ERCP in patient with altered Upper GI anatomy
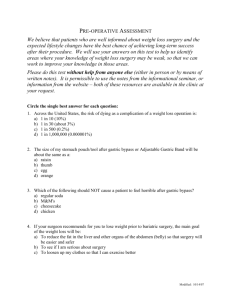
advertisement
ERCP in patient with altered Upper GI anatomy Bariatric surgery • • • • 75 million Americans are obese, BMI > 30 15 million are morbidly obese, BMI >40 Total economic cost $147 this year, and rising 200,000 bariatric surgeries performed in 2012 – 1-2% are on patients less than 21 years old – 39% are Lap band procedure – 61% Roux en Y Gastric bypass or gastric sleeve Bariatric surgery • Success defined as 50% loss of excessive weight. • Success rate is higher with RYGB surgery compared with Lap band • Complications: GERD, Vomiting, Stricture, anastamotic ulcers , anastamotic leak. • 25% of gastric bands require additional surgery for revision or removal Gallstones in Bypass patients • If Gallstones are present at the time of Gastric bypass, elective cholecystectomy generally done, otherwise prophylactic chole not done Rapid wt loss is a risk factor for gallstone formation. Risk of stone formation • 125 patients followed for at least 16 months following RYGB, none had stones at time of bypass surgery, none treated with urso: – 100 female; 25 male subjects – 10 developed symptomatic gallstones in 3-21 months following bypass, and required surgery; – All 10 pts were female – Treated with lap chole, or open chole – Caruana et al Surg Obes Rel Dis 2005, Nov. 564 Gallstones in Bariatric surgery • Estimated that 30% will form stones at some point following gastric bypass • Reduced to 2% by giving URSO for 6 months post op. • Gallstones migrating into the common bile duct can cause pancreatitis , jaundice, cholangitis. ERCP after bypass or Whipple • Standard transoral ERCP is difficult or impossible following Bypass • The Roux limb is 50-100 cm long. • The Limb passes thru the mesentery at the distal anastamosis. • The endoscope approaches the ampulla backwards, making cannulation, and sphincterotomy difficult. Treating common duct stones should be done before gallbladder is removed • Percutaneous cholangiogram, with basket lithotripsy, and balloon dilation of the ampulla • Open gastric access to create stoma in gastric reminant to pass duodenoscope to the ampulla, then conventional sphincterotomy, followed by balloon or basket stone removal • Single or double balloon enteroscopy • Operative common duct exploration Open gastric access • Done in OR, general anesthesia, laparotomy with 4-5 inch midline incision. • Sterile technique for Gastroenterologist, and assisting Nurse • Protocol approved by surgery department and endoscopy unit is essential • Surgical capability for common duct exploration is essential Start with the scope • High level disinfection – Duodenal scope – Forward view diagnostic endoscope in case of unexpected pathology, such as pyloric stenosis that needs balloon dilation – Extra air water, suction valves, and instrument channel caps – Sterile cautery cable that is compatible with your equipment scope • Operating Room tech will come to scope washing facility to remove the scope from washer, and transport to OR in sterile container using sterile technique Instruments • The OR scrub nurse will take instruments from package and place on sterile field – Contrast, syringes (consider full strength) – Saline wash – Sphincterotome, straight and curved guidewire – Retrieval balloon – Stone basket with lithotripsy capability Back up instruments: • • • • TTS CRE balloon for pylorus Pancreatic stents 5 french, Wilson Cook Biliary stents, 10 fr, 5 and 7 cm length Fully coated biliary stent (Boston Scientific) Patient preparation • • • • Pre op antibiotics Fluoroscopy table DVT prophylaxis Possible PEG tube placement if further endoscopy is needed for stent removal • Not currently using indomethacin suppository for post ERCP procedure pancreatitis Length of Procedure • OR time 2-3 hours (longer if CBD exploration) • ERCP time ; 30 minutes to set up equipment, 30-40 minutes of endoscopy time • Fluoroscopy generally 5 minutes • Recovery: • 1-2 days in hospital, longer if pancreatitis or cholangitis