Nd:YAG - 1064 nm
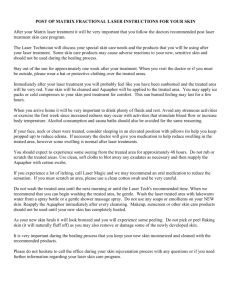
advertisement

LASER : VARICOSITES DES MEMBRES INFERIEURS Mise à jour SFLM - FEVRIER 2011 GENERALITES Lasers Surg Med 1987;7(3):219-23 Study of three laser systems for treatment of superficial varicosities of the lower extremity Apfelberg DB, Smith T, Maser MR, Lash H, White DN Three separate laser modalities were investigated in the treatment of superficial varicosities/telangiectasias of the lower extremities. Sixteen patients were treated and followed for 12 m onths. The superpulse CO2, the pulsed focally specific CO2, and the Nd:YAG laser transmitted through a diffusing sapphire tip were able to produce cosmetically satisfactory permanent obliteration of vessels after a 12-month follow-up interval. These results were a significant improvement over six-month results indicating a long fading time for laser treatment of leg veins. Zentralbl Chir 1993;118(7):383-9 Use of laser in vascular surgery Berlien HP, Philipp C, Engel-Murke F, Fuchs B The use of lasers in the field of vascular surgery concerns 3 completely different principles of application. The main field is the therapy of hemangiomas and congenital vascular diseases (CVD). The experience of the therapy of congenital diseases can be also used in the treatment of varicosis, especially in the treatment of the perforating veins. In contrast to the angioplasty, where the therapeutic aim is recanalisation of an arterial vessel, in the venous system it is the occlusion of a vessel. The thermal procedures using argon- or Nd:YAG lasers with hot tips, saphire tips or with the bare fiber are no longer relevant. Only photoablation using pulsed lasers is able to remove calcified material. The excimer laser is currently the best known system for angioplasty. New developments, for example solid state lasers like the holmium laser, have as yet to show their advantages. A main emphasis of research should be the improvement of catheter systems since present applications are limited by those currently available catheter systems. Tissue fusion is still an experimental procedure. There is a lot of basic research to be done to establish this procedure in the clinical routine. J Dermatol Surg Oncol 1993 Jan;19(1):74-80 Cool laser optics treatment of large telangiectasia of the lower extremities Chess C, Chess Q BACKGROUND. Lower extremity telangiectases have been traditionally treated using sclerotherapy. However, because of significant side effects from sclerotherapy, laser treatments have been investigated. Results from laser treatments have been generally unsatisfactory. OBJECTIVE. This study was based on the premise that simultaneous cooling and lasing would permit more effective treatment. METHODS. Thirty lower extremity telangiectases on 13 patients were treated by a technique of simultaneous cooling and lasing. Argon (488/514 nm) and argon dye (577 nm, 585 nm) laser light were delivered through a new cooling device to telangiectatic vessels of approximately 1-mm diameter on the thigh and leg. Pulsed and continuous beam treatments were utilized at high levels of irradiance. RESULTS. Sixty-seven percent of treated sites were improved; half of these were completely or nearly completely cleared. There were no complications. In only 2 of 30 (7%) treated sites were there persistent pigmentary changes. CONCLUSION. These results compare favorably with other methods for treatment of lower extremity telangiectases. Successful treatment of large lower extremity telangiectases by simultaneous cooling and lasing with minimal side effects suggests a reduction of thermal injury to nonvascular tissue while allowing destruction of ectatic vasculature. Lasers Surg Med 1997;20(3):346-53 Optimal parameters for laser treatment of leg telangiectasia Kienle A, Hibst R BACKGROUND AND OBJECTIVE: The optimal parameters for treatment of leg telangiectasia with a pulsed laser are investigated. STUDY DESIGN/MATERIALS AND METHODS: The Monte Carlo method is used to calculate the light penetration and absorption in the epidermis, dermis, and the ectatic blood vessel. Calculations are made for different diameters and depths of the vessel in the dermis. In addition, the oxygen saturation of the blood vessel, the laser beam diameter, and the laser irradiation profile is varied. RESULTS: It is found that for vessels with diameters between 0.3 mm and 0.5 mm wavelengths about 600 nm are optimal to achieve selective photothermolysis for the considered damage model. It is also shown that an elliptical laser beam area has advantages compared to a circular beam area for treatment of leg telangiectasia. CONCLUSIONS: We recommend the treatment of leg telangiectasia with dye laser wavelengths longer than the normally used 577 nm and 585 nm. Dermatol Surg 1999 Apr;25(4):328-35; discussion 335-6 The role of lasers and light sources in the treatment of leg veins Dover JS, Sadick NS, Goldman MP Telangiectasia of the legs occurs in 29% to 41% of women in the United States. The variation in size, flow, depth, and type preclude the possibility of a single effective treatment modality. When a systematic approach is used where feeder vessels are first surgically removed and sclerotherapy proceeds from largest to smallest vessels, 80-90% of vessels respond to a single sclerotherapy treatment. Because of the relatively modest results demonstrated with lasers and light sources and the high rate of success and the relatively low cost of ambulatory phlebectomy, compression sclerotherapy and superficial sclerotherapy, we generally recommend using lasers and light sources only for vessels that remain after this treatment approach. Lasers and light sources should be considered prior to sclerotherapy in patients who are fearful of needles, who do not tolerate sclerotherapy, who fail to respond to sclerotherapy, or who are prone to telangiectatic matting. Carefully monitored, controlled studies are essential to better define the role of the available laser and light sources in the treatment of leg veins. Lasers Surg Med 2000; 26(2):158-63 New approaches to the treatment of vascular lesions Dover JS, Arndt KA BACKGROUND AND OBJECTIVE: The pulsed dye laser was developed based on the concept of selective photothermolysis. By using a wavelength of light well absorbed by the target and pulse duration short enough to spatially confine thermal injury, specific vascular injury could be produced. STUDY DESIGN/MATERIALS AND METHODS: Although the pulsed dye laser revolutionized the treatment of port wine stains (PWS) and a variety of other vascular lesions, the ideal thermal relaxation time for the vessels in PWS is actually 1-10 ms, not 450 micros of the original pulsed dye laser machines. These original theoretical calculations recently have been proven correct in a study that used both an animal vessel model and in human PWS. RESULTS: Longer wavelengths of light, within the visible spectrum, penetrate more deeply into the skin and are more suitable for deeper vessels, whereas longer pulse durations are required for larger caliber vessels. CONCLUSION: A variety of lasers recently have been developed for the treatment of vascular lesions which incorporate these concepts into their design, including pulsed dye lasers at 1.5 ms, a filtered flash-lamp pulsed light source with pulse durations of 1-20 ms, several 532-nm pulsed lasers with pulse durations of 1 ms to as high as 100 ms, long pulsed alexandrite lasers at 755 nm with pulse durations up to 20 ms, pulsed diode lasers in the 800 to 900 nm range, and long pulsed 1064 Nd:YAG sources. Les lasers vasculaires sont exploités depuis les années 80 ; ils présentent une alternative intéressante à la greffe cutanée pour le traitement des angiomes plans y compris sur les membres inférieurs. Depuis quelques années ils sont appliqués au traitement des télangiectasies des membres inférieurs sont plus ou moins associés à la sclérothérapie classique. Ce traitement reste un complément de la sclérose qui reste indispensable, de même que la prise en charge phlébologique classique. Son efficacité intéresse surtout les vaisseaux inaccessibles à l’aiguille de 0,3 mm soit 300 µm de diamètre. Ces vaisseaux constituaient auparavant les foyers de récidive ultérieure. Le KTP 532 nm est particulièrement adapté aux vaisseaux rouges alors que d’autres longueurs d’onde comme le Diode 810 nm voire le Nd :YAG 1064 nm sont plus adaptées aux vaisseaux bleus. Le laser se caractérise en comparaison aux autres méthodes par son caractère sélectif. Semin Cutan Med Surg 2000 Dec;19(4):245-52 The role of lasers in the treatment of leg veins Kauvar AN New developments in laser technology have enabled improved therapy of small and large leg telangiectasia. While sclerotherapy remains the gold standard of treatment, laser therapy should be considered a first line approach for isolated, superficial, fine-caliber, nonarborizing telangiectasia and postsclerotherapy telangiectatic matting. Laser therapy is an excellent option for patients who are fearful of needles or have demonstrated a poor response to sclerotherapy injections. Recent studies have demonstrated good clearance of leg telangiectasia and reticular veins using a variety of laser systems with deeper penetrating, near-infrared wavelengths and higher fluences in conjunction with various epidermal cooling methods. As with sclerotherapy, optimal results are achieved with lasers when larger feeding vessels are treated first using appropriate modalities. Dermatol Surg 2001 Jan;27(1):31-3 Clinical characteristics of 500 consecutive patients presenting for laser removal of lower extremity spider veins Bernstein EF BACKGROUND: Laser treatment for removal of lower extremity spider veins is emerging as a modality of choice in patients with small spider veins, those who have previously undergone sclerotherapy or vein stripping, and those refusing sclerotherapy. OBJECTIVE: To determine clinical characteristics of patients presenting for laser treatment of leg veins. METHODS: The clinical characteristics of 500 patients presenting for laser treatment of spider veins were evaluated to investigate characteristics leading to their development, and to characterize the type of patients presenting for laser treatment. RESULTS: Patients presenting for treatment range widely in age and have had spider veins for an average of 14 years. Both pregnancy and previous sclerotherapy were factors that contributed to the development or exacerbation of spider veins. CONCLUSION: As laser treatment of spider veins improves, this modality will play an increasing role in the management of lower extremity telangiectasias. Dermatol Clin 2001 Jul;19(3):467-73 Treatment of leg veins with lasers and intense pulsed light. Preliminary considerations and a review of present technology Goldman MP Each laser system has different wavelengths, spot sizes, cooling mechanisms, and pulse durations. This article examines the advantages and disadvantages of different lasers with the proposition that, in the end, the best laser is the one that the practitioner can use best. Phlébologie 2001, 54 (4), 405-11 Theorical and technical bases of vascular laser treatment Anastasie B, Célerier A, Blanchemaison Ph Cet article détaille les différentes étapes entre l’irradiation par une lumière laser et la dénaturation tissulaire conduisant à la photo-coagulation du vaisseau cible. D’autres mécanismes peuvent être impliqués comme la photo-thermolyse ou la photo-thrombose. Le commencement est une inversion de population dans la chambre d’activation du laser jusqu’à la dénaturation tissulaire aboutissant à la sclérose du vaisseau. La conversion de la lumière en chaleur implique l’absorption de la lumière par un chromophore comme l’hémoglobine. La manipulation de cet outil exige des connaissances concernant la diffusion optique tissulaire, objet de ce travail. This article details the different stages between laser irradiation and tissular alteration leading to photocoagulation of target vessel. Other mechanisms can be involved as photothermolysis and photothrombosis. The beginning is the inversion of an atomic population in the activation chamber of the laser until the target tissue alteration leading to sclerosis of the vessel. The conversion of light into heat involves absorption by a chromophore as haemoglobin.The manipulation of this tool requires knowledges interesting the field of optic tissular diffusion, subject of this work. J Cosmet Dermatol. 2003 Apr;2(2):73-81 The treatment of leg telangiectasia Neumann HA, Kockaert MA Leg telangiectasia is more difficult to treat than facial telangiectasia. Investigations may be needed to elucidate the origin of the telangiectasia. In cases of venous insufficiency, investigation of venous haemodynamics is desirable. Treatment is primarily by sclerotherapy, including foam sclerotherapy. Light and laser treatments are also effective, especially for telangiectasia up to 1 mm in diameter. New developments incorporate longer pulse durations, such as frequency-doubled neodynium YAG and diode lasers as well as intense pulsed light. After all treatment methods, compression for 48 h using pads, bandages or hosiery is recommended. As with all cosmetic procedures, patients need to be tutored comprehensively about anticipated results and possible complications or side-effects. Ross V, Domankevitz Y Laser leg vein treatment: a brief overview J Cosmet Laser Ther. 2003 Dec; 5(3-4): 192-7 Laser treatment of leg veins has been associated with a number of disadvantages, but the introduction of new devices has increased the role of lasers in the treatment of leg veins. This paper reviews the role of laser devices applied from the surface in the treatment of reticular and spider veins. Success is determined by the proper selection of wavelength, fluence, pulse duration, spot size, and number and frequency of treatments. J Cosmet Laser Ther. 2004 Nov;6(3):152-5 A prototype vessel compressor helps efficient laser treatment of small leg veins Trelles MA, Calderhead RG The eradication of small leg veins with lasers continue to present problems. Visible light lasers (488 nm approximately 595 nm) are well absorbed in haemoglobin but melanin is also a target, necessitating aggressive skin cooling to prevent damage to the epidermis and adding to the expense of these laser systems. A new generation of much less expensive semiconductor-based lasers operating in the near infrared offers a different approach, with protein as the main target rather than pigment. For visible light lasers, compression of the target vessels is a contraindication, since the target pigment is removed. For near IR diode lasers, however, compression of the vessels is a benefit, as the cooling effect of the blood flow is removed and the highly proteinous vessel walls are coapted which encourages efficient coagulative vessel closure. The prototype of a simple vessel compressor is presented, which first compresses vessels and coapts the walls, and then presents the coapted vessels as a target for a laser of an appropriate wavelength. Lasers Surg Med. 2005 Feb;36(2):105-16 Laser treatment of leg veins: Physical mechanisms and theoretical considerations Ross EV, Domankevitz Y BACKGROUND AND OBJECTIVES: A discussion of laser treatment of leg veins is based on a review of the literature, theoretical analysis, and the clinical experiences of the authors. Theoretical computations are discussed within the context of clinical observations. STUDY DESIGN/MATERIALS AND METHODS: A Monte Carlo model is used to examine volumetric heat production, fluence rate, and temperature profiles in blood vessels at 1,064 and 532 nm wavelengths with various beam diameters, vessel diameters, and pulse durations. RESULTS: Clinical observations, Monte Carlo results, and a review of the literature suggest that longer wavelengths and longer pulses durations favor vessel contraction over intraluminal thrombosis. Monte Carlo simulations show that longer wavelengths are more likely to uniformly heat the vessel compared to highly absorbing wavelengths. Methemoglobin production causes deeply penetrating wavelengths to generate more volumetric heat for the same input radiant exposure. CONCLUSIONS: Clinical observations and models support the role of long wavelengths and long pulses in optimal clearance of most leg telangiectasias. Dermatol Surg. 2005 Apr;31(4):388-90 Laser-doppler examination shows high flow in some common telangiectasias of the lower limb Bihari I, Muranyi A, Bihari P BACKGROUND: The accepted pathophysiology of telangiectasias is reflux from superficial or deep veins. There are physical signs and scientific findings that do not fit this theory but support the possibility of arteriovenous (AV) shunt origin. OBJECTIVE: If there is a higher flow in spider veins than in the surrounding skin, it means that AV shunts participate in the circulation of the telangiectasia. On the other hand, slow flow indicates reflux as the etiologic factor. METHOD: Telangiectasias and the surrounding skin of 22 legs of 19 patients were examined with laser-Doppler equipment. RESULTS: The probe over the spider vein found a higher flow value (average 28.2 perfusion units [PU]) than in the surrounding skin (15.6 PU) in 13 limbs, but it was significantly higher only in 5 cases. In 9 limbs, the flow was slower. CONCLUSION: We interpret the higher flow values as a consequence of open AV shunts. This means that AV shunt pathophysiology was present in some of our cases. Semin Cutan Med Surg. 2005 Dec;24(4):184-92 Laser treatment of leg veins Kauvar AN, Khrom T The development of lasers using deeper-penetrating, near-infrared wavelengths with millisecond pulse durations and skin-cooling methods has produced safer and more predictable results for the treatment of leg veins less than 1 mm in diameter and depth. Recent prospective studies of the near-infrared lasers show comparable efficacy and side effect profiles to those observed with sclerotherapy. Treatment of reticular and varicose veins is effective with these wavelengths but is limited by patient discomfort when compared with sclerotherapy. Visible light lasers (such as the pulsed dye and KTP) and intense pulsed-light sources are reproducibly effective only for superficial, nonarborizing pink-to-red telangiectasia, in the absence of points of proximal reflux. Because most lower-extremity vascular ectasias comprise a heterogeneous group of vessel sizes and depths, many patients achieve the best results using a combination of techniques. This article reviews the fundamentals of laser tissue interactions for the treatment of leg veins and details the recent clinical experience with the newer near-infrared devices. Hautarzt. 2006 May 3; [Epub ahead of print] Laser therapy for vascular lesions Greve B, Raulin C The use of lasers to treat vascular lesions began in the late 1960s with the introduction of argon laser. More recently pulsed laser and intense pulsed light techniques have further improved results and reduced side effects. Their function is based on the principle of selective photothermolysis. Simultaneous application of cooling methods (contact cooling, cold air, cryogen spray) has become standard procedure for these types of therapy, whose most important indications are port-wine stain, hemangioma, and telangiectasia. A persistent difficulty is their limited penetration, resulting in limited or no effect on deeper dermal layers. New approaches therefore include combinations with bipolar radio frequency or the use of two different laser systems, e.g., dye and Nd:YAG lasers. The different lasers are described along with their effectivity, limitations and indications. Clin Dermatol. 2007 Sep-Oct;25(5):454-61 Laser therapy for leg veins Kunishige JH, Goldberg LH, Friedman PM Visible veins on the leg are a common cosmetic concern affecting approximately 80% of women in the United States (Engel A, Johnson MI, Haynes SG. Health effects of sunlight exposure in the United States: results from the first national health and nutrition examination survey, 1971-1974. Arch Dermatol 1988;124:72-9). Without a quick and noninvasive treatment available, leg veins present a therapeutic challenge. This challenge has been tackled by the design of lasers with longer pulse durations, and the use of lasers with longer wavelengths and cooling devices. Recent studies show the efficacy of laser treatment beginning to approach that of sclerotherapy, the gold standard. This review outlines the principles guiding laser treatment, the current available options, and a clinically oriented approach to treating leg veins. Perspect Vasc Surg Endovasc Ther. 2008 Dec;20(4):358-66. Epub 2008 Nov 21 Comment in: Perspect Vasc Surg Endovasc Ther. 2008 Dec;20(4):367-8 Perspect Vasc Surg Endovasc Ther. 2008 Dec;20(4):369-70 Laser ablation of cutaneous leg veins Almeida JI, Raines JK. Patients presenting with lower-extremity telangiectasias, commonly known as spider veins, are a frequent presentation for vascular surgeons. The use of lasers in the treatment of lower-extremity spider veins has gained increased popularity during the past 5 years. This technology, driven by consumer demand, has been effective in treating vessels that are refractory to sclerotherapy treatment, vessels that arise from telangiectatic matting, and in patients who experience a phobia to needles. One laser wavelength per machine limits what the practitioner can do. That is, each type of vein responds best to a specific wavelength. Light skin is more forgiving to complications than dark skin. The devices are a complement to good sclerotherapy, not a substitute. 532 nm Lasers Surg Med 1988;8(2):130-4 532-nanometer green laser beam treatment of superficial varicosities of the lower extremities Smith T, Apfelberg DB, Maser MR, Lash H, White DN Green laser light at 532 nm was utilized in an attempt to thrombose and blanch superficial varicosities of the lower extremity in 14 patients. Selective vascular damage with sparing of overlying skin was the theoretical rationale for use of green light. Seven of the 14 patients achieved satisfactory results (total or near-total obliteration of vessels without scarring) after a 6-month period of observation. Dermatol Surg 1998 Jan;24(1):71-4 Long pulse 532-nm laser treatment of facial telangiectasia Adrian RM, Tanghetti EA BACKGROUND: Facial telangiectasias are a frequently observed cosmetic concern: Current therapeutic modalities have certain side effects and limitations. We treated a group of patients with facial telangiectasias with a new variable pulse width frequency-doubled neodymium: YAG laser at 532 nm. OBJECTIVE: This study evaluated the clinical response and side effects during the treatment of facial telangiectasias in 40 patients. METHODS: Forty patients with facial telangiectasias were treated with the VersaPulse laser. Fluences of between 9.5 and 12.0 J/cm2 at 3 or 4-mm spot size were used. A sapphire water-cooled chill tip was used to cool the cutaneous surface during treatment. RESULTS: Ninety percent of patients experienced between 75% and 100% clearance of their facial telangiectasias after single treatment. No significant side effects or complications were noted. CONCLUSION: The VersaPulse variable pulse width neodymium: YAG laser appears to be an effective treatment modality for facial telangiectasia. Dermatol Surg 1998 Jan;24(1):19-23 Treatment of leg telangiectasias using a long-pulse frequency-doubled neodymium:YAG laser at 532 nm. Adrian RM BACKGROUND: At the present time a large variety of vascular lesion lasers are available for the treatment of both congenital and acquired disorders of blood vessels. Although most vascular lesions lasers are variably effective in the treatment of facial telangiectasias, port-wine stains, hemangiomas, and other vascular anomalies, their use in the treatment of leg veins has been disappointing. Histologic, anatomic, and other variables have been associated with a poor response of leg veins to currently available vascular lesion lasers. OBJECTIVE: This study examines the use of a new long pulse frequency-doubled Neodymium (Nd):YAG laser emitting radiation at 532 nm for the treatment of leg veins. METHODS: Fifty patients with leg telangiectasias of varying diameters were treated using a variable pulse width frequency doubled Nd:YAG laser. This laser delivers energy through a novel water-cooled chill tip, which appears to limit epidermal damage during laser treatment. RESULTS: Sixty-two treatment sites were evaluated in 50 patients. Seventy-three percent of patients had greater than 50% improvement after one treatment. Eight-three percent were graded with clearances of better than 50% after two treatments, with 63% showing greater than 75% improvement. CONCLUSION: The VersaPulse variable pulse width laser appears to be an effective modality for the treatment of leg telangiectasias. The relative lack of patient discomfort combined with a high degree of patient satisfaction may indicate a fairly high level of patient acceptance of this new form of therapy for the treatment of leg telangiectasias. Dermatol Surg 1998 Feb;24(2):221-6 Comparison of the long-pulse dye (590-595 nm) and KTP (532 nm) lasers in the treatment of facial and leg telangiectasias West TB, Alster TS BACKGROUND: Telangiectasias develop on the face secondary to genetic predisposition, chronic actinic damage, collagen vascular disease, topical steroid application, and disorders of vascular regulation including acne rosacea. Linear and "spider" telangiectasias develop on the legs, especially in women beginning in the second to third decade, secondary to multiple factors including genetic predisposition, gravity, pregnancy, and trauma. OBJECTIVE: The purpose of this investigation was to compare the 590- and 595-nm long-pulse (1.5 msec) dye laser and KTP (532 nm) laser in the treatment of facial and leg telangiectasias. RESULTS: For both facial and lower extremity telangiectasias, the difference in improvement ratings between the two lasers following both one and two treatment sessions was statistically significant. CONCLUSION: Both the flashlamp-pumped long-pulse dye laser and the KTP laser may play a role in the treatment of facial and leg telangiectasias. However, when used to treat vessels on the lower extremities, both of these laser systems are probably best used in conjunction with sclerotherapy of the larger "feeding" reticular veins. While long-pulse dye laser irradiation achieves superior vessel clearance, patients may prefer multiple treatments with the KTP laser due to its low side effect profile and decreased associated pain. Hautarzt 1999 Mar;50(3):181-5 Long-pulsed frequency-doubled neodymium:YAG laser in treatment of superficial varicose veins. Initial clinical experiences Bethge S, Stadler R Many different therapeutic approaches are employed to treat small vessels on the leg. In recent years a variety of lasers (argon, Neodymium: YAG and dye lasers) have been used as well as sclerotherapy, cryosurgery and electrosurgery. None of these lasers are entirely satisfactory, and there are a number of side effects. Because of its special physical characteristics, the newly developed long-pulsed frequency-doubled neodymium: YAG laser has clear advantages in the treatment of vascular lesions compared to other laser systems. These include: no vessel rupture compared to dye laser, no epidermal lesions compared to argon laser. In clinical tests it shows a high rate of effectiveness with minimal side effects. Dermatol Surg 1999 Sep;25(9):677-80 Comment in: Dermatol Surg. 2000 Feb;26(2):169-70, Dermatol Surg. 2000 Jan;26(1):92-3. Successful treatment of spider leg veins with a high-energy, long-pulse, frequency-doubled neodymium:YAG laser (HELP-G) Massey RA, Katz BE BACKGROUND: While sclerotherapy has been the standard treatment for spider leg veins for many years, recent advances have allowed lasers to be considered as a treatment option. OBJECTIVE: To study the efficacy of a frequency-doubled Nd:YAG laser at 532 nm with a 50 ms pulse width and chill tip device in the treatment of spider leg veins. METHODS: Forty-six patients with spider leg veins with a diameter of less than 1 mm or 1-2 mm were treated with a frequency-doubled Nd:YAG laser at 532 nm with a pulse width of 50 ms (VersaPulse HELP-G laser) while using a water-cooled chill tip device. RESULTS: Of patients with veins less than 1 mm in diameter, 60% had greater than 50% clearing after one treatment and 80% had greater than 50% clearing after two treatments. Of patients with veins 1-2 mm in diameter, 39% achieved greater than 50% clearing after one treatment and 67% had greater than 50% clearing after two sessions. CONCLUSION: Our results suggest that the frequency-doubled Nd:YAG laser with a pulse width of 50 ms and chill tip device offers an excellent alternative to sclerotherapy in the treatment of small spider leg veins. J Cutan Laser Ther 1999 Sep;1(3):179-80 Treatment of spider veins of the leg using a long-pulsed Nd:YAG laser (Versapulse) at 532 nm McMeekin TO BACKGROUND AND OBJECTIVE: Prior studies have shown improvement in leg telangiectasias using a long pulse, frequency-doubled nd:YAG laser at 532 nm. The following study, with longer follow-up, was undertaken to determine the effectiveness of this laser and incidence of side-effects from a single treatment for lower extremity telangiectasia of less than 1 mm in diameter. MATERIALS AND METHODS: Ten patients of skin types I-III received a single treatment on each of 18 treatment sites. One to three passes were used on each vessel with a repetition rate of 2 Hz. Two energy fluences of 12 J/cm2 and 16 J/cm2 were compared. Patients were followed for 1 year with follow-up photographs taken, from which the percentage of vessel clearance and side-effects were rated. RESULTS: Overall, 44% of patients had a greater than 50% clearance from a single treatment using the frequency-doubled Nd:YAG laser at 532 nm. The higher fluence of 16 J/cm2 showed a better response than the lower fluence of 12 J/cm2. Side-effects were more marked and were seen in more patients treated at 16 J/cm2 than at the 12 J/cm2 setting. Some 94% of patients had hyperpigmentation that took up to 6 months to resolve. One patient treated at 16 J/cm2 experienced blisters, crusts and scarring, which persisted for 1 year. There was further improvement from 6 months to 1 year in one-third of the treatment sites. CONCLUSION: The long-pulsed Nd:YAG laser at 532 nm with a chilled sapphire tip can treat leg telangiectasias of 0.5 to 1.0 mm in diameter with greater than 50% clearance at 44% of sites with a single treatment. Higher fluences of 16 J/cm2 demonstrated a greater clearance, but also greater adverse effects, including atrophic scarring persisting for 1 year. Further clinical improvement was seen at 6-month to 1-year follow-ups. Dermatol Surg 1999 Apr;25(4):316-20 Treatment of spider veins using a 10 millisecond pulse-duration frequency-doubled neodymium YAG laser Bernstein EF, Kornbluth S, Brown DB, Black J BACKGROUND: The pulsed dye laser has been the standard for treating vascular lesions. Although quite effective for treating facial vessels and port-wine stains, spider veins of the lower extremities are more difficult to treat. Recent studies have shown that lasers with longer pulse durations are more effective at treating spider veins. A new long-pulse frequency-doubled Neodymium:YAG laser has been developed with a 10-ms pulse duration and sufficient energy to enable treatment with a 3- or 4-mm diameter treatment beam. OBJECTIVE: To determine the effectiveness of the long pulse Neodymium:YAG laser for treating spider veins of the lower extremities. METHODS: Spider veins less than 0.75 mm in diameter on the legs of 15 female volunteers were treated in 1 or 2 areas. Treatments were administered through a water-cooled chill tip using the frequency-doubled Neodymium:YAG laser with a 10-ms pulse duration. A dose of 16 J/cm2 was administered, completing 3 passes over each visible vein during each session, for a total of 2 sessions administered 6 weeks apart. Photographs of treatment areas were digitally analyzed for degree of vessel clearance. RESULTS: Computer-based image analysis revealed clearing of over 75% of veins following 2 treatments with 16 J/cm2. Side effects were minimal, and the treatments were well tolerated. CONCLUSIONS: The 532 nm, 10 ms pulse duration, frequency-doubled Neodymium:YAG laser is safe and effective for treating spider veins of the lower extremities less than 0.75 mm in diameter, in patients with Fitzpatrick skin Types I-III. Cutan Laser Ther 2000 Sep;2(3):141-6 Treatment of facial telangiectasias with a diode-pumped Nd:YAG laser at 532 nm Cassuto DA, Ancona DM, Emanuelli G OBJECTIVE: Facial telangiectasias are a common cause of cosmetic concern. Current treatment modalities present various untoward effects and limits. The pulsed dye laser has been considered the gold standard in efficacy and safety; unfortunately it causes postoperative intracutaneous hematomata, discouraging many patients from undergoing this treatment. Several other vascular lasers (argon, tunable dye, copper, krypton, etc.) are disadvantaged by the risk of hypopigmented and atrophic scars. MATERIALS AND METHODS: We assessed a recent powerful version of the potassium titanyl phosphate (KTP) 532 nm laser, which delivers sufficient energy in single pulse lasting 10-50 msec (DioLite 532; IRIDEX, Mountain View, CA, USA). Collateral damage is reduced while the heating of the vessel is slow enough to avoid explosive photothermolysis with its associated purpura. Sixty six patients with facial telangiectasias were treated. RESULTS: In 62/66 patients (93.9%) we achieved a 75-100% clearance of the lesions, while two treatments were needed to reach an acceptable clearance in the remaining 4/66 patients (6.1%). The eventual need for more sessions was well tolerated because the acceptable postoperative appearance allowed patients to continue normal business and social activities between treatments. No permanent complications or undesired effects were noted. CONCLUSION: We conclude that this diode-pumped frequency-doubled Nd:YAG laser is an effective device for the treatment of facial telangiectasias, with a low profile of undesired effects that can be well tolerated by patients. 14 Th World Congress of International Union of Phlebology, Rome 9-14 Sept 2001, Abstract P 240 Treatment of leg telangiectasias using a 532 nm green laser system R.Lonardi, R.Marra, G. Zorzan, M.Gargiulo, V.Melita, A.Rumolo Leg telangiectasias are a very important cosmetic problem for a high percentage of the female population. Sclerotherapy is the treatment most widely used today, but there are some situations when this option isn't the most suitable method, like telangiectatic matting. Objective: This study evaluates the effectiveness and safety of a green laser system (532 nm) on leg telangiectasias equal or less than 1 mm in diameter. Material and Methods: 87 female patients, Fitzpatrick skin type I - III, mean age 41 years, were treated for leg telangiectasias less than or equal to 1 mm in diameter, alter surgical therapy and/or complementary sclerotherapy of larger tributary veins. Energy fluence varies from 10 to 23 J/cm2, with a pulse duration from 8 to 50 ms and a spot size of 600 nm and 1500-2000 nm according to the vessel diameter. Only one pass was used on each telangiectasia. All patients were photographed before and alter each session and during follow-up at 1 month, 6 months and 1 year. Every treatment site needed 1 to 4 sessions according to the extension of the area involved. A contact cooling system was always used. Results: At the end of the treatment good results were observed in 83 patients (95,4% ; 70-100 clearance), while 4 patients (4,6%) showed fair vessel clearance (30-70 %). Multiple adverse reactions were noted in 63 patients (72,4%) but no patients had hypoor hyper-pigmentation alter 6 months. Conclusions - The Green Laser System (532 nm) has shown its efficiency in treating lower limb telangiectasias equal or less than 1 mm in diameter. 14 Th World Congress of International Union of Phlebology, Rome 9-14 Sept 2001, Abstract P 241 Does Laser Treatment for Leg Teleangiectasia works? Raskin,Boris,Scuderi ,Angelo,Raskin Reis,Fany Unitherms: Mating treatment;Laser and Varices treatment Introduction: The reason of this paper was to find out the limits of leg telangiectasia treatment with laser 532 and its effectiveness. lt is well established that Laser Treatment of Facial telangiectasia has good results . Methods: 300 patients clinically diagnosticated having primary teleangiectasia were treated with laser only, in 1 session, age between 15 and 70 years. Laser fluence varying from 16 to 28 joules ,3 watts power ,4 hertz repetition rate, handpiece Of 700 micron. Digital photografy were taken 1 week and 1 month before and after laser therapy. Results: Better statistic results of 65 °%o regarding on occlusion of capillaries (empty capillary circulation test) in 1 single session of 15 minutes. Pain , skin temporary hyper or hypopigmentation were the main complication events. Conclusion: Physical laser treatment works well in leg Telangiectasia in the great majority Of patients (60 %). He is the only method of treatment and prevention of matting or neovascular formation after chemical scleroterapy. To achieve better results it is necessary to associate with others methods (chemical,capillaries drainage). 14 Th World Congress of International Union of Phlebology, Rome 9-14 Sept 2001, Abstract P 335 Sclerotherapy of red leg telangectasia compared with association of sclerosis and laser therapy (532 nm) B Anastasie We submit the results of a study regarding more than 50 patients to compare sclerosis of red leg telangectasia versus sclerosis combined with a 532 nm laser treatment alter three processings. We also set out our method to assess our data using transparent tracing paper. We report our clinical experience with other 1,500 patients since three years: side-effects, clinical results, treatment processing. It is clearly possible to treat patients on three sessions with an interval of one month. Compared to classical sclerotherapy, this combination allows dividing the number of sessions by two, better esthetics results obtained with prolonged efficiency. We explain this phenomenon by the specificity of the wavelength (532 nm) on the target tissue compared with others thermical methods, by the synergy of chemical and specific thermical sclerosis of the small veins (<500 µm) and the treatment of telangiectasias less than 300 µm which is the smallest caliber of needle (30G); these little telangectasias are the origin of recidivation. The combination of treatment with laser and classical sclerotherapy is more efficient than sclerotherapy alone witch is still essential. Lasers Surg Med. 2002;31(3):194-201 Treatment of spider leg veins with the KTP (532 nm) laser--a prospective study Spendel S, Prandl EC, Schintler MV, Siegl A, Wittgruber G, Hellbom B, Rappl T, Berghold A, Scharnagl E BACKGROUND AND OBJECTIVES: Spider leg veins are telangiectasias located intracutaneously. This condition poses a cosmetic problem. STUDY DESIGN/PATIENTS AND METHODS: The purpose of this study was to determine what influence the KTP (532 nm) laser has on spider leg veins dependent on the vascular diameter and to what extent the skin has been affected. Seventy female patients were treated in three laser sessions. Analysis was done 30 weeks after the last laser treatment session. RESULTS: Fifty-six patients completed the study. In group 1 (vascular diameter < or = 0.6 mm), spider leg veins were no longer visible in 33%; in 40%, a decrease in vascular diameter could be observed; in 27%, no change in size occurred. In group 2 (vascular diameter 0.7-1.0 mm), laser-treated spider leg veins were visible in all patients. Hyperpigmentation occurred in 13 patients. CONCLUSIONS: The KTP (532 nm) laser is an effective for treating spider leg veins having a vascular diameter under 0.7 mm. Dermatol Surg. 2002 Jul;28(7):564-71 Treatment of leg telangiectases with a 532 nm KTP laser in multipulse mode Fournier N, Brisot D, Mordon S BACKGROUND: The multiple mode emission emphasizes the efficacy of the KTP laser. OBJECTIVE: To evaluate the efficacy of a 532 nm KTP laser emitting in multipulse mode for the treatment of superficial 0.5-1 mm leg telangiectases. METHODS: A 532 nm KTP laser was used in a nonuniform pulse sequence or multipulse mode emission (three stacked pulses of 100 msec, 30 msec, 30 msec, and a delay between pulses of 250 msec), a fluence of 60 J/cm2, and a 0.75 mm collimated spot. No cooling was used. Fourteen female patients (average age 46 years, range 27-57 years), phototypes I-IV were examined with Doppler ultrasound to ensure their big veins were competent. A topography of the telangiectatic network was reported on a tracing plastic frame before each session and 6 weeks after the last one. These frames were digitized and the number of vessels (before and 6 weeks after each session) was determined using imaging software. Side effects, pain, and patient satisfaction were noted. RESULTS: Moderate pain, immediate erythema and edema, sometimes light scabbing, temporary hypopigmentation rarely, and no matting were observed. After one treatment, vessel clearing was 53% (P <.001). It increased to 78% (P <.001) 6 weeks after two treatments, to 85% (P <.05) 6 weeks after three treatments, and to 93% (NS) 6 weeks after four treatments. CONCLUSION: This nonuniform pulse sequence or multipulse mode emission emphasizes the efficacy of the KTP laser in this study. It provides a safe and effective treatment that achieved an important reduction of red leg veins telangiectases from 0.5 to 1 mm in diameter, with very few side effects. Angéiologie, 2003, 55 (1): 37-46 Sclérose des varicosités versus sclérose associée au laser 532 nm. Etude des effets indésirables Anastasie B L’objectif de ce travail était d’attester l’efficacité de la sclérose et du laser 532 nm associés sur un même temps de traitement, comparativement à la sclérose seule. Ces travaux ont permis d’évaluer la reproductibilité de la méthode utilisant des calques transparents. Quarante patientes ont été incluses en choisissant des sites divisés en deux après un repérage anatomique précis sur un calque transparent. Une partie était simplement sclérosée (aoetoxysclérol ® 0,5 % dilué au G 30 %), l’autre partie subissait en sus un traitement par laser 532 nm avec une fluence (16 J / cm²), une durée de pulse (10 ms) et un diamètre de spot (2 mm) constants. Le critère d’efficacité retenu était le pourcentage de raccourcissement des vaisseaux repérés. Leur diamètre était mesuré de 0,1 à 1 mm. La transillumination était systématiquement associée à la sclérose pour éviter des biais liés à des reflux ignorés qui sous-estiment l’efficacité du traitement. Deux séances à un mois d’intervalle étaient pratiquées avec une prise de nouveau calque au troisième mois. Les résultats montrent un pourcentage de réduction de longueur des vaisseaux (R) égal à 78,95 % (P < 0,00001) lorsque les deux traitements sont associés, versus 47,35 % pour la sclérose seule. Les résultats sont meilleurs sur les faces externes de cuisse (24 patientes, R = 84,12 %) que sur les autres sites confondus (16 patientes, R = 70,68 %). Il n’y a pas de différence significative avec ou sans traitement hormonal (14 patientes, R = 78 % - 26 patientes, R = 79,46 %) ou si l’index de masse corporelle est supérieur à 25 (13 patientes, R = 76,46 %) ou inférieur à 25 (27 patientes, R = 80,14 %). Nous publions nos résultats d’une seconde étude concernant les effets indésirables sur une population de 216 patients, et la possibilité pratiquer les deux types de traitements sur la même séance, sur les mêmes vaisseaux . Nous relatons notre méthodologie après 2000 patients traités depuis 1997. Mots-clés: laser, 532 nm, varicosités, télangiectasies The aim of this study was to testify the efficacy of sclerosis and laser 532 nm associated in the same session of treatment comparatively with the sclerosis alone. These works allows to value the reproductiveness of the method using transparent tracing papers. Forty patients have been included while we have selected sites divided in two parts after precise anatomic marking on these transparent tracing papers. One part was treated with sclerosis alone (aoetoxysclérol ® 0,5 % diluted with glucosed 30 %), on the over one was added laser 532 nm with constant value of fluence (16 J/cm²), pulse duration (10 ms) and spot diameter (2 mm). The efficacy criterion was the shortening percentage of the located vessels. Their diameter was measured between 0,1 to 1 mm. Transillumination was systematically associated with sclerosis to avoid mistakes dued to ignored reflux which under-estimate the treatment efficacy. Two sessions with one month of interval were carried out with new transparent process at the third month. Results showed a percentage of vessels shortening (R) equal to 78,95 % (P < 0,00001) while the two treatments were associated compared with sclerosis alone (47,35 %). Results are better on the external side of the thigh (24 patients, R = 84,12 %) compared with other anatomic sites (16 patients, R = 70, 68 %). There is no significant difference with or without hormonotherapy (14 patients, R = 78 – 26 patients, R = 79,46 %) or if the corporeal mass index was upper than 25 (13 patients, R = 76,46) or lower than 25 (27 patients, R = 80,14 %). We publish our results of a second study concerning side effects on a population of 216 patients where we demonstrate that it is possible to practice the two treatments on the same session, on the same vessels. We relate our methodology after 2000 patients treated since 1997. Rozhl Chir. 2003 Jul;82(7):371-5 Personal experience with laser photocoagulation of varicose veins Foldyna A, Lajmar K, Matousek P Based on the published information on the use of operation lasers for endoluminal photocoagulation to seal varices the authors began to use KTP laser in 2001. The cohort included 200 patients operated on in 2002. The cohort was composed of three groups of patients: patients with reticular varices, those with non-saphenous varices and patients with the stem saphenous varices. The intervention was made by a KTP laser, wavelength 532 nm, light-conducting wires of 0.2, 0.3 or 0.6 mm diameter. Dermatol Surg. 2003 Dec;29(12):1176-80; discussion 1180 532-nm Nd:YAG and 595-nm pulsed dye laser treatment of leg telangiectasia using ultralong pulse duration Woo WK, Jasim ZF, Handley JM BACKGROUND: Telangiectatic leg veins have been treated using lasers with variable success. OBJECTIVE: We aimed to examine the efficacy and tolerability of a 595-nm pulsed dye laser (PDL) and a 532-nm Nd:YAG laser using ultralong pulse duration to improve leg telangiectasias with a single treatment. METHODS: Ten subjects with leg telangiectasias up to 1.0 mm in diameter participated in the study. The telangiectatic patch was divided into two approximately equal adjacent areas. The first area was treated with a 532-nm Nd:YAG laser at a fluence of 20 J/cm2 and a pulse duration of 50 ms using a contact cooling device. The second area was treated with a 595-nm PDL at a fluence of 25 J/cm2 and a pulse duration of 40 ms using cryogen spray precooling. Each area was treated once only. Photographic evaluation was used for an assessment of response. RESULTS: Two of 10 subjects had less than 25%, 3 had 25% to 50%, 2 had 50% to 75%, and 3 had more than 75% improvement after single treatment with a 532-nm Nd:YAG laser. Similarly, 2 of 10 subjects had less than 25%, 2 had 25% to 50%, and 6 had 50% to 75% improvement with the 595-nm PDL. Hyperpigmentation occurred in one subject treated with the 532-nm Nd:YAG laser and two subjects treated with the 595-nm PDL. No blistering, crusting, hypopigmentation, or scarring were observed. CONCLUSION: Both lasers using ultralong pulse width improved leg telangiectasias after a single treatment with minimal adverse reactions. Lasers Surg Med. 2004;35(1):68-76 Long pulse Nd:YAG laser for treatment of leg veins in 40 patients with assessments at 6 and 12 months Trelles MA, Allones I, Martin-Vazquez MJ, Trelles O, Velez M, Mordon S BACKGROUND AND OBJECTIVES: This study assessed subjectively and objectively the efficacy of a long-pulsed Nd:YAG laser system in clearing dermal leg veins, successful treatment of which remains problematic. STUDY DESIGN/PATIENTS AND METHODS: Forty female patients (24-58 years old, skin types II-IV) with leg veins were treated with synchronized micropulses from a long-pulsed 1,064 nm Nd:YAG laser, 6 mm diameter spot size, 130 and 140 J/cm2. One to three treatments were given at 6-week intervals, with post-treatment assessments at 6 and 12 months. Patients assessed improvement subjectively with a satisfaction index (SI). Objective assessment was based on the clinical photography, and in addition on computer-generated data from a Canny operator-based edge-detection program. RESULTS: The overall patient satisfaction rates and objective assessments at the 6 and 12 month assessments were 42.5 and 57.5%, and 75 and 82.5%, respectively. CONCLUSIONS: The long-pulsed Nd:YAG laser offered efficient treatment of leg veins. Side effects were minimal and transient. The edge-detection program may help patients appreciate better the actual results of the treatment. 578 nm Dermatol Surg 2002 Jan;28(1):21-5 The utilization of a new yellow light laser (578 nm) for the treatment of class I red telangiectasia of the lower extremities Sadick NS, Weiss R BACKGROUND: A dual-wavelength approach is necessary in order to achieve consistent results when utilizing lasers and intense pulsed light sources to treat red and blue lower extremity vessels. In this regard, short-wavelength technologies (500-800 nm) may be employed to treat red telangiectasia of less than 2 mm on the lower extremities. OBJECTIVE: To demonstrate a new yellow light laser utilizing a copper bromide medium and its potential efficacy in the treatment of red lower extremity telangiectasia of less than 2 mm. METHODS: Forty-six women (mean age 37 years) were treated in two private practice settings with a 578 nm yellow light laser with a circulating cooling window (1-4 degrees C). Class I red telangiectases of the thighs 1.5 mm or less in diameter were considered for treatment. Patients were treated with up to three treatments at 6-week intervals on a 5 cm2 surgical area of vessels utilizing a fluence of 50-55 J/cm2. Results were analyzed by macrophotographic imaging, double-blinded observer evaluation/optical chromatography, and a patient evaluation scale. RESULTS: An average of 1.7 patient treatment sessions produced significant clearing of 75-100% in 71.8% of patients. The mean erythema index showed significant lightening (51-65a+) in the study population. Finally, 76.1% of patients reported great satisfaction with the results of their treatment session. CONCLUSION: A new 578 nm copper bromide (CuBr) yellow light laser produces excellent results in eradicating red telangiectases of the lower extremities that are less than 2 mm in diameter. LAMPES FLASH Dermatol Surg 1996 Apr;22(4):323-30 Comment in : Dermatol Surg. 1997 Apr;23(4):303-5. Photothermal sclerosis of leg veins. ESC Medical Systems, LTD Photoderm VL Cooperative Study Group Goldman MP, Eckhouse S BACKGROUND. The flashlamp-pumped pulse dye laser at 585 nm has previously been reported to be somewhat effective in treating leg telangiectasia with diameters less than 0.2 mm. A pulsed photothermal devise (intense pulsed light source [IPLS]) has been developed to treat leg veins ranging in size from 0.1 to 3 mm in diameter. Vessel necrosis occurs from an intense pulsed light that penetrates through the skin and is absorbed by the blood vessels based on the principle of selective photothermolysis. OBJECTIVE. To determine the effectiveness of this novel device on treating leg veins. METHODS. One hundred fifty-nine patients with 369 lesions were treated with the IPLS in a multicenter trial. RESULTS. Clearance of 75-100% was achieved in 79% of treated lesions. Better than 50% clearance was achieved in 94% of completed cases. A very low rate of adverse effects occurred. CONCLUSION. The IPLS is a safe and effective modality to treat leg veins ranging in size from 0.1 to 3 mm in diameter. Hautarzt 1996 Apr;47(4):258-63 Selective photothermolysis of superficial varicose veins telangiectasias of the lower extremity Wiek K, Vanscheidt W, Ishkhanian S, Weyl A, Schopf E Leg venectasia is a common problem. Although there are a variety of therapeutic modalities, none of them gives satisfactory results. The effects of sclerotherapy in the treatment of telangiectasia with a small diameter are poor. Electrocoagulation and argon laser treatment often result in scarring. We studied the effectiveness of the flashlamp pumped pulsed dye laser at a wavelength of 585 nm in the treatment of leg venectasia. After repeated treatments using this laser system, only 30% of the vessels that looked blue on clinical examination could be removed; we obtained better lightening of smaller red, telangiectatic vessels with a diameter up to 0.4 mm. However, hyperpigmentation frequently developed after treatment. In post-treatment biopsies, occlusion of the vessels was found. Based on these results, we recommend a combined therapy for leg venectasia. Larger diameter vessels should be treated with sclerotherapy, while finer telangiectasia can be treated with the flashlamp pumped pulsed dye laser. Lasers Surg Med 1997;21(5):413-6 Progressive ascending telangiectasia treated with the 585 nm flashlamppumped pulsed dye laser Perez B, Nunez M, Boixeda P, Harto A, Ledo A BACKGROUND AND OBJECTIVE: Progressive ascending telangiectasia (PAT) is a distinct entity with telangiectatic superficial vessels on lower extremities as its main clinical feature. A relationship with occult infections and response to antibiotic and antifungal drugs have been described, although not all cases can be successfully managed with these therapies. Our objective was to treat a woman with PAT that had failed to respond to systemic antibiotic and antifungal drugs. STUDY DESIGN/PATIENTS AND METHODS: A 44-year-old woman with PAT was treated with the flashlamp-pumped pulsed dye laser at 585 nm, with fluences varying from 7 to 7.25 J/cm2. RESULTS: A successful outcome was obtained with this treatment approach, with no relevant adverse effects except for mild pigmentary changes. CONCLUSIONS: Although ectatic vessels on lower extremities are often resistant to dye laser therapy, superficial thin capillaries like those featuring PAT can be eliminated with the pulsed dye laser at 585 nm. Transient pigmentary changes occur on treated areas but they are expected to disappear in 6 to 12 months after treatment. Laser treatment should be considered in PAT despite the extension and location of the lesions. Dermatol Surg 1997 Oct;23(10):941-5; discussion 945-6 Comment in: Dermatol Surg. 1997 Dec;23(12):1221. Treatment of essential telangiectasias with an intense pulsed light source (PhotoDerm VL) Raulin C, Weiss RA, Schonermark MP BACKGROUND: The flashlamp-pumped pulsed dye laser (585 and 577 nm) has proven to be a very effective and safe treatment option in the therapy of essential telangiectasias (ETE). Nevertheless, the postoperative intracutaneous hematomata, which most patients see as cosmetically disfiguring, always has been a matter of concern. OBJECTIVE: To test the efficacy and safety of a new, large spot size, intense pulsed light source, the PhotoDerm VL, which omits noncoherent light adjustable within the 515-1200-nm range, in the treatment of ETE. METHODS: Fourteen patients were treated with the PhotoDerm VL. They suffered from ETE of the face, postoperative teleangiectasis of the nose, ETE of both legs, and poikiloderma of Civatte. RESULTS: All treated lesions could be abrogated with excellent results by this new device. There were no unpleasant side effects of the treatment. Additionally, due to the large spot size (2.8 cm2), a larger area could be treated within one session. No anesthesia was required. CONCLUSION: The PhotoDerm VL is an innovative, highly effective, and comparably safe therapeutic alternative to the laser in the treatment of ETE. The rate of cosmetically relevant side effects is considerably smaller, the patient compliance is excellent, and the method can be applied easily in an outpatient setting. Hautarzt 1998 Jul;49(7):560-5 Treatment of superficial varicosities with a flashlamp-pumped pulsed dye laser with 1.5 ms impulse time Hohenleutner U, Wenig M, Walther T, Baumler W, Landthaler M A new flashlamp-pumped pulsed dye laser with 1.5 ms pulse length and tunable wavelengths between 585 and 600 nm (Candela ScleroPLUS) is now available for the treatment of ectatic leg veins. We evaluated 232 single test treatments using 595 and 600 nm wavelength in 75 test persons. For smaller vessels up to a diameter of 0.5 mm, treatments at 16 and 18 J/cm2 showed good results in 60 and 82% respectively; for vessels up to 1 mm in 27 and 33%. Treatment at 595 nm was a little more effective than at 600 nm. Larger vessels could not be treated effectively. The main side effects consisted in hyper-(34%) or hypopigmentation (30%). Thus, in addition to the usual sclerotherapy, this laser is a useful device for the treatment of leg vein ectasia. Dermatol Surg 2001 Jun;27(6):549-54 Skin temperature measurements during intense pulsed light emission. Miyake RK, Miyake H, Kauffman P BACKGROUND: Although lasers and intense pulsed light sources have improved the capability of injuring veins without affecting the overlying skin, work is needed to improve the procedure. OBJECTIVE: To create a method for predicting skin reaction to pulsed light. METHODS: Twenty patients were divided into four groups according to skin type (I-IV). An industrial thermometer equipped with a laser-aiming system was adapted to the intense pulsed light source handpiece. Patients received shots of increasing intensity while the skin temperature was measured. RESULTS: Fluence and temperature data were analyzed by logistic regression to evaluate possible injury. The stepwise method selected skin type and temperature variation as predictors of skin injury. Logistic curves indicated the maximum temperature variation tolerable for each skin type. More pigmented skin types tolerated less temperature increase. CONCLUSION: Skin type can predict cutaneous reaction to intense pulsed light through measurements of temperature variation. This method may help achieve successful selective photothermolysis. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 335 Laser treatment of facial telangiectasias Hilario Robledo , Phd, FACS The patients with facial telangiectasias look for some type of treatment, fundamentally based on a cosmetic attitude, therefore it is important that the used method is relatively free of risks and without undesirable resulting scars. They have been used for many years different types of treatments in the history of facial telangiectasias like electrosurgery and sclerotherapy, but first. due to the possibility and frequency whereupon these methods can produce undesirable effects, and second, to the development of new technologies like the different types from lasers and intense pulsed light-IPL and specially within of IPL system, the phenomenon of fluorescence. for the elimination of this problem chat can affect to the 10-15 % of the population. Nowadays we think chat the methods previously mentioned have been obsolete and they would not have to be made. Also the use of the lasers would have to be practiced by surgeons specially trained in this type of treatments and with an exhaustive knowledge of the anatomical, pathological concepts and a specialized knowledge of the laser lights and the tissue interactions produced by the absorption of this coherent light in the specific cromophore, the hemoglobin, without affect the surrounding tissue, except the whole vessel layers. J Am Acad Dermatol 2002 Jan;46(1):66-72 A dual wavelength approach for laser/intense pulsed light source treatment of lower extremity veins Sadick NS BACKGROUND: Consistent reproducible aesthetic results are a desired component of laser/intense pulsed light (IPL) treatment of lower extremity blood vessels. In this regard, shorter wavelengths may be used to treat fine red telangiectases, whereas longer wavelengths may be used to treat larger diameter blue venulectasia and small reticular veins. OBJECTIVE: The purpose of the present study was to demonstrate that a bimodal wavelength approach to laser/IPL source treatment for lower extremity vessels up to 8 mm in diameter produces results superior to previously described photothermolytic approaches for eradication of unwanted lower extremity blood vessels. METHODS: Fifty female patients (mean age, 37 years) were treated in a private practice setting with class I-III red telangiectasia, blue venulectasia, and reticular veins (0.1-4.0 mm in diameter) on the inner or outer thighs. A combined approach of laser/IPL treatment was used; patients had up to 3 treatments at 6-week intervals on a 5-cm2 surface area of vessels with the use of an IPL source wavelength of 550 nm, fluence of 40 J/cm2, for treatment of red telangiectases less than 1 mm in diameter, while a 1064-nm Nd:YAG laser at a fluence of 140 J/cm2 was used to treat venulectases and reticular vessels that were 1.0 to 4.0 mm in diameter. Results were analyzed by macrophotographic imaging, double-blinded observer evaluation, optical chromatography, and a patient evaluation scale. RESULTS: An average of 2(1/2) patient sessions produced significant clearing (75%-100%) in 80% of patients. The mean erythema index showed significant lightening (35.3+dl) in the study population. Finally, 76% of patients reported great satisfaction with the treatment results. CONCLUSION: A bimodal wavelength approach utilizing both short and long wavelengths produces significant clearing of the variably colored, multiple-diameter/depth array of vessels, which commonly presents a therapeutic challenge to the vascular laser surgeon. LASER ARGON Lasers Surg Med 1984;4(3):221-31 Use of the argon and carbon dioxide lasers for treatment of superficial venous varicosities of the lower extremity Apfelberg DB, Maser MR, Lash H, White DN, Flores JT Superficial telangiectasia of the lower extremity in 38 patients was treated with both argon and CO2 lasers. Results after five months revealed no change or worsening of the veins in 49% of the patients and good to excellent improvement or segmentation in 16% of the patients. The most common complication was brown hemosiderin bruising in almost half of the patients. Phlebologie 1984 Apr-Jun;37(2):229-34 Role of the argon laser in the treatment of varicose veins of the legs. Apropos of 17 cases Beranger P The Argon is not just a fashionable sophisticated toy; it has definite indications in the field of phlebology: varicosities which can not be catheterised, flat angiomas, angiokeratoses and pigmented lesions. Some of its major advantages are the possibility of treating a large number of angiectases at the one session; the low risk of recurrence of the treated lesions in comparison with other methods and the excellent healing (respect of the pilosebaceous adnexae) which, however, is slower than for acne rosacea. Red angiectases respond better than blue lesions which require higher intensity laser. The major disadvantage is the cost, which justifies the creation of multi-disciplinary units (Ophtalmology, Gastro-enterology...). The techniques of laser coagulation still have to be defined (continuous or intermittent, intensity, time of irradiation). Finally, the skin of the legs acts as a shield by the thickness of the horny layer which absorbs or reflects the radiat LASER HELIUM-NEON Vestn Khir Im I I Grek 1984 Jan;132(1):69-71 Use of the helium-neon laser in the treatment of crural varicose ulcers Usik VS Results of the laser therapy of varicose ulcers of the crus in 45 patients were analyzed. The laser therapy is considered by the author to favourably influence the healing of the ulcers, to reduce pain, edema and skin hyperemia. LASER A COLORANT J Dermatol Surg Oncol 1990 Apr;16(4):338-44 Pulsed-dye laser treatment of leg telangiectasia: with and without simultaneous sclerotherapy Goldman MP, Fitzpatrick RE Thirty consecutive female patients with red leg telangiectasia less than 0.2 mm in diameter were treated with a Candela SPTL-1 Pulsed Dye Laser (PDL) tuned to 585 nm with a pulse duration of 450 microseconds at energies ranging from 6.0 to 8.5 J/cm2 delivered through a 5-mm spot size to the entire length of the telangiectasia. Seven patients with 25 patches of telangiectatic matting after previous sclerotherapy were also treated. Twenty-seven patients with symmetrical telangiectatic patches or a large "starburst" telangiectatic flair that could be divided into two separate treatment sites were treated at one site with PDL alone, and at the other site with a combination of PDL followed immediately by sclerotherapy (SCL) with Polidocanol 0.1-0.25 ml per injection site at a concentration of either 0.25%, 0.5%, or 0.75%. PDL treatment is efficacious for both essential telangiectasia and vessels that arise through the phenomena of telangiectatic matting. Sixty-five percent of vessels are completely faded with treatment. PDL alone has a remarkably low incidence of adverse sequelae. Treatment is most efficacious if all vessels larger than 0.2 mm in diameter, especially varicose and reticular feeding veins, are treated first. Treatment results are not affected by vessel location. And post-treatment compression of this type of vessel appears unnecessary. Combination PDL/SCL treatment appears to offer no advantage to sclerotherapy treatment alone and has a significant degree of complications when treatment is limited to red telangiectasia less than 0.2 mm in diameter with the laser parameters utilized. J Am Acad Dermatol 1990 Jul;23(1):23-30 Pulsed dye laser treatment of telangiectases with and without subtherapeutic sclerotherapy. Clinical and histologic examination in the rabbit ear vein model Goldman MP, Martin DE, Fitzpatrick RE, Ruiz-Esparza J The treatment of leg telangiectases with the carbon dioxide or argon laser results in a low success rate and an unacceptable risk of scarring. Sclerotherapy is effective; however, pigmentation and telangiectatic matting induced by extravasation of RBCs and excessive posttreatment inflammation are common. We conducted a clinical and histologic study of therapy with the 585 nm pulsed dye laser alone and in combination with subtherapeutic sclerotherapy in the rabbit ear vein model. The pulsed dye laser alone was effective when 10 joule/cm2 was used. In combination with immediate injection of the sclerosant, effective endosclerosis occurred with all tested laser energies (8 to 10 joule/cm2). Surgery 1991 Feb;109(2):163-8 A preliminary study of dye-enhanced laser photosclerosis Libutti SK, Oz MC, Chuck RS, Auteri JS, Treat MR, Nowygrod R Laser ablation of veins after injection of wavelength-specific dyes to enhance and localize energy absorption could provide a useful adjunct to current treatment options. To enhance the absorption of diode laser energy at 808 nm, ear veins of 41 rabbits were infused with 2 to 3 ml of indocyanine green dye (maximum absorption, 805 nm) and exposed for 2 to 20 seconds. Animals were killed between 0 and 28 days after operation. Discrete time intervals of laser exposure exist during which various-sized vessels can be ablated without significant thermal injury to the overlying tissue. Small vessels (0.2 mm in diameter) blanch after 2 to 3 seconds of exposure, whereas medium-sized vessels (2 mm in diameter) require 8 to 10 seconds. Vessels can be ablated with a power density as low as 11.1 W/cm2. Specimens taken immediately after laser exposure show vessel wall thinning and a reirradiation effect, created as laser energy initially absorbed by dye is reemitted. By the seventh day after operation, a brisk inflammatory response and acanthosis of the overlying epidermal layer develop. The lumen is partially filled by thrombus with cellular invasion. By postoperative day 28, the epidermal thickening and inflammatory reaction have resolved; the vessel walls are fibrotic. The use of low-power, air-cooled diode lasers, in conjunction with wavelength-specific dyes, may provide a simple, viable, and cosmetically appealing alternative to the treatment of superficial varicosities of the extremities. Lasers Surg Med 1997;20(1):1-5 Treatment of leg telangiectasia using a long-pulse dye laser at 595 nm Hsia J, Lowery JA, Zelickson B BACKGROUND AND OBJECTIVE: Pulsed dye lasers (PDL) operating at 585 nm wavelength and 0.45 msec pulsewidth offer effective treatment for port wine stains (PWS). Vessels in leg telangiectasias are larger than those in PWS. Longer pulsewidths and wavelengths may improve clearance of these larger vessels. STUDY DESIGN/MATERIALS AND METHODS: Twenty patients were treated using PDL at 595 nm and 1.5 msec. Vessel diameters ranging from 0.635 to 1.067 mm were treated using energy densities of 15 and 18 J/cm2, and a 2 x 7 mm elliptical spot. Telangiectasia clearance and complications were scored at 6-weeks and 5-months following the single treatment. RESULTS: Results demonstrated > 50% clearance by 6 weeks in 11/26 (42.3%) patients using 15 J/cm2, and 6/13 (45.2%) using 18 J/cm2. By 5 months > 50% clearance was noted in 18/34 (53.0%) using 15 J/cm2, and 11/17 (64.7%) using 18 J/cm2. Complications were minor and infrequent. CONCLUSION: The long-pulse PDL may have a role in treating leg telangiectasias. Australas J Dermatol 1997 Feb;38(1):22-5 Pulsed dye laser treatment of spider telangiectasia Tan E, Vinciullo C Spider telangiectasia is a common benign vascular malformation which can be a source of cosmetic concern for the patient. A retrospective review of 30 adults and children with spider telangiectasia treated by the flashlamp-pumped pulsed dye laser was undertaken. There was complete clearance of treated spider telangiectasia in 93% of patients after a single treatment. There were no reported permanent adverse effects with purpura being the only transient problem. Most patients were satisfied with the eventual results of treatment and would recommend treatment to other people with a similar problem. This laser should be considered as the treatment of choice for spider telangiectasia. Lasers Surg Med 1998;23(2):72-8 Leg telangiectasia treatment with a 1.5 ms pulsed dye laser, ice cube cooling of the skin and 595 vs 600 nm: preliminary results Hohenleutner U, Walther T, Wenig M, Baumler W, Landthaler M Department of Dermatology, University of Regensburg, Germany. BACKGROUND AND OBJECTIVE: Preliminary results indicate that pulsed dye lasers (PDL) with 1.5 ms pulsewidth and 595 nm wavelength are effective in the treatment of leg telangiectasia. The aim of this study was to evaluate if the clinical results could be improved by a) an effective skin cooling with ice cubes and b) the longer wavelength of 600 nm. STUDY DESIGN/MATERIALS AND METHODS: In 87 patients with vessels up to 1 mm in diameter, 257 single test treatments were performed using wavelengths of 595 and 600 nm, fluences of 16, 18, and 20 J/cm2, a 1.5 ms pulse duration, and an elliptical spot of 2 x 7 mm. In 7 patients, the skin surface temperature curve was measured after cooling with ice cubes vs hydrogel dressings, and spot geometry and fluence were investigated with and without the gel dressing. RESULTS: Vessel clearance was evaluated 6-8 weeks after treatment. 20 J/cm2 were most effective (80% clearance >50%), and 18 J/cm2 were more effective than 16 J/cm2 (66.2 vs 52.5% clearance >50%). There was a tendency towards better results with 595 nm, but the differences were not significant. Vessels with a diameter <0.5 mm cleared significantly better than those with 0.5-1 mm (69.1 vs 31.9% clearance >50%). Hypo- and hyperpigmentation were seen in 32% of the patients. Cooling with ice cubes proved to be far more effective than with hydrogel dressings (temperature decrease approx 15 vs 5 degrees C). Additionally, the gel dressing caused an energy loss of approx 35% and an irregular spot geometry as shown on burn paper. CONCLUSIONS: Treatment of leg telangiectasia with the 1.5 ms-PDL is safe and effective, especially in vessels smaller than 0.5 mm in diameter; 595 nm and 18 J/cm2 seem to be somewhat more effective as 600 nm and 16 J/cm2; and 20 J/cm2 are even more effective, but persistent hyperpigmentation cannot yet be excluded due to insufficient follow-up time. Cooling with ice cubes is more effective and less expensive than gel dressings, and the short term clinical results are equivalent, even if the frequency of transient pigmentary changes is increased. Hautarzt 1998 Jul;49(7):560-5 Treatment of superficial varicosities with a flashlamp-pumped pulsed dye laser with 1.5 ms impulse time Hohenleutner U, Wenig M, Walther T, Baumler W, Landthaler M A new flashlamp-pumped pulsed dye laser with 1.5 ms pulse length and tunable wavelengths between 585 and 600 nm (Candela ScleroPLUS) is now available for the treatment of ectatic leg veins. We evaluated 232 single test treatments using 595 and 600 nm wavelength in 75 test persons. For smaller vessels up to a diameter of 0.5 mm, treatments at 16 and 18 J/cm2 showed good results in 60 and 82% respectively; for vessels up to 1 mm in 27 and 33%. Treatment at 595 nm was a little more effective than at 600 nm. Larger vessels could not be treated effectively. The main side effects consisted in hyper-(34%) or hypopigmentation (30%). Thus, in addition to the usual sclerotherapy, this laser is a useful device for the treatment of leg vein ectasia. Dermatol Surg 1998 Jul;24(7):737-40 Evaluation of the long-pulse dye laser for the treatment of leg telangiectasias Reichert D BACKGROUND: Leg telangiectasias are common visible ecstatic dermal capillaries, arterioles, or veins. Multiple methods of treatment have been reported for this entity. A long-pulse (1500 microsecond) dye laser has been developed to treat leg veins ranging in size from 0.1 to 1.0 mm in diameter. OBJECTIVE: To determine the effectiveness of this novel device on treating leg veins with varying wavelengths and fluences. METHODS: Eight patients with more than 250 sites of leg telangiectasis were treated with the long-pulse dye laser. RESULTS: Clearance of 100% was achieved after one or two treatments by vessels with diameters up to 0.5 mm. Vessels with diameters between 0.5 and 1.0 mm faded in about 80% of treatments. Transient adverse affects were observed in a low incidence. CONCLUSIONS: The long-pulse dye laser is a safe and effective tool in the treatment of leg telangiectasias. J Am Acad Dermatol 1998 Nov;39(5 Pt 1):746-50 Comment in: J Am Acad Dermatol. 2000 May;42(5 Pt 1):849-50. Treatment of spider veins with the 595 nm pulsed-dye laser Bernstein EF, Lee J, Lowery J, Brown DB, Geronemus R, Lask G, Hsia J BACKGROUND: Previous attempts to treat spider veins with the conventional 585 nm pulsed-dye laser with a 0.5-ms pulse duration have been relatively ineffective. Recently, a new pulsed-dye laser that is tunable from 585 to 600 nm with a pulse duration 3 times longer than previously available lasers has preliminarily been shown to be effective for treatment of spider veins. OBJECTIVE: Our purpose was to evaluate the effectiveness of multiple treatments with the tunable long-pulse dye laser in treatment of spider veins of the lower extremity. METHODS: Ten female volunteers were treated in two separate areas containing blue or red linear spider veins less than 1.5 mm in diameter. Treatments were administered with the pulsed-dye laser with a 1.5-ms pulse duration and 595-nm light at fluences of 15 and 20 J/cm2, and each subject received a total of 3 treatments at each site, administered at 6-week intervals. Photographs were taken before and 6 weeks after the last treatment. RESULTS: Computer-based image analysis showed clearing of more than three fourths of veins after 3 treatments with 15 or 20 J/cm2. Side effects were minimal and the treatments were well tolerated. CONCLUSION: The 595 nm, 1.5 ms pulse duration, pulsed-dye laser is safe and effective for treating blue or red spider veins of the lower extremities less than 1.5 mm in diameter in nontanned patients with Fitzpatrick skin types I and II. Multiple treatments improve on the results obtained after a single treatment. Dermatol Surg 1999 Jun;25(6):445-9 Comparison of the 595 nm long-pulse (1.5 msec) and ultralong-pulse (4 msec) lasers in the treatment of leg veins Alora MB, Stern RS, Arndt KA, Dover JS BACKGROUND: Although several lasers and light sources are now available for vascular lesions, treatment of leg veins has not been very satisfactory. Lengthening the pulse width should theoretically result in improved response rates. OBJECTIVE: This study compared the efficacy and safety of 595 nm pulsed lasers at 1.5 msec and 4 msec in treating leg veins. METHODS: For group A, 27 healthy adult volunteers with leg veins measuring less than 1 mm in diameter were treated with a 2 mm x 7 mm elliptical handpiece. Each patient had three areas treated. The first two areas were treated with the 4 msec pulsed dye laser with fluences of 16 and 20 J/cm2, while the last area was treated with a 1.5 msec pulsed dye laser at fluences ranging from 14 to 16 J/cm2. For group B, 13 subjects were treated. Areas 1 and 2 were treated with the 4 msec pulsed dye laser using a 3 mm x 5 mm and 5 mm handpiece, respectively, while the third site was treated with a 1.5 msec laser using a 3 mm x 5 mm handpiece. Fluences ranging from 14 to 16 J/cm2 were used. Clinical evaluations were performed and photographs taken at 4-8 week intervals. RESULTS: Neither laser regularly induced satisfactory diminution or disappearance of these vessels after one treatment. In group A, more than 50% of patients had little to no improvement, while in group B little to no improvement was observed in 33% of patients following a single treatment. Although there was no significant difference in outcomes between the test sites, the 4 msec PDL with a 3 mm x 5 mm spot size appeared to be most effective. Transient hyperpigmentation was common following either treatment, while hypopigmentation was seen in group B subjects. No scarring was noted. CONCLUSION: Both the 4 and 1.5 msec flashlamp-pumped pulsed dye lasers were ineffective in treating leg telangiectasia following a single treatment. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 243 Laser-therapy as part of a combined treatment in chronic venous insufficiency J Ley, G. Canellas, I. Guijo, M.E. Vega Although different equipments for laser therapy of vascular lesions are available, reported results are not always satisfactory. The aim of this study was to evaluate the effectivity of the laser treatment in varicose veins. We included ail the patients (N=244) who finished their treatment in our clinic from October 2000 to January 2001 with clinical diagnosis of chronic venous insufficiency All patients were evaluated using color-coded Doppler sonography of the lower limbs. Surgical treatment was applied when vessel diameter was greater than 4 mm. Isolated surgical treatment was required in only 24 patients (9,8 %). No surgical treatment was necessary in 143 patients (58%). 29 patients were excluded because they did sot finished the treatment or refused sclerotherapy and laser. Afterwards, the patients were divided at random in two groups: (A) who received sclerotherapy with polidocanol (0,5% -1%) and cromated glicerine (N=89) and (B) the same sclerotherapy and laser Vbeam Candela (595 nm) with pulse duration from 10 to 30 ms and fluencies from 11 to 14 J/cm2 (N=102). Only two sessions of laser treatment were applied to each patient in the same area. Photographic assessment of venous dilatations was performed before and alter each treatment. In group A, clearing of more than 75% of telangiectases was reached in 46 patients while in Group B the similar result was reached in 89 cases (p<0,001). Laser-therapy seems to be a good alternative for the treatment of telangiectases, having reduced the venous pressure by sclerotherapy or surgery. J Cosmet Laser Ther. 2003 Jun;5(2):71-5 Treatment of telangiectasia using the multi-pass technique with the extended pulse width, pulsed dye laser (Cynosure V-Star) Tanghetti E, Sherr E BACKGROUND: The pulsed dye laser (PDL) has been used for the treatment of facial and leg telangiectasia, where it provides safe and effective treatment. Often, a single treatment with the PDL can provide acceptable vessel clearance. Unfortunately, the hallmark of PDL treatment is transient purpura, which can be cosmetically unacceptable to patients. A new class of PDL has been developed in an effort to reduce this transient side effect while maintaining both safety and efficacy. OBJECTIVE: To evaluate the ability of multi-pass treatment for telangiectasia with extended pulse width (40 ms) PDL to provide effective, single-treatment vessel treatment without inducing purpura. METHODS: A total of 40 patients presenting with facial or leg telangiectasia were treated with the extended pulse width PDL (595 nm), used in conjunction with refrigerated air-cooling (SmartCool; Cynosure). Treatment was given using a pulse width of 40 ms and fluences at or below the purpuric threshold (less than 16 J/cm(2)) and with high-flow air cooling at -4 degrees C. Up to three passes were given until vessel disappearance or intravascular coagulation was observed. A second treatment was done, where needed, 4-8 weeks following the initial treatment. Patients were evaluated 4, 8, and 12 weeks after the final treatment. RESULTS: Following a single treatment, 70% of facial and 80% of leg vessels exhibited at least 75% clearance. After two treatments, 14/20 leg vessels cleared at 75-100%. In all cases, vessel clearance was associated with transient purpura lasting less than 7 days. Hyperpigmentation occurred in 5% of facial vessels and 55% of leg veins. Sub-purpuric doses did not provide acceptable single-treatment clearance. CONCLUSIONS: Extended pulse width dye lasers significantly increase the threshold for purpura, allowing higher fluences to be employed. For the goal of single treatment vessel clearance, the extended pulse duration provided acceptable, single-treatment improvement but only in the presence of purpura. While additional, non-purpuric treatments may provide acceptable outcomes, additional improvements will be necessary to provide consistent, effective, single-treatment clearance of telangiectasia without generalized purpura. Dermatol Surg. 2003 Dec;29(12):1176-80; discussion 1180 532-nm Nd:YAG and 595-nm pulsed dye laser treatment of leg telangiectasia using ultralong pulse duration Woo WK, Jasim ZF, Handley JM BACKGROUND: Telangiectatic leg veins have been treated using lasers with variable success. OBJECTIVE: We aimed to examine the efficacy and tolerability of a 595-nm pulsed dye laser (PDL) and a 532-nm Nd:YAG laser using ultralong pulse duration to improve leg telangiectasias with a single treatment. METHODS: Ten subjects with leg telangiectasias up to 1.0 mm in diameter participated in the study. The telangiectatic patch was divided into two approximately equal adjacent areas. The first area was treated with a 532-nm Nd:YAG laser at a fluence of 20 J/cm2 and a pulse duration of 50 ms using a contact cooling device. The second area was treated with a 595-nm PDL at a fluence of 25 J/cm2 and a pulse duration of 40 ms using cryogen spray precooling. Each area was treated once only. Photographic evaluation was used for an assessment of response. RESULTS: Two of 10 subjects had less than 25%, 3 had 25% to 50%, 2 had 50% to 75%, and 3 had more than 75% improvement after single treatment with a 532-nm Nd:YAG laser. Similarly, 2 of 10 subjects had less than 25%, 2 had 25% to 50%, and 6 had 50% to 75% improvement with the 595-nm PDL. Hyperpigmentation occurred in one subject treated with the 532-nm Nd:YAG laser and two subjects treated with the 595-nm PDL. No blistering, crusting, hypopigmentation, or scarring were observed. CONCLUSION: Both lasers using ultralong pulse width improved leg telangiectasias after a single treatment with minimal adverse reactions. Lasers Surg Med. 2004;35(1):62-7 Treatment of leg veins with the long pulse dye laser using variable pulse durations and energy fluences. Kono T, Yamaki T, Ercocen AR, Fujiwara O, Nozaki M BACKGROUND AND OBJECTIVES: Attempts at using the pulsed dye laser (PDL) operating at 585 nm wavelength and 0.45 milliseconds pulse duration to treat leg veins have been notably unsuccessful. The aim of this study is to evaluate the efficacy and complications of the 595 nm long PDL in the treatment of leg veins. STUDY DESIGN/PATIENTS AND METHODS: Fourteen patients with 38 lesions were treated using a long PDL equipped with a cryogen spray cooling (CSC) device. Variable pulse durations ranging from 1.5 to 20 milliseconds and energy fluences from 10 to 20 J/cm2 were utilized depending on the size of treated vessels. All patients received two laser treatments at an interval of 2 months. RESULTS: Of patients with veins type 1A and type 1, 6 (100%) and 3 (13%) had complete clearing, respectively. Of patients with veins type 1 and type 2, 18 (78.3%) and 2 (22.2%) lesions showed excellent response, respectively. Hyperpigmentation was the only observed complication lasting several months in 57.9% of treated sites. CONCLUSIONS: The long PDL operating at 595 nm is a safe and effective treatment for leg veins, especially in type 1A and type1 vessels. Lasers Surg Med. 2005 Jul;37(1):19-28 Epidermal and vascular damage analysis of in vivo human skin in response to 595 nm pulsed laser irradiation Pikkula BM, Chang DW, Dai T, Anvari B BACKGROUND AND OBJECTIVES: Laser irradiation is the current modality for treatment of cutaneous hypervascular malformations such as port wine stains and telangiectasia. Although cryogen spray cooling (CSC) is used to protect the epidermis from non-specific laser-induced thermal damage in moderately-pigmented skin types, individuals with high melanin content are still at risk for epidermal damage using the current laser irradiation and CSC parameters. The objective of this study was to investigate the influence of the spray Weber number (1,100 or 5,100) on epidermal protection and examine vascular coagulation in response to pulsed dye laser irradiation. STUDY DESIGN/MATERIALS AND METHODS: Normal, in vivo human skin from eight subjects of Fitzpatrick skin types I-V were precooled with either low or high Weber number cryogen sprays and subsequently irradiated with a pulsed dye laser at 595 nm. Analysis of gross purpura, morphological vascular damage, and apoptosis of the vascular walls were performed. RESULTS: Results demonstrated a high Weber number spray of 5,100 decreased the level of epidermal damage in darker and moderate pigmented individuals compared to a Weber number spray of 1,100. This study also established a positive correlation between gross purpura and the level of vessel wall apoptosis. CONCLUSIONS: This study has demonstrated that CSC with a high Weber number spray can decrease nonspecific thermal damage to the epidermis in response to laser irradiation in vivo. We have also established a positive correlation between gross purpura and the level of vessel wall apoptosis. Lasers Surg. Br J Plast Surg. 2005 Oct;58(7):981-7 Pulsed dye laser treatment, a review of indications and outcome based on published trials Smit JM, Bauland CG, Wijnberg DS, Spauwen PH INTRODUCTION: Pulsed dye laser (PDL) treatment is based on the principle of selective photothermolysis and is widely considered to be the treatment of choice for a variety of cutaneous vascular lesions. OBJECTIVE: To review the indications and outcome of PDL treatment and summarise new developments. METHOD: A literature-based study has been conducted entailing the review of publications over the period January 1993-December 2003 using the databases Medline and Cochrane CENTRAL. RESULTS: The PDL was found to be effective in port wine stain, facial telangiectasia, leg telangiectasia <0.5 mm, scars, hypertrophic scars and ulcerated haemangioma. DISCUSSION: Essential characteristics of lesions suitable for PDL treatment are discussed and guidelines are presented for future research. Dermatol Surg. 2006 Jan;32(1):41-8 Treatment of vascular skin lesions with the variable-pulse 595 nm pulsed dye laser Woo SH, Ahn HH, Kim SN, Kye YC BACKGROUND: In the dermatology field, variable-pulse 595 nm pulsed dye lasers (PDLs) are now being widely used to treat vascular skin lesions. However, there is little information available on variable-pulse 595 nm PDL treatment of dark-skinned patients. OBJECTIVE: The objective of this study was to evaluate the outcome of variable-pulse 595 nm PDL treatment on Korean patients. METHOD: Two hundred thirty-nine patients (Fitzpatrick skin phototypes III to V) with vascular skin lesions, such as nevus flammeus, telangiectasia, or hemangioma, were included in this study. All patients were treated with a variable-pulse 595 nm PDL, and the outcomes were assessed by comparing preoperative and postoperative photographs. RESULTS: The average number of treatments per patient was 4.29, and 51.9% of patients showed a good (51-75% clearance) to excellent (76-100% clearance) response. For nevus flammeus, 48.0% of the patients achieved good to excellent results. The gender and age of the patients did not influence the clinical response; however, lesions of the head and neck were found to respond more favorably to treatment. For telangiectasia, 78.0% of patients showed good to excellent results, and, again, the gender and age of the patients did not alter the treatment outcome. For hemangioma, the male to female ratio of patients was 1.0:3.1 and 54.1% of the patients achieved a good to excellent response. Superficial hemangioma showed a better clinical response than deep hemangioma, and the lesions of younger patients responded more favorably than those of older patients. CONCLUSION: The variable-pulse 595 nm PDL was found to be effective for treating several vascular skin lesions in dark-skinned patients. However, there were differences in treatment outcome owing to disease, age, and the location of the lesions. Sivarajan V, Al Aissami M, Maclaren W, Mackay IR Recurrence of spider naevi following treatment with 585 nm pulsed dye laser J Plast Reconstr Aesthet Surg. 2007;60(6):668-71. Epub 2007 Jan 26 During a 2-year period 201 patients underwent treatment for spider naevi with a 585nm pulsed dye laser at Canniesburn Hospital Laser Suite. Patients were treated with a either single or double pulse technique. Of these patients 191 (95%) had a successful result, with clearance in a mean of 1.8 treatments (range, 1-7). There was no significant difference between the two treatment protocols in terms of probability of clearing the lesion or number of treatments required. These 191 patients were contacted by postal survey to determine their long-term results. The mean duration of follow-up was 37.9 months (range, 27-51 months). Response rate to the survey was 73%, 139 patients. Fifty patients (36%) had suffered recurrence of their spider naevi in the same site. There was no correlation found between the risk of recurrence and the site, number of treatments received, size and characteristics of the spider naevus, or treatment protocol used. The risk of recurrence increased with increasing age and was higher for peripheral facial lesions. The most common time of recurrence was between 6 and 18 months with 48% of recurrences occurring during this period. Existing published series, which have demonstrated low recurrence rates, have either had low numbers of patients or short follow-up periods of less than 6 months. Bernstein EF The new-generation, high-energy, 595 nm, long pulse-duration, pulsed-dye laser effectively removes spider veins of the lower extremity Lasers Surg Med. 2007 Mar;39(3):218-24 BACKGROUND AND OBJECTIVES: Lower-extremity spider veins are a cosmetic problem that poses formidable clinical difficulty for laser removal. They are significantly harder to remove than facial telangiectasias. A new-generation, pulsed-dye laser (PDL), capable of administering pulses that clinically behave like true 40-millisecond pulses has been developed, by doubling the number of sub-pulses comprising each laser pulse. STUDY DESIGN/MATERIALS AND METHODS: Fifteen subjects with Fitzpatrick skin types I-III were enrolled in the study and treated to 35 sites. Subjects were treated three times at 6-week intervals using an average fluence of 20.4 J/cm(2), a 3 x 10 mm spot, and a dynamic cooling device to protect the epidermis. Digital photographs were taken before initiating treatment and 8 weeks following the final treatment. RESULTS: Mean improvement scores using a 4-point scale as rated subjectively by the treating physician were 0.92 (<25%), 2.7 (approximately 40-50%), and 3.6 (approximately 65-75%), 6 weeks following 1st and 2nd treatments and 8 weeks following the 3rd and final treatment, respectively. Improvement was also determined by three physicians, rating digital photographs and blinded as to which photographs were pre- or post-treatment. They rated improvement as mild (0-25%) in 10.5% of photographs, moderate (26-50%) in 15.2%, marked (51-75%) in 38.1%, and excellent (76-100%) in 6.3%. There was no textural change in any treatment site. CONCLUSIONS: The new-generation, high-energy, 595 nm, long pulse-duration, PDL effectively removes lower-extremity spider veins in subjects with skin types I-III. ALEXANDRITE 755 nm Dermatol Surg 1999 Jan;25(1):52-8 Laser therapy of spider leg veins: clinical evaluation of a new long pulsed alexandrite laser McDaniel DH, Ash K, Lord J, Newman J, Adrian RM, Zukowski M BACKGROUND: The response of spider leg veins to laser or intense pulsed light therapy has generally been characterized by varying degrees of success and frequently inconsistent clinical response rates. OBJECTIVE: The purpose of this study was to examine the effectiveness of the 755 nm long pulsed infrared alexandrite (LPA) laser for the treatment of leg telangiectasias. METHODS: This study was constructed in four phases. Phase I examined 28 patients with variable sized telangiectasias using 5 treatment parameters (15 J/cm2 x 1 pulse, 20 J/cm2 x 1 pulse, 20 J/cm2 x 2 pulses, 20 J/cm2 x 3 pulses, or 30 J/cm2 x 1 pulse). Each patient received 3 treatments at 4 week intervals with the LPA. Patient diaries were obtained to examine the effects of the treatments. Subjective grading was performed at each follow-up visit by the investigators. Blinded objective grading was performed at the conclusion of the study by trained observers. Phase II examined the effects of these treatment parameters on varying vessel diameters. Vessels were grouped into small (<0.4 mm), intermediate (0.4-1.0 mm), and large (1.0-3.0 mm) subsets. Phase III examined the effects of a combination of LPA treatment followed by 23.4% hypertonic saline sclerotherapy. Subjective and blinded objective grading was used to determine improvement after a single treatment with the LPA at 20 J/cm2, single pulsed with a pulse duration of 5 or 10 msec followed by treatment with 23.4% hypertonic saline injected 3, 7, 14, or 28 days after laser therapy. Phase IV involved biopsies after LPA treatment alone at time intervals of immediately posttreatment and 5 and 21 days posttreatment. RESULTS: These evaluations revealed that the optimal treatment parameters for LPA therapy alone appeared to be 20 J/cm2, double pulsed at a repetition rate of one Hz. After 3 treatments at 4 week intervals, subjective grading indicated a 63% reduction in leg telangiectasias. Medium diameter vessels responded best with small vessel diameters responding poorly, if at all. The addition of 23.4% hypertonic saline sclerotherapy performed 3 to 7 days after laser therapy (LPA at 20 J/cm2, single pulsed with a pulse duration of 5 msec) produced 87% reduction in leg telangiectasias. Biopsies after LPA treatment revealed vessel wall endothelial cell necrosis at 5 days with fibrosis occurring at 3 weeks. The optimal clinical "window" for sclerotherapy seems to coincide with the period of endothelial cell necrosis. CONCLUSION: LPA therapy is most effective for leg telangiectasias 0.4-3.0 mm in diameter. This LPA technique is significantly improved with the addition of sclerotherapy. Arch Dermatol 2000 Nov;136(11):1371-5 Pulsed alexandrite laser for the treatment of leg telangiectasia and reticular veins Kauvar AN, Lou WW OBJECTIVE: To examine the safety and efficacy of a pulsed alexandrite laser for treatment of leg telangiectasia and reticular veins. DESIGN: Observational study. SETTING: Laser and Skin Surgery Center of New York, New York, NY. SUBJECTS: Twenty women with skin phototypes I to III and with 54 patches of leg veins measuring 0.3 to 2.0 mm in diameter. INTERVENTIONS: Each patch was treated once using 1 to 3 passes of a 755-mm, 3-millisecond alexandrite laser. An 8-mm spot and fluences of 60 to 80 J/cm(2) were used, with dynamic epidermal cooling. MAIN OUTCOME MEASURES: Subjects underwent evaluation at 4 and 12 weeks for degree of clearance, based on a quartile grading system, and incidence of adverse effects. RESULTS: At the 4-week follow-up, 17 (35%) of 48 treatment sites showed greater than 75% clearance and an additional 16 (33%) showed greater than 50% clearance. By 12 weeks, 33 (65%) of 51 treatment sites showed greater than 75% clearance, and there was greater than 50% clearance in an additional 11 (22%). Hyperpigmentation was observed in 18 (35%) of 51 treatment sites. CONCLUSION: A single treatment with a 755-nm, 3-millisecond alexandrite laser at high fluence in conjunction with cryogen skin cooling produced excellent clearance of telangiectasia and reticular veins of the leg with minimal adverse effects. Lasers Surg Med. 2009 Feb 18;41(2):104-109. [Epub ahead of print] Optimal pulse durations for the treatment of leg telangiectasias with an alexandrite laser Ross EV, Meehan KJ, Gilbert S, Domankevitz Y BACKGROUND AND OBJECTIVES: Determine optimal settings using a long pulse 755 nm alexandrite laser in the treatment of superficial leg veins. STUDY DESIGN\MATERIALS AND METHODS: Fifteen patients with Fitzpatrick skin types I-III with telangiectasia ranging from 0.2 to 1.0 mm were enrolled. Spot size varied from 3 to 6 mm. Pulse durations ranged from 3 to 100 milliseconds. For each pulse duration, test sites were performed to determine threshold radiant exposures using persistent bluing and/or immediate stenosis (closure) as the clinical endpoint. Test sites were re-evaluated 21 days later. Optimal settings, those that resulted in the greatest clearance with minimal side effects (pain, purpura, epidermal damage, pigment changes), were used to treat a larger area of like-sized vessels. Follow-up evaluations were conducted 12 weeks after a single treatment using the optimal setting. Polarized digital photographs were obtained at each visit. Improvement was determined by blinded evaluation of pre/post-treatment photographs. RESULTS: Fourteen patients completed the study. Radiant exposure thresholds for immediate vessel changes depended on vessel diameter, with larger radiant exposures required for smaller spot sizes and smaller vessels. The average threshold radiant exposure for closure was 89 J/cm(2). The optimal pulse duration was 60 milliseconds for most of the patients. With this pulse width, clearance approached 65% 12 weeks after a single treatment. Transient hyperpigmentation occurred in four patients. Increasing the pulse duration improved epidermal tolerance and decreased the likelihood of purpura. CONCLUSIONS: By lengthening the pulsewidth beyond 3 milliseconds, a long pulse alexandrite laser achieves satisfactory clearance with an improved side effect profile. 810 nm Clin Exp Dermatol 2000 Jul;25(5):419-22 Laser therapy of telangiectatic leg veins: clinical evaluation of the 810 nm diode laser Varma S, Lanigan SW Telangiectatic leg veins (TLV) are experienced by millions of women and men. As they cause significant cosmetic embarrassment, many women seek effective treatment. Options include sclerotherapy and treatment with different lasers. We investigated the safety and efficacy of an 810-nm diode laser in the treatment of TLV. Ten females had treatment to a >/= 25 cm2 area of TLV four times at 4-weekly intervals at 25-35 W, 0.1 s duration, 0.5 s interval and a 5-mm circular spot size (fluence of 12.7-17.8 J/cm2). Assessment of response was performed 4 weeks after the final treatment and patients were asked to complete a questionnaire requesting information regarding the treatment. No statistically significant clearing of the leg veins was demonstrated although some improvement was noted in individual patients. Side-effects were negligible, consisting of discomfort or mild pain. There was no scarring, purpura or pigment alteration. A visual analogue scale questionnaire (0-10) revealed that patients found the treatment acceptable (range, 4-10). Overall difference as assessed by the patients ranged from 0 to 8.4 and degree of satisfaction with the treatment from 0 to 9.8. Currently, the treatment of choice for TLV remains sclerotherapy. Our results suggest that the 810-nm diode laser is safe and well tolerated. Further research could establish whether effectiveness can be improved with higher fluences or in combination with sclerotherapy. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 240 The 810 diode LASER in the treatment of telangiectasias and spider veins This study was performed on 500 patients presenting varicosities or telangiectasias. All the reflux were treated before by surgery and sclerotherapy. The assesment was made on the age , the hormonal treatment, the phototype (according to Fitzpatrick) The classification of varicosities was made as follow Type of veins : systematized, non systematized, matting Color: red purple or blue Level on the member: thigh , calf, foot Recoloring time alter pressure Visual scale of satisfaction for patient and physician Side effects The results will be presented during the congress 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 241 Photodynamic treatment with diode laser of lower limbs telangectasia previously injected with methylene blue: a preliminary report Pepe, N, Gioffre L, Mancini G, Meloni V Authors report first results of 50 photodynamic treatments with 810 nm diode laser on 30 patients affected from lover limbs telangiectasia, in which the previous injection of methylene blue enabled on enhanced effectiveness with a lower fluence. The aim of this method is to set a new standard in the treatment of 0,5-3mm telangectasia, instead of sclerotherapy - at the moment considered the "gold"standard which requires many applications and is sometimes burdened from hyperpigmentation and matting. The vital stain, is injected with a 30 g. needle alter a light local infiltration anesthesia, and at the same time the vessel is irradiated with a 810 mn. laser beam ( Diomed A 400 ), with a fluente of 100 J and a pulse of 300 ms, cooling simultaneous1y the skin with anhydrous cool air (criojet). Results were good, with a nearly complete obliteration of treated telangectasia, without residual hyperpigmentation, mattingp and hypopigmentation, neither on 171-IV class phototype.Authors pointed out the advantage of this method, based on a simple thermic destruction of vessel, without the chimical endothelioangiitis typical sclerotherapy, and leading to phlogistic and pigmentary complications.The length of 810 nm. is poorly adsorbed from water and is selective for chromophores (Hb, melanine, and methylene blue), resulting less injurious for dermal tissues.The use of methylene blue, has the double role of enhancing the 810 nm. hght absorption and of colouring the vascular wall, i.e. our main target. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 244 Transdermal treatment of varicose and spider veins with vascular laser 810 nm DRES Claudio Manuel Codina , José Luis Neme Until today, the treatment of varicose and spider veins had not reach a good performance. Only in combination with sclerosants agents the transdermal laser therapy had achieved acceptable results. We present a series of 214 patients, who were treated transdermally with a vascular laser 810 nm of wavelength. A handpiece of 2 mm was used in them all the treatments were made in an ambulatory form. A total of 412 transdermal treatments were performed with an 85% of efficacy between May 2000 and February 2001. J Cosmet Laser Ther. 2003 Dec;5(3-4):154-62 Response of spider leg veins to pulsed diode laser (810 nm): a clinical, histological and remission spectroscopy study Wollina U, Konrad H, Schmidt WD, Haroske G, Astafeva LG, Fassler D BACKGROUND: Spider leg veins are common. Their treatment with laser or intensed light therapy shows generally variable success rates and often adverse side effects such as hyper- or hypopigmentation. This study was performed to investigate whether pulsed diode laser (810 nm) treatment is effective and safe. METHODS: Thirty-five female patients with spider leg veins were included in this prospective trial. They were treated twice with a pulsed diode laser (810 nm; spot size 12 mm, frequency 2-4 Hz, pulse width 60 msec, fluence 80-100 Jcm(-2)). Laser therapy was performed on day 0 and day 14. Clinical assessments were carried out before and immediately after the first laser therapy, after 2 weeks, 8 weeks, and one year. Skin biopsies were taken before and immediately after the first laser treatment, and after 10 weeks. Contact-free remittance spectroscopy was performed before laser treatment, immediately after the first treatment, after 2 weeks and 8 weeks. RESULTS: After the first treatment 15 patients showed a complete disappearance (CR) of spider leg veins; in the remaining 20 patients a remarkable improvement (RI) was noted (n=35). After six months of follow-up CR was seen in 6 patients, RI in 6, a stable situation in 9, and scar formation in 1 patient (n=21). The effect was almost completely stable during one year of follow-up. The examination of histological specimens before and after laser treatment showed no cellular inflammatory reaction. The mean vascular area was significantly reduced after the first (p<0.05) and after the second (p<0.05) laser treatment. Spectral analysis showed a marked decrease of peaks for oxygenized haemoglobin immediately after laser treatment and during the follow-up. Safety profile was excellent without purpuric reaction or pigmentary changes. Mild scarring was observed in two patients at the end of follow-up. CONCLUSIONS: Pulsed diode laser therapy (810 nm) is an effective and safe treatment option for spider leg veins. The effects can be seen immediately. Objective monitoring by non-invasive remission spectroscopy and histology of biopsy specimens demonstrates selectivity of the laser action. Lasers Med Sci. 2004;19(1):21-6. Epub 2004 Jun 24 An 810 nm diode laser in the treatment of small (< or = 1.0 mm) leg veins: a preliminary assessment Trelles MA, Allones I, Trelles O A consistently effective treatment for small leg veins (< or = 1.0 mm) is still being sought. The efficacy of an 810 nm diode laser in vein removal was assessed in a preliminary study. Fifteen females, skin types I to III, vein diameters 0.5-1 mm, aged from 25 to 42 years, participated in the study. An 810 nm diode laser (90 W, 20 ms/pulse, 10 Hz rep rate, 4.0 mm hand piece) was applied along the target veins. Biopsies were taken from two patients before and after the first treatment session. No compression was applied post-treatment. Four weeks later, a second treatment was given. Results were assessed subjectively from the patients' satisfaction index (SI) and objectively from clinical photography done by an independent clinician, who also judged the venous morphology before and 4 weeks after the second session. All patients completed the trial. Pain was moderate to severe at the time of treatment and erythema which was mild, which was seen in all 15 patients; oedema occurred in 12 patients and blistering in only one. No scarring was noticed. The overall satisfaction indices at the 4and 8-week assessments were 20.7% and 55.1%, respectively. No patient got worse. The objective evaluations at the 4- and 8-week assessments showed increasing improvement in all aspects examined. Pain at the time of treatment was a problem for all patients, so epidermal cooling should be added. Despite this, the 810 laser diode was an interesting and promising device for treatment of small leg veins, warranting further study in larger patient cohorts with a longer-term follow up. J Am Acad Dermatol. 2006 Feb;54(2):282-9 The 800-nm diode laser in the treatment of leg veins: assessment at 6 months Trelles MA, Allones I, Alvarez J, Velez M, Martin-Vazquez M, Trelles OR, Luna R, Buil C, Mordon SR BACKGROUND: The efficacy of the 800-nm diode laser system in clearing leg veins was analyzed subjectively and objectively in a variety of leg veins. METHODS: A total of 10 women (age 25-55 years, skin types II-IV) with a variety of leg vein types were treated with an 800-nm diode laser. A sequence of pulses (5-8 stacked pulses, pulse duration 50 milliseconds, delay 50 milliseconds) was applied on a 3-mm spot (210-336 J/cm2 fluence, depending on vessel size). Treatment on the same vein was performed at intervals of 2 months until complete clearance was achieved (maximum: 3 treatments). The results were assessed at 6 months from the last treatment. Patients evaluated their subjective improvement by means of a questionnaire to elicit the satisfaction index. In an independent objective assessment, the clearance index was based on the pretreatment and posttreatment clinical photography, also analyzed by a computer program. RESULTS: All patients completed the trial with mild but transient side effects. The patient 6-month assessments for very good, good, fair, poor, and worse were 1, 5, 3, 1, and 0, respectively. For the clinician-assessed clearance index, the numbers for the same grades were 2, 6, 2, 0, and 0, and for the computer assessment they were 1, 6, 2, 1, and 0. No patient scored worse in any assessment. The overall satisfaction index and clinician and computer clearance indexes were 60%, 80%, and 70%, respectively. LIMITATIONS: No control group could be obtained in this study. CONCLUSIONS: The 800-nm diode laser as used in the study may well offer an effective treatment method for leg veins that is comparatively pain and side-effect free. Best results were obtained in vessels of 3 to 4 mm in diameter located on the thigh, and in patients with phototype III skin. No correlation was seen between results and patient age. 940 nm J Am Acad Dermatol. 2003 May;48(5):768-74 The new 940-nanometer diode laser: an effective treatment for leg venulectasia Passeron T, Olivier V, Duteil L, Desruelles F, Fontas E, Ortonne JP BACKGROUND: The 940-nm diode laser has been shown to be an effective treatment for leg veins. OBJECTIVE: We sought to evaluate the effectiveness of the 940-nm diode laser on leg veins, depending on the size and morphologic aspect of the treated vessels. METHODS: A total of 60 patients (mean age: 44.4 years, Fitzpatrick skin types I-IV) underwent up to 3 treatment sessions at 4-week intervals using the 940-nm diode laser. Treatment parameters were: vessels < 0.4 mm in diameter, 0.5-mm spot, pulse duration of 10 milliseconds, fluence 306 J/cm(2); 0.4 to 0.8 mm in diameter, 1-mm spot, pulse duration of 30 milliseconds, fluence 306 J/cm(2); and 0.8 to 1.4 mm in diameter, 1.5-mm spot, pulse duration of 70 milliseconds, fluence 317 J/cm(2). Repetition rate was 2.5 Hz. Success rate was evaluated through double-blind observation. RESULTS: Only 13.33% of patients with telangiectases less than 0.4 mm in diameter had a percentage of vessel clearance superior to 75%. However, 88.24% of patients with vessels between 0.8 and 1.4 mm in diameter obtained more than 75% vessel clearance. CONCLUSION: The treatment of leg veins by the 940-nm diode laser strongly depends on the size of the target vessel. Better results were obtained with 0.8- to 1.4-mm leg venulectases. 980 nm J Cosmet Laser Ther. 2004 Dec;6(4):217-21 Treatment of vascular abnormalities with a long-pulse diode at 980 nm. Levy JL, Berwald C BACKGROUND: Lasers have been used to treat a variety of vascular abnormalities for over 20 years. For minor vascular targets, a small and friendly diode laser with cooling handpiece appears to be a challenger to other systems. OBJECTIVE: The purpose of this study was to compile treatment data and to examine the effectiveness of a longer pulse duration diode laser in the treatment of vascular pathologies such as facial telangiectasia, venous lakes, spider nevi, blue telangiectasia, leg veins and dermatological treatments. SUBJECTS AND METHODS: Thirty patients were treated with the diode laser with a pulse of 150 ms, energy densities of 300-500 J/cm(2) and wavelength at 980 nm. Patients were treated with a surface cooling device. Clinical evaluations were categorized into improvements of 0-25%, 25-50%, 50-75% and greater than 75%. RESULTS: 60% of the patients have up to 50% improvement. The maximum clearance was obtained with only one treatment. However even the cooling system is performed +5 degrees C, pain was relatively high for a majority of patients. CONCLUSIONS: The long-pulse diode laser at 980 nm is effective for treating a wide variety of small vascular abnormalities, for deep and thick vascular lesions and leg veins. The surface cooling device is useful for epidermal protection and pain-free treatment. Nd:YAG - 1064 nm Vasa Suppl 1991;33:109-10 Laser sclerosing of intracutaneous varicose veins Quellmalz U 87 patients with intracutaneous varicosities underwent a percutaneous Neodym-YAG-laser therapy. The results of 72 of them were satisfactory. Only in 2 cases complications (Hyperpigmentation, scarification) were found. The laser seems to be an additional tool in the therapy of varicosities, so small calibrated, that intravasal drug application seems to be impossible. Vasa 1998 Feb;27(1):43-5 Arteriovenous fistula after endoscopic dissection of the perforant vein of the lower leg with the neodymium:YAG laser in chronic venous stasis syndrome Folsch C, Rauber K, Langer C The endoscopic dissection of the perforating veins has been invented by Hauer in the last decade. He introduced the videoendoscopy to this surgical procedure. The avoidance of operative access through areas of trophic changes is very beneficial for reducing postoperative complications. Although postoperative thermic lesion have been reported on. Following an endoscopic laser coagulation of a Cockett perforating vein an arterio-venous fistula between the posterior tibial artery and vein developed by the mechanism mentioned. Persisting pain and the persistence of the ulcer led to several diagnostic measures including phlebography, digital subtraction angiography and CT-scan. After the fistula had been closed successfully by percutaneous embolization with four platin wires the ulcer disappeared. Ann Plast Surg 1988 Sep;21(3):223-30 The treatment of cutaneous vascular lesions with the Nd:YAG laser. Rosenfeld H, Wellisz T, Reinisch JF, Sherman R. Section of Plastic Reconstructive Surgery, University of Southern California The Nd:YAG laser is well suited for the treatment of cutaneous vascular lesions. The characteristic properties of the Nd:YAG laser emissions in tissue are a high degree of penetration with low absorption by unpigmented tissue. The result is a coagulative effect on tissue containing hemoglobin with relative skin sparing. The Nd:YAG laser was used to treat 116 patients with a variety of cutaneous vascular lesions. Good to excellent results were obtained with a low complication rate for deep cavernous and capillary lesions, port wine stains, and minor vascular ectasias above the lower extremities. Minor venous ectasias and varicosities located on the lower extremities responded poorly. The Nd:YAG laser represents an efficacious tool for the treatment of difficult vascular lesions, with the exception of venous lesions of the lower extremities. Dermatol Surg 1998 Oct;24(10):1119-23 Sclerosis and the Nd:YAG, Q-switched laser with multiple frequency for treatment of telangiectases, reticular veins, and residual pigmentation Cisneros JL, Del Rio R, Palou J BACKGROUND: The combination of low concentrations of sclerosing solution and the Nd:YAG, Q-switched laser with multiple (quadruple) frequency provides good results in the treatment of telangiectases and reticular varicose veins of the lower extremities, as well as pigmentation that may appear during sclerotherapy. OBJECTIVE: This paper is based on a series of patients with telangiectases and reticular veins who were treated with sclerotherapy and the Nd:YAG, Q-switched laser with quadruple frequency. METHODS: Patients with telangiectases and reticular veins received two or three treatment sessions with polydocanol and the Nd:YAG, Q-switched laser with quadruple frequency. Then, they were assessed a clinical score corresponding to the level of improvement achieved. Residual hematic pigmentation lesions were also eliminated with the laser. RESULTS: Excellent improvement was evident in 90% of the patients with minimal residual lesions. CONCLUSIONS: The combined technique of sclerosing solution and the Nd:YAG laser with multiple frequency is a valid alternative for the elimination of telangiectases and reticular veins of the lower limbs. This technique has several advantages, such as the use of low concentrations of sclerosing solution, high patient acceptance levels due to minimal disturbances, and the fact that local anesthesia is unnecessary. Good results are obtained without complications and minimal residual pigmentation. These mild pigmentation can be treated with the Nd:YAG laser. Dermatol Surg 1999 May;25(5):399-402 Early clinical results with a multiple synchronized pulse 1064 NM laser for leg telangiectasias and reticular veins Weiss RA, Weiss MA BACKGROUND: The 1064 nm wavelength penetrates tissue and blood vessels with little absorption by melanin. OBJECTIVE: To perform a study examining the effects of 1064 nm laser used in pulses from 4 msec to 16 msec on leg telangiectasias ranging in size from 0.5 to 3 mm. METHOD: In this initial trial, 50 sites on 30 patients were enrolled and treated with a multiple synchronized pulse laser at 1064 nm. The primary parameter utilized was a single 10-16 msec pulse. Improvement was judged by comparison of digital images at 1 month, 2 months, and 3 months posttreatment. Improvement was judged, based on size and number of vessels remaining. Side effects were noted as present or absent at each visit. RESULTS: Immediate contraction or darkening followed by urtication and visible total vessel closure as indicated by absence of blanching and visual elimination of the vessel border occurred in most of the treated sites. Two 3 mm diameter vessels were confirmed to be closed without flow by Duplex ultrasound visualization, using a 10 MHz transducer. Bruising from vessel rupture was seen in approximately 50% of the cases. No epidermal injury was noted in any sites, even in Fitzpatrick skin Types IV. At 3 months follow-up, 75% improvement was noted at treatment sites. CONCLUSIONS: Initial clinical results with a new multiple synchronized pulsed 1064 nm laser indicate that this longer wavelength supplied at pulses of up to 16 msec appears to be a valuable modality for immediate closure and subsequent elimination of leg ectatic veins. Epidermal injury is unlikely, as the near infrared wavelength has minimal interaction with melanin. Minerva Cardioangiol 2000 Oct;48(10):329-34 Treatment of deep underlying reticular veins by Nd:Yag laser and IPL source Colaiuda S, Colaiuda F, Gasparotti M BACKGROUND: The purpose of this paper is to estimate the efficacy of Nd:Yag laser and IPL combined action for the treatment of deep (up to 5 mm) and large (up to 3 mm in diameter) reticular varicosity of the lower extremity. METHODS: A group of 38 subjects (2 male and 36 female) aged from 34 to 65 years were treated for deep reticular varicosity of the legs. All patients underwent various clinical analyses in order to evaluate and exclude pre-existing cardiovascular pathology, coagulation disorders as well as pathology due to saphena incontinence. Also, for the first three months they underwent ambulatory specialistic treatments at 21-days intertreatment interval. RESULTS: A reduction of venous network of 80-90% after 2 treatment sessions with Nd:Yag laser was obtained in 84% of subjects. Successive 3 treatment sessions with IPL have achieved complete vanishing of the treated venous network in 36 patients (95%). CONCLUSIONS: A combined action of Nd:Yag laser and IPL has demonstrated its particular efficacy in non-invasive treatment of deep and extensive reticolar varicosity of the lower extremity, considering also that it is well tolerated by patients and applicable in each single case on out patient basis. Dermatol Surg 2001 Apr;27(4):355-7 Generalized essential telangiectasia successfully treated with high-energy, long-pulse, frequency-doubled Nd:YAG laser. Gambichler T, Avermaete A, Wilmert M, Altmeyer P, Hoffmann K. BACKGROUND: Generalized essential telangiectasia is a rare cutaneous disorder with limited therapeutic options. OBJECTIVE: To evaluate the treatment with high-energy, high-frequency, long-pulse Nd:YAG laser in a patient with generalized essential telangiectasia. METHODS: A 62-year-old woman presented with a 20-year history of generalized essential telangiectasia. She had extensive telangiectasias primarily on the forearms and lower legs. The patient was treated with an Nd:YAG laser using a fluence of 20 J/cm2 and a pulse width of 20 msec. A sapphire water-cooled chill tip was used to cool the skin during laser therapy. The treatment was performed every 4 weeks over a period of 6 months. RESULTS: After six treatment sessions an almost complete clearance of telangiectatic lesions was observed. Side effects such as purpura, scarring, and pain did not occur. After a follow-up of 6 months, small telangiectatic lesions relapsed. CONCLUSION: Our results suggest that the Nd:YAG laser appears to be an effective and safe treatment option for generalized essential telangiectasia. Dermatol Surg 2001 Apr;27(4):365-9 Long-term results with a multiple synchronized-pulse 1064 nm Nd:YAG laser for the treatment of leg venulectasias and reticular veins Sadick NS BACKGROUND: The long-pulsed Nd:YAG (1064 nm) laser has been shown to be effective in the treatment of blue venulectasias and reticular veins. OBJECTIVE: The present study examined the clinical efficacy and long-term follow-up (12 months) of patients treated with the 1064 nm Nd:YAG laser technology. METHODS: Twenty-five female patients (mean age 37.6 years, Fitzpatrick skin types II-V) were treated with up to three treatment sessions at 6-week intervals on a 5 cm2 surface area of vessels utilizing the 1064 nm Nd:YAG laser with a circulating cooling device. Treatment parameters were vessel size 0.2-2.0 mm treated with a double pulse of 7 msec at 120 J/cm2 and vessel size 2.0-4.0 mm treated with a single pulse of 14 msec, fluence 130 J/cm2, with a spot size of 6 mm. Improvement was judged by double-blinded observer evaluation, macrophotographic imaging, optical chromatography, and a patient evaluation scale. RESULTS: Sixty-four percent of patients treated in the present study achieved 75% or greater clearing of vessels after a maximum of three treatment sessions. Optical chromatography revealed statistically significant decreased chromophore intensity (mean blueness reduction index of 41.2b-). Sixty-four percent of patients were greatly satisfied with the results of the laser treatment. Two patients manifested vessel recurrence when examined at 6 and 12 months, respectively. CONCLUSION: The 1064 nm Nd:YAG laser can produce effective long-term photosclerosis of blue venulectasia and reticular veins. The potential for recurrence should be recognized by the vascular laser surgeon. Arch Dermatol 2001 May;137(5):613-7 Clinical and pathophysiologic correlates of 1064-nm Nd:Yag laser treatment of reticular veins and venulectasias Sadick NS, Prieto VG, Shea CR, Nicholson J, McCaffrey T BACKGROUND: The goal of sclerotherapy, laser therapy, and intense pulsed-light therapy is to produce long-term, cosmetically significant elimination of disfiguring leg veins. This study examines the histologic and clinical effects of using a 1064-nm Nd:YAG laser system on lower extremity vessels. DESIGN: A single treatment using the following parameters: wavelength, 1064 nm (multiple synchronized pulsing); spot size, 6 mm; pulse duration, 14 milliseconds (single pulse); and fluence, 130 J/cm(2). SETTING: Private dermatology practice. PATIENTS: Thirteen women (mean age, 38.5 years) with blue venulectasia, 0.5 to 1.5 mm in diameter (class 2), and reticular veins, 1.5 to 3.0 mm in diameter (class 3), on the thighs. MAIN OUTCOME MEASURES: Examination of treated and untreated areas by 2 masked observers using macrophotography (1, 2, 3, and 6 months after treatment), Doppler, and optical chromatographic changes. Findings from three 2-mm punch biopsies from treated (immediately and 4 weeks after treatment) and untreated sites. Routine histologic examination; special stains (for elastic and connective tissue and for mucopolysaccharides); and immunohistochemical analysis for expression of the heat shock protein hsp70, tie2 (an endothelial cell-specific receptor tyrosine kinase), and transforming growth factors beta1 and beta2. RESULTS: Eight patients (62%) manifested 75% to 100% clearing of treated vessel surface area. Treated areas revealed perivascular hemorrhage, thrombi, fragmentation and homogenization of elastic fibers, and eosinophilia of vessel walls. Expression of hsp70 and transforming growth factor beta was increased in treated vessels. CONCLUSIONS: Our data confirm the effectiveness of 1064-nm Nd:YAG laser treatment in clearing dilated lower extremity veins, probably by heat-induced vessel damage and subsequent fibrosis. Maintenance of clearing was achieved for up to 6 months. However, the presence of recanalized thrombi in some of the specimens suggests the potential for long-term vessel reappearance. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 242 Three year results with the long pulser Nd:YAG Laser for leg telangiectasias RA Weiss, MA Weiss We have utilized an Nd:YAG 1064nm laser (VasculightTU, ESC/Sharplan, Norwood, MA) with puise durations of up to 40 millisec on leg telangiectasias up to 3mm for over three years. Over 350 patients have been treated, with an average of 3 sites per patient. The average size of telangiectasias treated is 0.8 mm (0.3mm - 3mm). Fluences have ranged from 110 -150 J/cm2. Improvement was judged by comparison of digital images (640x480, 16M colors) at one month, one year and three years post treatment Five categories of improvement based on size and number of vessels remaining were assigned at three year post treatment. Results demonstrated an average of 2.38 treatments were required for patients to note satisfactory improvement, which numerically rated a 3.25 (approximately 75% improvement) by photographic evaluation. Side effects included hyperpigmentation (16%) which appeared very similar to post-sclerotherapy hyperpigmentation and resolved in 95% at the 6 month follow up. Telangiectatic matting was noted in 4%. Minor epidermal injury was noted in only one treatment site. At three years follow up, the long pulsed millisecond domain 1064nm laser remains an effective modality for destruction and subsequent clearance of leg telangiectasias with efficacy and side effects comparable to other methods. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 242 Treatment of leg telangectasias with a 1064 nm long pulse Nd:YAG Laser; a comparative study Leyda Bowes, M.D. and Mitchel P. Goldman, M.D. A subset of leg telangiectasias occur which appear to be recalicitrant to sclerotherapy treatment and/or arise as a result of sclerotherapy treatment (telangiectaic matting). Lasers are therefore useful in treating these two classes of vessels. 50 telangiectatic areas on 40 patients with bilaterally symmetrical telangiectasias without obvious evidence of feeding reticular veins were treated with either the CoolTouch Varia or CoolGlide 1064nm long pulse Nd:YAG lasers. Individual telangiectatic vessels were treated with multiple passes until thermocoagulation and/ or vasospasm occurred. Areas were treated once monthly fora total of three treatments. Preliminary results show that both.lasers perform nearly identically in causing a resolution of telangiectasias in greater than 90% of lesions. An average of two treatments are required in order to effect maximal resolution. The authors define acceptable resolution as greater Chan 90%. Pulse duration, spot size, and fluence were identical for the two lasers. The only variable was the method of cooling, The CoolTouch Varia provides a dynamic spray-cooling method. The CoolGlide laser provides a contact cooling method. Patients tended to prefer the CoolToûch Varia dynamic cooling system as it caused less pain. The use of lasers in treating leg telangiectasias has utility in a subset of patients. The 1064 long pulse Nd:YAG lasers appear to be highly efficacious in finis regard. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 241 Validation study of the sclero-therapy in saphenic vein system insufficiency treated with Nd:YAG laser and IPL. Preliminary data on a selected group of patients S. Venosi*, M. Benedetti Valentine*, F. Intrieri*, R. De Vita**, S. Colaiuda**, M. Diana** Nowadays the use of the laser in the vascular field has found wide application in the treatment of cutaneous anaesthetisms (teleangectasys). The new technologies introduced with the Nd: Yag laser and IPL can extend the method in vascular pathologies of the venous system, allowing the correction of flow alterations in ectasies and/or in varicose veins of the saphenic veins and their tributary system. In a group of 374 patients treated for vascular anaesthetism of the lower limbs, we selected 18 patients (Males=6, Females=12, average age 31 years, range 16-68), with a chronic venous insufficiency syndrome (progressive worsening towards varicose vein and with echo-color Döppler suggestive of venous valve incompetence. All patients were treated with Nd: Yag laser and IPL, with a monthly frequency of max. four applications. Immediately before the laser session, an venous mapping was carried out. Five patients were checked with two echo-color Döppler two weeks after the first laser session , while 13 patients were checked two weeks after the second laser session. All patients were checked with echo-color Döppler 30, 60 and 180 days after the last laser session. In two patients the ultrasound controls were compared with MR phlebography. At the end of the treatment it was possible to show the stabilized obstruction of the treated venous segments: 4 patients underwent 3 sessions, the remaining patients received the complete course of treatment. Two patients who in the final echo-color Döppler showed an enlargement of the tributary vessels, underwent a fifth session of treatment in order to achieve the extension of the sclerosis and its stabilization. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 244 Laser in phlebology Prof.Roberto Simkin The author presents his experience with a new Laser yag of 1064 nm which is indicates in the treatment of the telangiectasies and reticular veins. The modern equipment gives -off, a directional light that photocoagulates the varicose veins immediately, and sometime making them disappear instantaneously. The treatment is indicated in the tree types of telangiectasies, red ,blue. and violet. The results in each types of pathology is different this is why it is necessary to graduate the laser waves in each cases. In the cases of reticular veins the results are very good, leaving in many cases, a red violet area that later disappear along with the veins. The complications observed with this kind of laser are burns and hyperpigmentation, bruising, which disappear in time, although many complications may last a year. The author obtained satisfactory results in 75% of the cases. In the remaining 25% the treatment had to be completed with scleroterapy. The association of laser and scleroterapy is the best choice. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 245 Results of the Nd:YAG in the treatment of telangectasia and reticular leg veins Dr. Hilario Robiedo MD, PhD, F ACS The visible veins in the Iegs are a frequent cosmetic problem whose treatment continues being a challenge for the surgeons that try this sort of pathology. The most important initiallv, it is the effective treatment of the venous hypertension witch is present in 85% of the patients that present venulectasia and telangiectasia in their limbs. The slerotherapy has been the standard treatment, but most of the minor vessels of 1 diameter millimeter are difficult of injecting and eradicating in only one treatment. The side effects of the sclerotherapy include changes in the pigmentation, ulceration of the skin, scars apparition and matting post sclerotherapy. Most of the telangiectasias in the legs vary from l mm to several diameter millimeters. In this study we.are presenting the results obtained in a series from patients treated through Nd:YAG (CoolGlide-Altus Médical), in those which has been solved previously their venous hypertension through sclerotherapy (sodium tetradecyl sulfate) with or without ligature interruption of greater saphenous vein and its tributaries, depending if in the findings obtained with previous duplex ultrasound. The GSV was incompetent (reflux or valve insufficiency) or not. Currently we are accomplishing prospective studies for the treatment of greater calibre veins (greater than 3 mm of' diameter) through vascular specific. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 336 Efficiency of the Nd:YAG laser in the treatment of leg veins Hilario Robledo , Phd, FACS The use of the different lasers as a rnedical instrument is an evolutionary process of continuous technical refinement and fundamentally based on the understanding of the laser-tissue interactions. The understanding these interactions is much more important that anyone of the laser devices that is going away to use. The capacity to obtain the wished therapeutic effect with a laser depend on the good selection of the intrinsic parameters of the laser like the density, wavelength of energy, irradiance, size of spot and width of pulse. The continuous evolution in this field will provide better results and will increase the possibility of treating other many pathologies. At the moment the use of the lasers is essential for a great number of clinical applications and we think that it would have to be integrated in the, medical and fundamentally surgical and essential learning for those clinical ones that they handle these instruments. For years they have been devised several laser systems to try vascular lesions, we have wanted to make the classification by their wavelength, these are: 1. 420nm: Argon. 2. 532mn: KTP, 3. 585-600 nrn: Dye laser, 4. 804-810nm: diode laser, 5. 1064nm: Nd:YAG laser, 6. Other devices not laser of not coherent light. Each one of these systems, depending on their wavelength, have an affinity most or less labeled by the haemoglobin, specific cromophore that in the case of the vascular lesions is the one which interests us that be absorbed the light issued by the laser to cause the wished effects specific destruction of the whole vessel without lesion of the adjacent tissue and with the smaller possibility of causing described side effects previously. J Cosmet Laser Ther 2001 Sep;3(3):147-53 Treatment of leg and face veins with a cryogen spray variable pulse width 1064-nm Nd:YAG laser--a prospective study of 47 patients Eremia S, Li CY OBJECTIVE: Throughout the 1990s laser treatment of leg veins has been a challenge. Newer, longer wavelength lasers capable of delivering high fluences with larger spot sizes, with variable pulse width have shown promising preliminary results. Experience with these lasers for the treatment of facial telangiectasia and periorbital reticular veins is even more scant. To the authors' knowledge this is the first prospective study to evaluate a variable pulse width, cryogen spray-equipped 1064-nm Nd:YAG laser for the treatment of both leg and face veins, including larger periorbital reticular veins. METHODS: A total of 47 volunteers aged 32-67 years (30 skin type I-V with leg telangiectasia and reticular veins, and 17 skin type I-IV with face telangiectasia and reticular periorbital veins) were treated with the Nd:YAG laser. For leg vein patients, two to three sets of different leg veins were treated with a maximum of three treatments. Patients were examined 1 week after each treatment and at 1, 2, and 3 months after the last treatment. All face vein patients received one treatment and were examined at 1 month post treatment. Treatment parameters for both leg and face veins varied with the size of vessels being treated. Pre and post treatment 35-mm photographs were taken. Improvement was judged by two experienced physicians both visually on patients and by comparison of pre and post treatment photos. Results were graded as percentage resolution, in five groups: 0%, 0-25%, 25-50%, 50-75% and 75-100%. RESULTS: In all, 23 of 30 patients completed the leg vein segment of the study. A total of 41 leg vein sites were treated. Greater than 75% improvement was observed at 85% of the treated sites; greater than 50% improvement was observed at 95% of the treated sites; less than 25% improvement was observed at 5% of the treated sites. In all, 17 of 17 patients completed the face vein segment of the study. A total of 32 sites were treated (24 on cheeks, nose, and chin telangiectasia and eight periorbital reticular veins). Greater than 75% improvement was observed at 97% of the treated sites; greater than 50% improvement was observed at 100% of the treated sites. Notably, 100% of the facial reticular veins treated had essentially 100% resolution. Pain during treatment was variably perceived by patients, but occasionally was sufficient for patients to decline further treatment. Transient hemosiderin pigmentation, as seen with sclerotherapy, was common with larger vessels. CONCLUSION: The cryogen spray-equipped 1064-nm Nd:YAG laser was remarkably effective and safe for skin type I-V patients. Excellent results for leg veins, approaching sclerotherapy outcomes, were obtained for both 0.3-1.5-mm telangiectasia and larger 1.5-3-mm reticular veins. Furthermore, this laser is also an outstanding tool for treatment of facial telangiectasia with little if any risk of purpura. For the first time it appears that there is a safe and effective treatment for 1-2-mm periorbital reticular veins. However, the use of topical anesthesia may be needed for some patients. J Eur Acad Dermatol Venereol 2001 Nov;15(6):559-65 Nd:YAG 1064 nm laser in the treatment of facial and leg telangiectasias Major A, Brazzini B, Campolmi P, Bonan P, Mavilia L, Ghersetich I, Hercogova J, Lottit T BACKGROUND: Facial and leg telangiectasias are a frequent cosmetic concern for both females and males with various skin types and ages. To date the different treatments for these problems, in particular leg telangiectasias, have frequently failed or led to negative side-effects. OBJECTIVE: This study examines the clinical effects and safety of applications with a 1064-nm Nd:YAG laser system (SmartEpil II, DEKA M.e.l.a., Florence, Italy) to treat vessels on the face and legs. MATERIALS AND METHODS: Twenty-five subjects with facial telangiectasias underwent one treatment at 100 J/cm2, 10 ms and 2 Hz repetition rate. Thirty-two subjects with leg telangiectasias, measuring 0.1-3 mm in diameter, were treated at 125-200 J/cm2, 10-30 ms and 2 Hz repetition rate. Subjects in this group underwent one to five treatment sessions at 8 week intervals. RESULTS: All subjects showed visible improvement, with 95-100% clearing of the face telangiectasias after only one treatment, and 50-100% clearing of the lower extremity vessels after three to five treatments. Transitory hypopigmentation was seen in two cases subjected to leg vessel treatment. CONCLUSIONS: Treatment of facial and leg telangectasias using a true long pulse 1064 nm Nd:YAG laser is an effective and safe method. The relative lack of discomfort combined with a high degree of individual satisfaction should play a part in the fairly high level of acceptance of this new form of therapy for the treatment of leg and face telangiectasias. J Am Acad Dermatol 2002 Jan;46(1):66-72 A dual wavelength approach for laser/intense pulsed light source treatment of lower extremity veins Sadick NS BACKGROUND: Consistent reproducible aesthetic results are a desired component of laser/intense pulsed light (IPL) treatment of lower extremity blood vessels. In this regard, shorter wavelengths may be used to treat fine red telangiectases, whereas longer wavelengths may be used to treat larger diameter blue venulectasia and small reticular veins. OBJECTIVE: The purpose of the present study was to demonstrate that a bimodal wavelength approach to laser/IPL source treatment for lower extremity vessels up to 8 mm in diameter produces results superior to previously described photothermolytic approaches for eradication of unwanted lower extremity blood vessels. METHODS: Fifty female patients (mean age, 37 years) were treated in a private practice setting with class I-III red telangiectasia, blue venulectasia, and reticular veins (0.1-4.0 mm in diameter) on the inner or outer thighs. A combined approach of laser/IPL treatment was used; patients had up to 3 treatments at 6-week intervals on a 5-cm2 surface area of vessels with the use of an IPL source wavelength of 550 nm, fluence of 40 J/cm2, for treatment of red telangiectases less than 1 mm in diameter, while a 1064-nm Nd:YAG laser at a fluence of 140 J/cm2 was used to treat venulectases and reticular vessels that were 1.0 to 4.0 mm in diameter. Results were analyzed by macrophotographic imaging, double-blinded observer evaluation, optical chromatography, and a patient evaluation scale. RESULTS: An average of 2(1/2) patient sessions produced significant clearing (75%-100%) in 80% of patients. The mean erythema index showed significant lightening (35.3+dl) in the study population. Finally, 76% of patients reported great satisfaction with the treatment results. CONCLUSION: A bimodal wavelength approach utilizing both short and long wavelengths produces significant clearing of the variably colored, multiple-diameter/depth array of vessels, which commonly presents a therapeutic challenge to the vascular laser surgeon. Dermatol Clin 2002 Jan;20(1):19-36 Laser surgery of leg veins Weiss RA, Dover JS The use of lasers and light sources in treating lower-extremity blood vessels has not been as successful as they are for treatment of facial telangiectasia. Several reasons for this lack of success include increased hydrostatic pressure on the lower extremities and the anatomy of lower-extremity blood vessels. These vessels are in a deeper location, have thick surrounding adventitial tissue, and have increased basal lamina when compared with facial telangiectasia. Improvements in matching pulse duration to vessel size, use of more penetrating, longer wavelengths, and the addition of sophisticated cooling methods have improved the results with leg veins during the past 2 years. Further refinements in laser technology over the next few years will probably enhance treatment efficacy of lower-extremity telangiectasias. Lasers Surg Med 2002;30(2):154-9 Comparative pilot study evaluating the treatment of leg veins with a long pulse ND:YAG laser and sclerotherapy Coles CM, Werner RS, Zelickson BD Background and Objective To date there have been very few side by side comparison studies of laser versus sclerotherapy in treating small leg veins. This study compares a long pulsed Nd:YAG laser with contact cooling to sclerotherapy for treating small diameter leg veins by evaluating objective and subjective clinical effects. Study Design/Materials and Methods Twenty patients were selected with leg veins ranging from 0.25 to 3 mm at two comparable sites. One site was treated with long pulsed Nd:YAG laser and the other received sotradecol sclerotherapy. The patients followed up at 8 weeks for another possible laser retreatment and 3 months following the last treatment. Photographs were taken pre- and post-operatively and at each follow-up visit and used for objective comparative analysis. The patients also completed a Quality of Life survey. RESULTS: Improvement was tabulated from the photographic assessment on an improvement scale from 0 (no change)--4 (greater than 75% clearing). The laser treated areas averaged 2.50 and sclerotherapy treated sites averaged 2.30. Patient surveys show 35% preferred laser and 45% choose sclerotherapy. CONCLUSION: This pilot study demonstrates that the Lyra Long Pulse Nd:YAG laser can yield results similar to sclerotherapy in the treatment of small leg veins. Copyright 2002 Wiley-Liss, Inc. Dermatol Surg 2002 Mar;28(3):220-3 Nd:YAG Laser (1064 nm) Irradiation for Lower Extremity Telangiectases and Small Reticular Veins: Efficacy as Measured by Vessel Color and Size Rogachefsky AS, Silapunt S, Goldberg DJ BACKGROUND: Laser treatment of lower extremity telangiectases and small reticular veins has remained difficult because of vessel color, diameter, depth, and associated high-pressure flow. Traditionally, larger-caliber blue leg veins do not respond well to laser treatment. Nd:YAG laser (1064 nm) irradiation is absorbed by oxyhemoglobin and reduced hemoblogin and is associated with greater depth of penetration than other previously studied vascular lasers. OBJECTIVE: Toevaluate a millisecond contact-cooled 1064 nm Nd:YAG laser for the treatment oftelangiectases and small reticular veins. METHODS: Twenty-one lower extremitysites, with Fitzpatrick skin types I-IV, received two laser treatments separatedby a 4 to 6-week period. Blue and red vessels, ranging in size from 0.25 to 4.0mm were treated. Pulse durations of 10-50 msec were utilized at fluences of 90-187 J/cm2. Three months after the last treatment, patients were evaluated for vessel improvement and complications. RESULTS: Seventy-one percent of lowerextremity vessels had improvement graded as significant. All vessel colors andsizes were successfully treated. The only complication at 3 months waspostinflammatory hyperpigmentation. CONCLUSION: 1064 nm Nd:YAG laser irradiation with associated contact cooling is a safe and effective treatment for telangiectases and small reticular veins of the lower extremities. Dermatol Surg 2002 Mar;28(3):224-30 A Side-by-Side Comparative Study of 1064 nm Nd:YAG, 810 nm Diode and 755 nm Alexandrite Lasers for Treatment of 0.3-3 mm Leg Veins Eremia S, Li C, Umar SH BACKGROUND: Laser and intense pulsed light device treatments of leg veins have generally yielded disappointing results. Use of longer wavelengths, longer pulse widths, and better cooling devices have recently sparked renewed interests in these methods.OBJECTIVE: To prospectively compare, side by side, a 3-msec cryogen spray-equipped 755 nm alexandrite, a sapphire window cooled super-long-pulse 810 nm diode, and a variable pulse width, cryogen spray-equipped 1064 nm Nd:YAG laser for the treatment of 0.3-3mm leg veins.METHODS: Thirty female volunteers, skin types I-V, age 32-67 years with comparable sets of leg veins were treated with the Nd:YAG laser and either the diode laser, alexandrite laser, or both. In most patients two to three sets of comparable sites were treated. Treatment parameters varied with each laser and according to the size of veins being treated. Patients were examined 1 week after each treatment and at 1, 2, and 3 months after the last treatment. Preand posttreatment 35mm photographs were taken. Improvement was judged by two experienced physicians both visually on patients and by comparison of pre- and posttreatment photographs. Results were graded as percent resolution, in five groups, 0%, 0-25%, 25-50%, 50-75%, and 75-100%.RESULTS: In the 22 patients completing the study, 36 leg vein sites were treated with the Nd:YAG laser, 18 leg vein sites were treated with the diode laser, and 12 leg vein sites were treated with the alexandrite laser. Greater than 75% improvement was observed at 88% of the Nd:YAG laser-treated sites, 29% of the diode laser-treated sites, and 33% of the alexandrite laser-treated sites. Greater than 50% improvement was observed at 94% of the Nd:YAG laser-treated sites, 33% of the diode laser-treated sites, and 58% of the alexandrite laser-treated sites. Less than 25% improvement was observed at 6% of the Nd:YAG laser-treated sites, 39% of the diode laser-treated sites, and 33% of the alexandrite laser-treated sites. Pain during treatment was variably perceived by patients, but occasionally sufficient for patients to decline further treatment. Posttreatment purpura and telangiectatic matting were a significant drawback for the alexandrite laser. Transient hemosiderin pigmentation, as seen with sclerotherapy, was common with larger vessels.CONCLUSION: The cryogen spray-equipped 1064 nm Nd:YAG laser was remarkably effective and safe for the treatment of 0.3-3 mm leg veins. The use of topical anesthesia may be needed for some patients. The super-long-pulse 810 nm diode laser gave unpredictable results. Additional refinements of fluence and pulse width could improve its performance. The 3-msec, 755 nm alexandrite laser at fluences of 60-70 J/cm2 and an 8 mm spot can be effective, but inflammatory response, purpura, and matting limit its usefulness. Longer pulse widths might decrease these problems. For leg vein treatment, the 1064 nm wavelength is very safe for type V skin, the 810 nm wavelength at super-long pulse widths of 400-1000 msec is very safe for type IV and marginal for type V skin, and the 755 nm wavelength is limited to nontanned type I-III skin. Dermatol Surg 2002 Mar;28(3):244-7 Treatment of Face Veins with a Cryogen Spray Variable Pulse Width 1064 nm Nd:YAG Laser: A Prospective Study of 17 Patients Eremia S, Li CY BACKGROUND: Through the 1990s laser treatment of leg veins has been a challenge. Newer, longer wavelength lasers with variable pulse width have shown promising results for both telangiectasia and reticular leg veins. Experience with these lasers for treatment of facial telangiectasia and periorbital reticular veins is scant.OBJECTIVE: To our knowledge this is the first prospective study to evaluate a variable pulse width, cryogen spray-equipped 1064 nm Nd:YAG laser for the treatment of facial telangiectasia and larger periorbital reticular veins.METHODS: Seventeen volunteers, ages 32-67 years, skin types I-IV, with facial telangiectasia and reticular periorbital/temporal veins were treated once with the Nd:YAG laser at fluences of 125-150 J/cm2 with a 6 mm spot size and pulse widths of 25 msec for small vessels and 75-100 msec for reticular veins. Patients were examined 1 week and 1 month after the treatment. Pre- and posttreatment 35mm photographs were taken. Improvement was judged by two experienced physicians, both visually on patients and by comparison of pre- and posttreatment photographs. Results were graded as percent resolution, in five groups: 0%, 0-25%, 25-50%, 50-75%, and 75-100%.RESULTS: All 17 patients completed the study. Thirty-two sites were treated (24 cheek, nose, and chin telangiectases, and 8 periorbital reticular veins). Greater than 75% improvement was observed in 97% of the treated sites. Greater than 50% improvement was observed in 100% of the treated sites. Notably, 100% of the facial reticular veins treated have essentially 100% resolution. Pain during treatment was variably perceived by patients, but occasionally sufficient for patients to express reservations about additional future treatment. Transient erythema and edema were common, but fine crusting was rare. Small areas of purpura were also quite rare.CONCLUSION: The cryogen spray-equipped 1064 nm Nd:YAG laser was remarkably effective and safe for skin type I-IV patients. It is an excellent tool for treatment of facial telangiectasia with minimal risk of purpura. For the first time we appear to have a simple, safe, and effective treatment for 1-2 mm periorbital reticular veins. The use of topical anesthesia may be needed for some patients. Phlébologie 2002, 55 (3) : 217-22 Lasers en phlébologie : prise en main, premières impressions cliniques et hémodynamiques du laser Nd :YAG (1064 nm) Lyra TM Emsallem J; Yidal-Michel JP, Porcher R La technologie des lasers vasculaires permet actuellement d'étendre leur champ d'application aux varices de plus grand diamètre et de plus grande profondeur grâce à l'association de nouvelles longueurs d'ondes pénétrantes et de procédés de refroidissement cutanés limitant leurs effets thermiques. Parmi ces longueurs d'ondes, la bande YAG 1064 nm (Lyra Nd-YAG) a démontré son efficacité dans la sclérose des varices et varicosités des membres inférieurs. Sur une étude portant sur 518 cas, pendant une période de 10 mois, les auteurs ont cherché à valider cette nouvelle technique, en déterminant les paramètres (puissance, fluence, durée d'impulsion, fréquence d'impulsions, couleur, profondeur et diamètre de la varice) utiles pour optimiser les résultats, atteindre des profondeurs et diamètres de varices accrus et limiter les effets secondaires. Globalement, les suites avec le laser Lyra Nd-YAG 1064 nm sont simples et les complications mineures et réversibles. Enfin ils ont pu montrer que les résultats du laser de haute énergie sont, dans des mains entraînées, assez superposables à ceux de la sclérose chimique et même de la phlébectomie des varices jusqu'à 3 mm de diamètre et 2,5 mm de profondeur. Dermatol Surg. 2002 Aug;28(8):694-7 Clinical comparison of sclerotherapy versus long-pulsed Nd:YAG laser treatment for lower extremity telangiectases Lupton JR, Alster TS, Romero P BACKGROUND: Sclerotherapy has traditionally been considered the gold standard of treatment for leg veins, but patient fear of multiple needle injections and side effects of treatment have fueled investigation into other treatment alternatives. As a result, vascular-specific laser and light sources have been developed in an effort to treat these vessels with minimal morbidity and improved efficacy. OBJECTIVE: To compare the clinical efficacy of leg telangiectasia treatment with sodium tetradecyl sulfate sclerotherapy to long-pulsed 1064 nm Nd:YAG laser irradiation. METHODS: A series of 20 patients with size-matched superficial telangiectases of the lower extremities were randomly assigned to receive two consecutive monthly treatments with injectable sodium tetradecyl sulfate on one leg and long-pulsed 1064 nm Nd:YAG laser irradiation on the other. Patients were evaluated by two masked assessors at each treatment visit and at 1 and 3 months after treatment to assess clinical improvement within matched sites. RESULTS: Leg telangiectases responded best to sclerotherapy in fewer treatment sessions than to long-pulsed 1064 nm Nd:YAG laser irradiation. The incidence of adverse sequelae was minimal and equivocal in both treatment groups. CONCLUSION: Despite recent advances in laser technology for treatment of lower extremity telangiectases, sclerotherapy continues to offer superior clinical effect in the majority of cases. Laser leg vein treatment appears to be most beneficial in patients with telangiectatic matting, needle phobia, or sclerosant allergy. J Am Acad Dermatol. 2003 Jan;48(1):76-81 Treatment of reticular leg veins with a 1064 nm long-pulsed Nd:YAG laser Omura NE, Dover JS, Arndt KA, Kauvar AN BACKGROUND: Millisecond-pulsed Nd:YAG lasers have been developed for the treatment of reticular leg veins. OBJECTIVE: We evaluated the effectiveness of a single treatment with a 50 millisecond 1064 nm Nd:YAG laser in the treatment of reticular veins of the lower extremity. METHODS: Twenty patients with reticular veins measuring 1.0 to 3.0 mm in diameter received one treatment with a 1064 nm Nd:YAG laser (Coolglide, Altus, Burlingame, Calif) at fluences of 100 J/cm(2) and 50 millisecond pulse duration. Symmetric matched areas that were left untreated served as the control. Eleven patients were pretreated with a topical anesthetic cream for 1 hour before treatment and wore compression stockings for 5 days after treatment. Nine patients were treated without topical anesthesia and did not wear compression stockings. Percent clearing and side effects were determined by 3 nontreating physicians (at each respective site) comparing projected Kodachrome images 1 month and 3 months after treatment. Patients also performed a self-assessment of their results. RESULTS: Two-thirds of vessels measuring 1 to 3 mm in diameter cleared more than 75% with one treatment. Larger vessels appeared to improve more than smaller vessels. Immediate treatment discomfort was tolerable. Side effects were minimal and included superficial thrombosis, delayed bruising, hyperpigmentation, and matting. CONCLUSION: Millisecond-pulsed Nd:YAG lasers used with 50 millisecond pulses are effective in the treatment of reticular leg veins. Am J Clin Dermatol. 2003;4(8):545-54 Laser and intense pulsed light therapy for the esthetic treatment of lower extremity veins Sadick NS The role of lasers and intense pulsed light sources has gained increasing popularity over the last decade. Major advances associated with improved results are the main reasons associated with this increasing popularity. These advances include epidermal cooling technologies, variable spot sizes and pulse durations as well as the ability to deliver high-energy fluences. These advances have allowed the delivery of sufficient energy to cause uniform pan-endothelial necrosis without affecting epidermal structures causing adverse sequelae such as post-inflammatory hyperpigmentation and epidermal surface irregularities. The advent of extended-pulse longer-wavelength technologies such as the 1064 Neodymium : Yttrium Aluminum Garnet (Nd : YAG) laser have allowed the treatment of individuals with darker phenotypic skin types as well as deep blue reticular veins up to 3mm in diameter in a monomodal fashion. Combined approaches of sclerotherapy plus laser treatments performed at the same treatment session may produce synergistic results in selected individuals. Lasers Surg Med. 2003; 32 (2): 160 -70. Using a "non uniform pulse sequence" can improve selective coagulation with a Nd:YAG laser (1.06 microm) thanks to Met-hemoglobin absorption: a clinical study on blue leg veins Mordon S, Brisot D, Fournier N BACKGROUND AND OBJECTIVES: Evaluation of the efficacy, on 1-2 mm blue leg telangiectasia, of a 1,064 nm Nd:YAG laser emitting in a non uniform pulse sequence calculated to consider Met-Hb formation during laser irradiation of a blood vessel. MATERIALS AND METHODS: A 1,064 nm Nd:YAG laser (Quantel Medical, Athos, France) was used in a non uniform pulse sequence mode, fluences: 300-360 J/cm(2) spot: 2 mm, + 5 degrees C contact cooling. The clinical evaluation was performed on 11 female patients, average age: 43 (25-57) years, phototype I-VI. All subjects were previously examined with Doppler ultrasound. A treatment site (6 x 4 cm) was selected on each patient. The topography of the vessels network was reported on a tracing plastic frame before each session and 6 weeks after the last one. These frames were digitized and the number of vessels was determined using the Digitized Tracing Frames Technique. Side effects were noted before and after every treatment, and 6 weeks after the last one. This study lasted for 10 months. RESULTS AND DISCUSSIONS: Patients tolerated the procedure without anesthesia. Moderate pain, transient erythema and edema, one hyperpigmentation and one matting were noted. There was no hypopigmentation. 55% (P < 0.002) vessels clearance after one session, 86% after two sessions (P < 0.001), and 98% (P < 0.001) after three sessions were obtained. On two patients, the treatment was completed after two sessions with a full clearance. Data reported in this study were obtained thanks to a computerized calculation of vessels clearance. They are similar or superior to those reported in the literature about 1,064 nm Nd:YAG lasers and leg telangiectasia. CONCLUSIONS: Since, it was developed to consider the modification of blood absorption and the methemoglobin formation which leads to an increase of the 1.06 microm wavelength absorption, the non uniform pulse mode emphasizes the efficacy of this 1,064 nm Nd:YAG laser concerning the treatment of blue leg veins telangiectasia between 1 and 2 mm. This mode gives the possibility to deliver high energy while preserving the surrounding tissue and leads to a rapid vessel clearance with reduced pain and few side effects when compared to previously published clinical studies using a 1.06 microm laser. Lasers Surg Med. 2004; 34(3): 273-6 Comparison and sequential study of long pulsed Nd:YAG 1,064 nm laser and sclerotherapy in leg telangiectasias treatment Levy JL, Elbahr C, Jouve E, Mordon S BACKGROUND AND OBJECTIVES: Millisecond pulsed 1,064 nm Nd:YAG lasers have been developed for the treatment of leg telangiectasias. To date there have been very few side by side comparison studies of laser versus the gold standard sclerotherapy in treating small leg veins. This study aims to compare a long pulsed Nd:YAG laser with contact cooling to sclerotherapy for treating small diameter leg telangiectasias by evaluating objective and subjective clinical effects. STUDY DESIGN/PATIENTS AND METHODS: Fourteen patients were selected with leg telangiectasias ranging from 0.5 to 2 mm at four comparable sites. One site was treated with long pulsed Nd:YAG alone, the second received sclerotherapy alone, the third laser then sclerotherapy, and the last one sclerotherapy then laser. The patients were followed up at 3 months after the last treatment. Photographs were taken pre-operatively and at 3 months after the last session. They were used for objective and comparative analysis. Statistical analysis was performed using Friedman's test controlling for subject. RESULTS: Improvement was tabulated from the photographic assessment on an improvement scale from 0 (no change) to 4 (greater than 75% clearing). There were clinical improvements in the laser group than sclerotherapy without statistical significance. Side effects were minimal and included hyperpigmentation. CONCLUSIONS: This pilot study demonstrates that the Smartepil LS long pulse Nd:YAG 1,064 nm laser can yield results similar to sclerotherapy in the treatment of small leg telangiectasias. Combination of both methods could increase response to treatment. Lasers Surg Med. 2004;34(5):446-50 60-minute application of S-Caine Peel prior to 1,064 nm long-pulsed Nd:YAG laser treatment of leg veins Jih MH, Friedman PM, Sadick N, Marquez DK, Kimyai-Asadi A, Goldberg LH BACKGROUND AND OBJECTIVES: Advancements in laser treatment of leg veins necessitate concurrent investigations in topical anesthesia to minimize treatment-related pain. To evaluate the efficacy of the S-Caine Peel for providing topical anesthesia after a 60-minute application. STUDY DESIGN/PATIENTS AND METHODS: A randomized, double-blinded, placebo-controlled trial was performed in two centers. Sixty patients received S-Caine Peel and placebo vehicle on different treatment sites for 60 minutes prior to laser treatment of leg veins using a 1,064 nm long-pulsed Nd:YAG laser. Patients rated their level of pain using a visual analog scale. Adequacy of anesthesia and expressed pain at each site were rated by the investigator. RESULTS: The mean visual analog scale (VAS) was 27 mm for active sites compared to 43 mm for placebo (P < 0.001). Improved pain relief was noted for 67% of active versus 30% of placebo sites (P < 0.001). Anesthesia was judged adequate by the investigator for 55% of active compared with 12% of placebo sites (P < 0.001). CONCLUSIONS: The S-Caine Peel is safe and effective when applied for 60 minutes prior to laser therapy of leg veins. Skin Therapy Lett. 2004 Nov;9(9):6-9 Laser treatment of leg veins Sadick NS The role of lasers and intense pulsed light sources has gained increasing popularity in the management of both cosmetic telangiectasias and medically significant symptomatic varicose vein disease. These advances include endovascular technologies, novel cooling technologies, variable spot sizes and pulse durations, as well as the ability to deliver high-energy fluences. These advances have allowed the delivery of sufficient energy allowing more efficient pan-endothelial necrosis without affecting epidermal structures, and yielding a lower complication profile such as post-inflammatory hyperpigmentation and epidermal surface irregularities. The advent of extended-pulse, longer wavelength technologies such as the 1064 Neodymium:Yttrium Aluminum Garnet (Nd:YAG) laser have allowed the treatment of individuals with darker skin phenotypes, as well as treatment of deep blue reticular veins up to 3 mm in diameter in a monomodal fashion. Combined approaches of sclerotherapy plus laser treatments performed during the same treatment session may produce synergistic results in selected individuals. Lasers Surg Med. 2006 Feb;38(2):98-105 Optimal pulse durations for the treatment of leg telangiectasias with a neodymium YAG laser Parlette EC, Groff WF, Kinshella MJ, Domankevitz Y, O'Neill J, Ross EV BACKGROUND: Leg veins can be effectively treated with lasers. However, the optimal pulse duration for small leg veins has not been established in human studies with a Nd:YAG laser. OBJECTIVES: The purpose of this study was to investigate a range of pulse durations to determine an optimal pulse duration for clearance of leg veins. STUDY DESIGN/MATERIALS AND METHODS: After mapping and photo documentation of the leg veins to be treated, a variable pulse duration Neodymium:Yttrium Aluminum Garnet (Nd:YAG) laser (3-100 milliseconds) was used in a single test site session. Pulse durations of 3, 20, 40, 60, 80, and 100 milliseconds were used. At the 3-week follow-up, the optimal pulse duration was defined as that pulse duration which resulted in the most complete clearance of vessels with the least side effects. Up to 20 vessels were then treated using the established "optimal" pulse duration. Final evaluation was at 16 weeks after the initial visit. Three blinded observers rated the percent of vessels completely cleared based on initial and final photographs. RESULTS: Eighteen patients completed the study. Fluence thresholds for immediate vessel changes varied depending on spot size and vessel diameter, with larger fluences required for smaller spot sizes and smaller vessels. Shorter pulse durations (< or =20 milliseconds) were associated with occasional spot sized purpura and spot sized post-inflammatory hyperpigmentation. Longer pulse durations (40-60 milliseconds) achieved superior vessel elimination with less post-inflammatory hyperpigmentation. With a single laser treatment, 71% of the treated vessels cleared. CONCLUSIONS: Compared to shorter pulses (<20 milliseconds), longer pulses may provide gentler heating of the vessel and a greater ratio of contraction to thrombosis. Ann Plast Surg. 2006 Feb;56(2):164-70 A side-by-side prospective study of intense pulsed light and Nd:YAG laser treatment for vascular lesions Fodor L, Ramon Y, Fodor A, Carmi N, Peled IJ, Ullmann Y Recently, lasers and light systems are used more for the treatment of vascular lesions due to their noninvasiveness, ease of use, and short recovery time. This side-by-side prospective study compares results, satisfaction, and complications after intense pulsed light (IPL) and Nd:Yag laser treatment of small vascular lesions. Twenty-five patients with telangiectases, leg veins, or cherry angiomas underwent treatment of the same category of lesion in the same area. One year after completing treatment, patients were asked to report their satisfaction level after comparing digital photos before and after treatment; 72% felt they had good to excellent results after Nd:Yag treatment, while only 48% felt the same after IPL. The most common side effect after Nd:Yag was hyperpigmentation. Satisfaction level was significantly higher after Nd:Yag than after IPL. Patients with telangiectases, cherry angiomas, or leg veins <1 mm were more satisfied after IPL, while those with leg veins >1 mm were more satisfied after Nd:Yag. Overall, satisfaction with treatment of vascular lesions was greater with Nd:Yag although this method was more painful. Br J Dermatol. 2006 Aug;155(2):364-71 Optimal parameters for the treatment of leg veins using Nd:YAG lasers at 1064 nm Baumler W, Ulrich H, Hartl A, Landthaler M, Shafirstein G BACKGROUND: The treatment of large vessels such as leg veins is successfully performed in clinical practice using pulsed Nd:YAG lasers. However, it is still unclear how laser parameters such as wavelength, fluence and pulse duration influence vessel destruction in leg veins. OBJECTIVES: To elucidate the governing parameters in selective photothermolysis of large vessels. METHODS: A recently developed mathematical model for photothermolysis has been adapted for the treatment of leg veins. The model was used to analyse the effectiveness of the selective photothermolysis process in laser treatment of leg veins by Nd:YAG at 1064 nm. The efficiency of laser-induced vessel heating was defined as a ratio between the absorbed and delivered energy. RESULTS: The efficiency improved with increasing vessel diameter, in agreement with clinical findings in various studies. The pulse duration made a minor contribution for laser fluences of 100-400 J cm(-2), whereas the efficiency was better for a small spot. The use of moderate fluences of 100-200 J cm(-2) reduced excess dermis heating and pain. CONCLUSIONS: We provide reference parameters for optimal treatment of leg veins using Nd:YAG lasers at 1064 nm. Our model predicts a maximal efficiency of a range of fluences (100-200 J cm(-2)) and pulse durations (10-100 ms). J Dermatolog Treat. 2010 Jul 28. [Epub ahead of print] Clinical comparison of potassium-titanyl-phosphate (KTP) versus neodymium:YAG (Nd:YAG) laser treatment for lower extremity telangiectases Ozden MG, Bahçivan M, Aydin F, Sentürk N, Bek Y, Cantürk T, Turanli AY Abstract Background: The Nd:YAG laser has been considered the gold standard of treatment for leg veins, but pain and side effects have fueled physicians to use treatment alternatives. Objective: To compare the clinical efficacy of the long-pulsed 1064-nm Nd:YAG laser with KTP laser irradiation in the treatment of leg telangiectasia. Methods: A series of 16 patients with size-matched superficial telangiectases of the lower extremities were randomly assigned to receive three consecutive monthly treatments with the longpulsed 1064-nm Nd:YAG on one leg and 532-nm KTP laser irradiation on the other. Results: For the 16 patients who completed the study, 64 leg vein sites were treated. Average clinical improvement scores were 1.94 and 1.25 for the KTP laser-treated leg and 3.38 and 3.50 for the Nd:YAG laser-treated leg with thin (</= 1 mm) and large (1-3 mm) vessels, respectively. After the third treatment session, average improvement scores of 2.44, 1.31 and 3.75, 3.23 were given for the KTP and Nd:YAG laser-treated sides, respectively. Conclusion: Both the 1064-nm Nd:YAG and KTP lasers are effective in the treatment of lower extremity telangiectases. However, the KTP laser has very low efficacy with vessels larger than 1 mm and should not be elected when treating such vessels. J Dermatolog Treat. 2010 Jul 28. [Epub ahead of print] Clinical comparison of potassium-titanyl-phosphate (KTP) versus neodymium:YAG (Nd:YAG) laser treatment for lower extremity telangiectases Ozden MG, Bahçivan M, Aydin F, Sentürk N, Bek Y, Cantürk T, Turanli AY Abstract Background: The Nd:YAG laser has been considered the gold standard of treatment for leg veins, but pain and side effects have fueled physicians to use treatment alternatives. Objective: To compare the clinical efficacy of the long-pulsed 1064-nm Nd:YAG laser with KTP laser irradiation in the treatment of leg telangiectasia. Methods: A series of 16 patients with size-matched superficial telangiectases of the lower extremities were randomly assigned to receive three consecutive monthly treatments with the long-pulsed 1064-nm Nd:YAG on one leg and 532-nm KTP laser irradiation on the other. Results: For the 16 patients who completed the study, 64 leg vein sites were treated. Average clinical improvement scores were 1.94 and 1.25 for the KTP laser-treated leg and 3.38 and 3.50 for the Nd:YAG laser-treated leg with thin (</= 1 mm) and large (1-3 mm) vessels, respectively. After the third treatment session, average improvement scores of 2.44, 1.31 and 3.75, 3.23 were given for the KTP and Nd:YAG laser-treated sides, respectively. Conclusion: Both the 1064-nm Nd:YAG and KTP lasers are effective in the treatment of lower extremity telangiectases. However, the KTP laser has very low efficacy with vessels larger than 1 mm and should not be elected when treating such vessels. Lasers Surg Med. 2010 Nov;42(9):609-14 Treatment of leg veins with combined pulsed dye and Nd:YAG lasers: 60 patients assessed at 6 months Trelles MA, Weiss R, Moreno-Moragas J, Romero C, Vélez M, Alvarez X INTRODUCTION: Leg telangiectasias have been reported to have been treated with a variety of lasers. This study was designed to measure response to treatment of leg telangiectasias with a unique coupled 585 nm and 1064 nm pulse. METHODS: Sixty female patients (24-62 y.o., skin types II-IV) with leg vein varicosities were treated with pulses of a combined 585 nm long pulsed dye (LPDL) and 1064 nm Nd:YAG lasers, which were delivered sequentially using a novel dual laser device. Pulses were placed along the entire length of the targeted veins. A beam diameter of 7 mm with pulses of 10 ms and 9 J/cm² of fluence for LPDL, and pulses of 30 ms and 80 J/cm² for the 106 nm Nd:YAG were utilized and these remained uniform. Time delays between sequential LPDL and Nd:YAG pulses were 125 ms, 250 ms and 500 ms depending on vein diameter of 4, 3 and 2 mm respectively. One or two treatments were given at 2 month intervals, with post-treatment assessments at 6 months following the final treatment. Patients subjectively assessed the treatment and their results were used to draw up a satisfaction index (SI). Objective assessment was based on clinical photography and computer-generated data using a vein clearance detection computer program. RESULTS: The overall patient satisfaction rate was 47 of 60 patients and the objective assessments, based on blinded evaluation of clinical photography as well as computer assessment, demonstrated good to very good improvement in 47 by photograph evaluation and 49 of 60 patients by computer edge detection data. CONCLUSIONS: The combination of LPDL and Nd:YAG laser pulses offered efficient treatment of leg veins irrespective of skin type. Results were better on blue and vessels larger than 1 mm. Side effects were minimal and transient. FRAXEL - 1550 nm J Cosmet Laser Ther. 2007 Jun;9(2):101-3 Fractional photothermolysis for the treatment of telangiectatic matting: a case report Glaich AS, Goldberg LH, Dai T, Friedman PM BACKGROUND: Recent reports have demonstrated clinical and histologic evidence of the potential benefit of fractional photothermolysis (1550 nm Fraxel SR laser) for the treatment of dermal vascular lesions. This report evaluated the potential efficacy of fractional photothermolysis for the treatment of matted telangiectasias. METHODS: A 62-year-old female, Fitzpatrick skin type III, with matted telangiectasias on her right medial thigh underwent five successive treatments at monthly intervals with the 1550 nm Fraxel SR laser. Digital photographs were taken prior to each treatment and at 6 months after the last treatment. Clinical assessments were performed by a non-treating physician. RESULTS: Clinical assessment 6 months after the last treatment with the Fraxel SR laser revealed marked improvement in the clinical appearance of the matted telangiectasias. The patient's degree of satisfaction paralleled the physician's assessment of improvement. Side effects were limited to mild pain during treatment and mild, transient post-treatment erythema and edema. CONCLUSION: Fractional photothermolysis is a potentially effective modality for the treatment of matted telangiectasias and warrants further studies. No long-term adverse events were noted and the safety profile appears to be fairly broad.