1 Methylene Blue-Assisted Technique for Harvesting Lymph Nodes
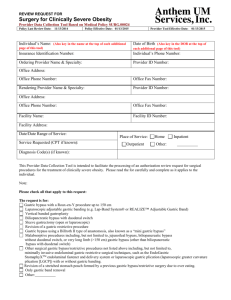
advertisement

1 1 Methylene Blue-Assisted Technique for Harvesting Lymph Nodes after Radical 2 Surgery for Gastric Cancer: A Prospective Randomized Phase III Study 3 4 Primary Investigators 5 Toru Aoyama and Takaki Yoshikawa 6 Department of Gastrointestinal Surgery, Kanagawa Cancer Center 7 2 8 0. Summary 9 Specimen after gastrectomy 10 Stratification factors: ・type of gastrectomy 11 12 (distal/total) ・extent of lymph node dissection 13 14 (D1+/D2) Randomized 15 16 Methylene Blue-Assisted Technique Standard methods 17 18 Primary end point:the ratio of the number of harvested lymph nodes to time (minutes) 19 Secondary end point:the number of harvested lymph nodes 20 21 1. Aim 22 The purpose of this study was to confirm the efficiency of the methylene 23 blue-assisted technique in harvesting LNs after gastrectomy with radical 24 lymphadenectomy for gastric cancer in comparison to the standard approach using fresh 25 samples. 3 26 Primary end point:the ratio of the number of the harvested lymph nodes to time 27 (minutes) 28 Secondary end point:the number of harvested lymph nodes 29 30 2. Background 31 Gastric cancer is the second most frequent cancer-related cause of death 32 following lung cancer1. Surgical resection with radical lymphadenectomy is the 33 standard treatment when the gastric cancer is local. The treatment strategy is determined 34 based on the pathological diagnoses of tumor invasion and lymph node metastasis. The 35 TNM classification recommends conducting a nodal examination of at least 16 or more 36 regional lymph nodes (LNs) when determining the N factor2. 37 Nodal sampling of specimens is influenced by the physician’s experience, 38 extent of dissection, type of gastrectomy and method used to harvest the LNs. Usually, 39 surgeons harvest LNs from fresh specimens immediately after surgery in Japan, while 40 pathologists in other countries harvest LNs from specimens fixed with formalin after 41 surgery3. Although surgeons may be more enthusiastic about harvesting LNs than 42 pathologists, it is difficult to perform this work immediately after surgery. On the other 43 hand, nodal sampling can be difficult for pathologists who are not familiar with surgical 4 44 anatomy. Moreover, tissues fixed with formalin are hard and difficult to separate; thus, 45 nodal sampling is time-consuming work for most pathologists. 46 The methylene blue-assisted technique is an alternative approach for harvesting 47 LNs. The specimens are fixed with formalin containing methylene blue after surgery, 48 thus allowing physicians to easily identify LNs stained with blue dye. Märkl reported 49 that the methylene blue-assisted technique for colon cancer is significantly superior to 50 the conventional method using samples fixed with formalin4. Several Japanese surgeons 51 have reported the efficacy of this method in single-arm gastric cancer studies 52 remains unclear whether the methylene blue-assisted technique is superior to the 53 Japanese standard method using fresh samples in patients with gastric cancer. 5,6 . It 54 55 3. Patients and methods 56 3.1 Eligibility criteria 57 The tumors will be staged according to the Japanese classification of gastric 58 carcinoma 3rd English edition7. The inclusion criteria are: 59 (i) Histologically proven adenocarcinoma of the stomach. 60 (ii) Clinical stage 1-3 disease. 61 (iii) R0 resection achieved via gastrectomy with D1+ or D2 lymphadenectomy as a 5 62 primary treatment according to the Japanese gastric cancer treatment guidelines, 2010 63 (ver. 3) 8. 64 Patients who receive any other treatment before surgery will be excluded. 65 3.2 Surgery 66 Patients with gastric cancer will undergo distal or total gastrectomy with 67 radical lymphadenectomy. The extent of dissection will principally follow the third 68 edition of the Gastric Cancer Treatment Guidelines published by the Japanese Gastric 69 Cancer Association8. Spleen-preserving D2 total gastrectomy is permitted in this study. 70 3.3 Harvesting lymph nodes and methylene blue staining 71 In the standard group, the LNs will be harvested from the specimen 72 immediately after surgery. In the methylene blue group, the specimens will be fixed 73 with 10% buffered formalin with methylene blue for 48 hours after surgery. Then, the 74 LNs will be harvested from the specimens. 75 3.4 Registration 76 Surgeons will register the eligibility criteria with the data center following 77 confirmation during surgery. The patients will be randomized and assigned to the 78 standard group or the methylene blue-assisted group using a centralized dynamic 79 method based on the following factors: lymphadenectomy (D1+/D2), type of 6 80 gastrectomy (subtotal/total) and surgical experience (less than 15 years/15 years or 81 more). The accrual was started in August 2012 and will continue for one year. 82 3.5 Qualifications of the participating surgeons 83 The surgeons harvesting LNs in this study are limited to those who have 84 performed at least 50 or more procedures of harvesting LNs for gastric cancer. 85 3.6 Statistical methods 86 The present study is a randomized phase III study performed to evaluate the 87 efficiency of the methylene blue-assisted lymph node technique for harvesting LNs after 88 surgery for gastric cancer. The primary end point is the ratio of the number of harvested 89 LNs to time (minutes). A 25% reduction in the ratio of harvested lymph nodes/time 90 (minutes) is necessary for this test treatment, considering the balance between the cost 91 and benefits. Retrospective data obtained from this institution were used to estimate the 92 ratio of the number of harvested LNs to time (minutes) in the control arm to be 40 per 93 30 minutes. A 25% risk reduction in the test arm is expected, with a rate of 40 per 22.5 94 minutes in the test arm. These conditions will require a sample size of 52 patients, with 95 26 patients per arm to ensure a two-sided alpha error of 5% and a statistical power of 96 80%. A total of 60 patients will be recruited due to the likelihood of enrolling ineligible 97 patients. 7 98 99 References 100 1. Ohtsu A, Yoshida S, Saijo N. Disparities in gastric cancer chemotherapy between the 101 East and West. J Clin Oncol 2006; 24: 2188-2196. 102 2. Sobin LH, Gospodarowicz MK, Wittekind Ch, International Union Against Cancer. 103 TNM Classification of Malignant Tumors. 7th ed. Oxford, UK: Wiley-Blackwell; 2009. 104 3. Bunt AM, Hermans J, van de Velde CJ, Sasako M, Hoefsloot FA, Fleuren G, et al. 105 Lymph node retrieval in a randomized trial on western-type versus Japanese-type 106 surgery in gastric cancer. J Clin Oncol. 1996; 14: 2289–94. 107 4. Märkl B, Kerwel TG, Jähnig HG, Oruzio D, Arnholdt HM, Schöler C, et al. 108 Methylene blue-assisted lymph node dissection in colon specimens: a prospective, 109 randomized study. Am J Clin Pathol 2008; 130: 913-9. 110 5. Isozaki E, Okajima K, Fujiwara A, Yasuda M, Yamada S, Mizutani H, et al. A study 111 of lymph node-metastases of gastric cancer using the methylene blue formalin fixing 112 method. Rinsho Shinkeigaku 1986; 26: 710-716 [Article in Japanese]. 113 6. Kurosu Y, Isozumi M, Aoki N, Ishikawa S, Isgii I, Tanjo K, et al. Study on lymph 114 node metastasis of cancer using the methylene blue formalin fixing method. J Nihon 115 Univ Med Ass 1987; 46: 1057-1059 [Article in Japanese]. 8 116 7. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 117 3rd English edition. Gastric Cancer 2011; 14: 101-12. 118 8. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 119 2010 (ver. 3). Gastric Cancer 2011; 14: 113-23.