stops at terminal bronchioles and diffusion takes over as main force driving gas movement, the greatest resistance is in mediumsized bronchi. See figure 21.15 Bronchial diameters are sensitive to neural controls and chemicals: the parasympathetic N.S. and histamine cause constriction, the sympathetic causes dilation. 2. Alveolar surface tension forces: impair ventilation. Surfactant, a detergent-like complex of lipids and proteins helps to reduce surface tension so the alveoli do not stick together. IRDS (infant respiratory distress syndrome) occurs with a lack of surfactant in premature babies. 3. Lung compliance: enhances ventilation. Compliance is the ease with which the lungs can be expanded. A higher compliance makes it easier to expand lungs. It can be diminished by 1. reduced resilience of lungs (fibrosis – scar tissue) 2. blockage of smaller respiratory passages with fluid or mucus 3. reduced surfactant 4. decreased flexibility of rib cage Dead space: air that fills conducting passages but never contributes to gas exchange in alveoli ( 150 ml or about 1 ml of air per lb of wt). If TV = 500 ml, then only 350 ml is ventilated. There is alveolar dead space if alveoli are not functioning. Alveolar ventilation: AVR = frequency X (TV – dead space) (ml/min) (bpm) (ml/breath) depth of breathing enhances alveolar ventilation more than rate, because dead space is constant. AVR drops during shallow, rapid breathing. See Table 21.2 Gas Exchange Dalton’s law of partial pressure: pressure of each gas is directly proportional to its percentage in a gas mixture. PO2 = 159 mmHg @ sea level See table 21.4 PO2 = 110 mmHg @ 10,000 PO2 = 3040 mmHg @ 99’ below Henry’s law: each gas will dissolve in liquid in proportion to its partial pressure. The volume of gas that will dissolve in liquid at any given partial pressure also depends on solubility of gas in liquid and temperature of liquid. CO2 is most soluble. O2 has 1/20 solubility of CO2. Solubility decreases with increasing temperature. Alveolar gas: 13.7% O2. PO2 = 104 mmHg See table 21.4 Gas exchanges between blood, lungs, tissues See figure 21.17 Depends on: 1. Partial pressure gradients and gas solubilities 2. Functional aspects, ventilation and perfusion 3. Structural characteristics 1. PO2 of venous blood: 40 mmHg. PO2 of alveoli = 104 mmHg. Therefore, O2 diffuses rapidly from alveoli to pulmonary capillary blood. PCO 2 of venous blood = 45 mmHg; PCO2 of alveoli = 40 mmHg. CO2 is 20x more soluble in plasma than O2. See figure 21.19 2. When PO2 is low: blood is shunted to areas of higher PO2. In high areas, arterioles dilate. PCO2 levels change diameters of bronchioles. In areas of high PCO2, bronchioles are dilated so that CO2 can be eliminated. See figure 21.19 PO2 and PCO2 = dilation of pulmonary capillaries and constriction of bronchioles PO2 and PCO2 = constriction of capillaries and dilation of bronchioles 3. Respiratory membrane: consists of wall of alveolus and wall of capillary. o o o o It is only about 0.5 – 1.0 m thick. Diffusion occurs across this membrane. During pneumonia the exchange membrane thickens and time of blood flow is insufficient for gas exchange. Surface area in alveoli is 40x greater than skin Emphysema occurs when the walls of adjacent alveoli break through and alveoli become larger. Tumors, mucus, or inflammatory material blocks gas flow. Gas exchange in tissues: PO2 in tissues is lower than in arterial blood (40 mmHg vs. 104 mmHg) See figure 21.17 Oxygen transport by blood See figure 21.22 Dissolved in plasma: 1.5% Bound to Hb (hemoglobin) as oxyhemoglobin (HbO2): 98.5% Also present, deoxyhemoglobin HHb HHb + O2 HbO2 + H+ (in lungs) (in tissues) PO2, temperature, blood pH, PCO2 and BPG in blood regulate O2 binding Dissociation curve: indicates binding of Hb with O2 See figure 21.20, 21.21 temp, PCO2, H+ or BPG and Hb binding shifts curve to right. This enhances O2 unloading from blood A decrease in the conditions above and Hb binding shifts the curve to left and more O2 binds. Bohr effect: decreased pH (acidosis) weakens HbO 2 binding in tissues. O2 unloading is accelerated where it is most needed (ie. In the tissues) Impairments of Oxygen transport Anemic hypoxia: too few RBC’s or Hb Ischemic hypoxia: blood circulation is impaired: congestive heart failure and emboli Histotoxic hypoxia: poisons (cyanide) Hypoxemic hypoxia: PO2, carbon monoxide poisoning Carbon dioxide transport See figure 21.22 1. Dissolved in plasma: 7-10% 2. HbCO2 (carbaminohemoglobin): binds to globin 20% 3. Bicarbonate ion in plasma: 70% CO2 + H2O H2CO3 H+ + HCO3- (memorize this equation!) This occurs faster in RBC’s because of carbonic anhydrase. H+ are released to lower pH which enhances O2 release and more CO2 loading. HCO3- is then carried in plasma. Cl- then moves into RBC’s to counteract loss of negative ions. In lungs, HCO3- goes into RBC’s (Cl- goes out), joins with H+ to make H2CO3 and is split by carbonic anhydrase into CO2 and H2O. Haldane Effect: PO2 and Hb saturation means CO2 can be carried. As CO2 enters systemic bloodstream, more O2 leaves Hb (Bohr effect) and more CO2 can combine and more HCO3- forms (Haldane effect). In pulmonary circulation, uptake of O2 facilitates release of CO2. As Hb becomes saturated w/ O2 , H+ is released, combines w/ HCO3- and CO2 is unloaded from pulmonary blood. See figure 21.23 Carbon dioxide and blood pH: changes in respiratory rate or depth produce changes in pH by altering H2CO3 in blood. Slow, shallow breathing causes a drop in pH (more H2CO3 ). Rapid, deep breathing flushes CO2, with a decrease in H2CO3 Control of Respiration See figure 21.24 Medulla oblongata 1. Ventral respiratory group: a network of neurons which appear to be the rhythm-generating and integrative center. Some neurons fire during inspiration, while others fire during expiration. When the inspiratory neurons fire, the diaphragm and external intercostal muscles contract. When the expiratory neurons fire, the signals to the inspiratory muscles stop, relaxation occurs, and the lungs recoil. This cyclic on/off activity repeats continuously to produce a respiratory rate of 12-15 bpm. 2. Dorsal respiratory group: integrates input from the peripheral stretch and chemoreceptors and communicates this information to the VRG. Pons Pontine respiratory centers: transmit impulses to the VRG to modify and fine-tune the breathing rhythms generated by the VRG during certain activities such as talking, sleep, and exercise. They receive input from higher brain centers and various sensory receptors in the body. Genesis of Respiratory Rhythm: The most popular hypothesis for this that two interconnected neuronal networks in the medulla inhibit each other and so cycle their activity to generate the rhythm. Factors Influencing Breathing Rate and Depth Chemical Factors PCO2 : CO2 levels are the most potent in influencing respiration. As CO2 levels rise, a condition called hypercapnia exists. CO2 in the CSF from the blood decreases pH through the same reaction that occurs in the RBC’s and central chemoreceptors in the ventrolateral medulla are stimulated to increase breathing rate. While rising CO2 levels begin the change in breathing rate, it is the regulation of H+ concentration in the brain that truly drives respiration rates. In summary, pH and CO2 stimulate rapid breathing. When PCO2 levels are abnormally low, apnea may occur. In summary, pH and CO2 stimulate breath holding. PO2 : peripheral chemoreceptors, the aortic and carotid bodies, must detect a mmHg before oxygen is a major stimulus for increased ventilation. PO2 of less than 60 Arterial pH: a drop in pH causes a rise in ventilation Exercise: increases ventilation due to use of O2 and generation of CO2 High altitude: increases ventilation due to low PO2 in atmosphere Pulmonary irritant reflexes: communicate with respiratory centers via vagus nerve. Mucus, dust, lint, cigarette smoke stimulate receptors in bronchioles that promote constriction, coughing, sneezing. Inflation reflex: Hering-Breuer reflex. Stretch receptors in lungs are stimulated when lungs inflate and send inhibitory impulses to vagus nerve and medullary respiratory centers to end respiration. Stretch receptors become quiet as lungs recoil – a protective rather than regulatory mechanism. Hypothalamic control: emotions and pain can increase or decrease rate. Cortical (cerebral cortex) control: voluntary control, except when CO2 levels are too high and brain stem reinitiates breathing Chronic obstructive pulmonary disease (COPD): common features 1. smoking 2. dyspnea: labored breathing 3. coughing and pulmonary infections 4. respiratory failure Obstructive emphysema Permanent enlargement of alveoli, lungs, lose elasticity Exhaustion occurs from breathing and “barrel chest” develops Chronic bronchitis Inhaled irritants lead to excessive mucus production, inflammation and fibrosis occur in mucosa. Airways become obstructed, frequent infections Asthma Coughing, dyspnea, wheezing, chest tightness. Begins as inflammation of airway, then bronchospasms affect lack of airflow. Tuberculosis Infection of tubercle bacillus that grows in lungs. Body forms granulomas around organism in response to its presence. Tubercles result. Lung cancer Caused primarily by cigarette smoke. Metastasizes rapidly and widely. Cystic fibrosis Genetic disease where chloride channels are not working properly and thick mucus is produced. Clogs lungs and infections occur.