Chapter15 - World Laparoscopy Hospital
advertisement

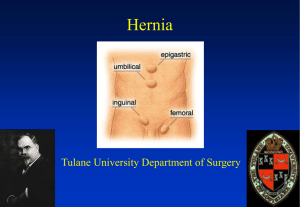
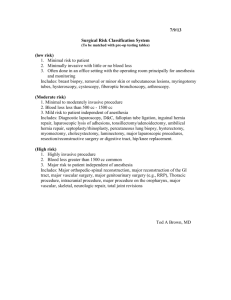
Laparoscopic Inguinal Hernia Repair—TEP Technique Pradeep K. Chowbey The inguinal hernia repair has been a controversial area in the surgical practice from time it has been conceived. The history of inguinal hernia repair over several decades implies how innovations are adopted into surgical practice through combination of scientific and subjective processes. The techniques of laparoscopic hernia repair have evolved in parallel with experience and technology. In the laparoscopic procedure, tension free repair is achieved by placement of a prosthetic mesh to cover the entire groin area including the sites of direct, indirect and femoral hernia. The laparoscopic approach is based on the principle of tension free repair, which has been well established by open operation by Nyhus and Stoppa. The greater availability of space in the extraperitoneal approach facilitates the insertion of a much bigger mesh. Patient selection TEP groin hernia repair is an advanced laparoscopic procedure. It requires greater skills of laparoscopic dissection and manipulation as the working space available is limited. It has a long learning curve and must be done only after acquiring experience in basic laparoscopic procedures and when the learning curve is over. Today, we are well past the learning curve and have performed well over thousand laparoscopic groin hernia repairs. Except for strangulated hernia, at present there are no absolute contraindications for this procedure. Relative contraindications include patients unfit for anesthesia, obese and pregnant patients and patients with a history of lower abdominal surgery. Preoperative preparation A thorough history of the presenting complaints and other comorbid conditions should be taken. Specific measures should be taken if the patient is on drugs like Aspirin and warfarin, oral hypoglycemic agents etc. Besides routine hematological investigations, other specific investigations like X-Ray chest, ECG, coagulation profile, pulmonary function test etc should be done for patients with history of cardiac / pulmonary pathology. A written consent should be taken explaining the probable complications and possibility of conversion to open surgery. Following preanesthetic check up and clearance for surgery, the patient is kept fasting overnight. The patient is prepared adequately. Surgical Technique The procedure is done under general anesthesia (regional anesthesia if the patient is unfit for general anesthesia). The patient is catheterized or asked to empty the bladders before surgery and prophylactic antibiotic is given at the time of induction of anesthesia. After induction, complete reduction of the contents of the hernial sac is ensured. Extraperitoneal access A 10mm infraumbilical transverse incision is made. The anterior rectus sheath is exposed and transverse incision is then made on the anterior rectus sheath to one side of the midline to avoid inadvertent opening of the peritoneum [Fig.1]. The margins of incised sheath are held in stay sutures using vicryl 1-0 [Fig.2]. The rectus muscle is retracted laterally from the midline and by finger dissection a space is created between the rectus muscle and the posterior rectus sheath. Fig. 1: Transverse infraumbilical incision with incision in anterior rectus sheath Fig. 2: Stay sutures over incised anterior rectus sheath Balloon dissection of the extraperitoneal space A self made balloon is then inserted in this preperitoneal space. The balloon trocar used by us is an indigenously made trocar where we tie two finger stalls of a size 8 latex surgical glove on the tip of the 5 mm laparoscopic suction cannula [Fig. 3]. The balloon trocar is the inflated with 100150ml of saline. It not only creates an initial working space but also brings about hemostasis by balloon tamponade. The balloon is then deflated and the cannula is removed. A 10 mm Hassan’s cannula (blunt tip cannula) mounted with a conical sleeve is then introduced into the preperitoneal space through the infraumbilical incision [Fig. 4]. The conical sleeve snuggly fits into the incision and is secured with stay sutures. The insufflation tubing is attached to the Hasson’s Cannula and insufflation is begun with pressure setting at 12 mm Hg. A 10 mm 30° telescope is used. The camera is introduced through the sub umbilical port and preperitoneal space is visualized. The other two working ports are placed in the preperitoneal space. First, a 5 mm port is placed about 2-3 cm above the pubic symphysis in the midline and second, a 5/10 mm port is placed in the midline midway between the two placed ports (subumbilical and suprapubic) [Fig. 5 & 6]. Fig. 3: Indigenous balloon trocar Fig. 4: Hassan’s cannula introduced in sub umbilical port Dissection of the extraperitoneal space The surgeon stands on the side opposite to the operating side / or side where hernia is present. Dissection in extra peritoneal space begins by dividing the loose areolar tissue in the midline using sharp and blunt dissection. The first landmark / reference point i.e. the pubic bone is identified which appears as white glistening structure in the midline. The pubic bone is visualized and bared of all connective tissue creating a shelf extending about 2-3 cm in the retropubic space, which acts as a shelf to place the mesh [Fig.7]. The dissection is then traced laterally towards the side of the hernia. In case of direct hernia, the hernial sac is visualized as a weakness in the Hasselbach’s triangle medial to the inferior epigastric vessels. On the other hand, in the indirect hernia, the inferior epigastric vessels are seen before the hernial sac, which is encountered laterally. Once the adhesions are lysed or hernial sac is reduced as in direct hernia, the anatomical landmarks which now become visible are Cooper’s ligament, iliopubic tract, femoral canal and the inferior epigastric vessels [Fig. 8, 9]. Fig. 5: Port placement for TEP Fig. 6: Preperitoneal space Fig. 7: Preperitoneal space Fig. 8: Left direct hernial defect seen after dissection Fig. 9: Right direct hernial defect The spermatic cord lies immediately inferior and lateral to the inferior epigastric vessels. The adhesions all around the cord are lysed with caution as the external iliac vessels lie just below the cord structures. The peritoneal extension (sac) is seen as a white glistening structure lying anterolateral to the cord [Fig.10]. The sac is completely dissected off the cord structures and reduced. In cases of complete hernia, attempt should not be made to completely reduce the sac as excessive traction and dissection causes severe postoperative pain and edema. The sac should be transected and ligated using a catgut endoloop or by intracorporeal sutures, leaving the distal sac open in situ [Fig.11]. Fig. 10: Right indirect hernial sac with cord structures Fig. 11: Dissected and ligated right indirect hernial sac The peritoneal sac with reflection is completely reduced. The vas deferens is seen lying separately on the medial side and gonadal vessels are seen on the lateral side forming a triangle. This triangle, known a “triangle of doom”, is bounded medially by the vas deferens laterally by gonadal vessels with its apex at the internal inguinal ring and the base is formed by the peritoneum. No dissection should be carried within this triangle as it contains the external iliac vessels. Dissection is continued lateral to the cord structures to create adequate space for the placement of mesh. The lateral space contains loose aerolar tissue, which is completely divided using sharp and blunt dissection. The psoas muscle is seen lying on the floor on which lateral cutaneous nerve of thigh and genito femoral nerve can be seen transversing. The anterior superior iliac spine marks the lateral boundary of the dissection. After creating the lateral space adequately the mesh is introduced through the 10mm subumbilical port [Fig.12]. The mesh is placed over the space created so that it covers the sites of direct, indirect, femoral and obturator hernias [Fig.13]. The mesh is the secured in place with the help of fixation devices like helical fasteners, staples anchors etc. depending upon the preference of the surgeon. After adequately spreading the mesh, which extends from the midline medially, to lying over the psoas muscle on the lateral side, preperitoneal space is deflated. In cases of bilateral hernias the similar procedure can be done on both the sides through the same three ports made for unilateral repair. Fig. 12: Rolled prolene mesh Fig. 13: Prolene mesh being placed for repair