outline25074

I.
Diagnostic Dilemma
A.
Optic nerve elevation is most challenging when it is bilateral
1.
Is it or is it not swollen?? a.
How can one differentiate the “elevated” from “swollen” b.
“Just because the nerve is elevated doesn’t mean it MUST be swollen”
2.
If so, now what to do about it?
3.
If not, what to do about it?
B.
What is the optometrist’s role in a case of bilateral disc elevation and/or edema?
1.
Detection and identification of true v. psuedopapilledema
2.
Timely and appropriate referral to specialist as needed
3.
Co-management (monitoring) condition
C.
Why is it important for practitioners to clearly differentiate congenital causes of disc elevation from acquired disc edema?
1. Important in order to avoid unnecessary and expensive neurological testing.
2. More important to avoid overlooking true, neurological disorders and provide the appropriate patient education and management
II.
Exam Checklist
A.
In every case of ONH elevation there should be an “instant checklist”, to help the practitioner to effectively determine if the nerve is in fact “swollen” or “elevated”
1.
Organize approach to case
2.
Logical approach to differential diagnoses
3.
Appropriate diagnosis of clinical findings
B.
Exam Checklist:
1.
History, History, History and don’t forget the BP
2.
BVA, EOM, color, pupils, VF (HVF 30-2), brightness comp/red cap desaturation
3.
Stereoscopic examination of ON
4.
Take baseline stereoscopic photos in the most questionable cases
5.
Neurological exam PRN based on clinical findings and symptoms
C.
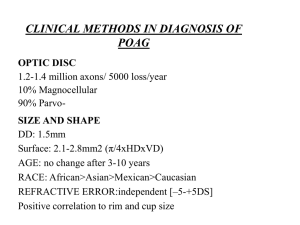
Optic Nerve Evaluation Key Characteristics
1.
Disc appearance – size and margins
2.
Neuroretinal rim – color, elevated (raised) vs. swollen??
3.
Nerve Fiber Layer- thickened, flame hemes, CWS, exudates
4.
Cup- C/D, shape, asymmetry? ??SVP +/-
5.
Vessels a.
Anomalous vessel branching at disc - congenital b.
Tortuosity – congenital when art/vein both involved c.
Obscuration of the peripapillary vessels – SWOLLEN
III.
Differentials to Consider in Bilateral disc swelling/elevation:
A.
Papilledema
1.
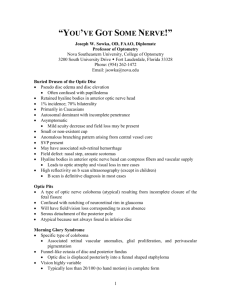
Papilledema – pathophysiology
2.
Papilledema – symptoms a.
Headaches – morning, middle of night, no relief, w/or w/o nausea b.
Transient visual obscurations (TVO) – 68% of PE cases c.
Tinnitus – “whooshing” – 58% of PE cases
d.
Sixth Nerve Palsy (SNP) – 38% of PE cases
3.
Papilledema – signs a.
VA, pupils, EOM, normal (unless SNP) b.
VF, variable but typically an enlarged blind spot, R/O neurological visual pathway defects w/ HVF 30-2 c.
Mild, moderate, severe degrees of disc edema/swelling – key characteristics
• Hyperemic rim tissue w/ blurred margins, no SVP, ?EVP
• Peripapillary vessel obscuration
• Optic nerve function: No APD, No conduction defects
4.
Papilledema – Causes a.
Space occupying mass. Guilty until proven innocent!! b.
Pseudotumor Cerebri (PTC) aka Idiopathic Intracranial HTN c.
Malignant Hypertension d.
Thyroid Optic Neuropathy
5.
Diagnostic Dilemma - Now what to do about it?? a.
Run a 30-2 HVF, stereo photos b.
Send patient for MRI w/in 24hrs, immediate neuroimaging MUST be done before the lumbar puncture!
• Why before lumbar puncture, Why MRI v. CT Scan?
• How-to write order for MRI
• MRI findings of PTC such as empty sella, partially empty sella c.
Refer to neurologist
• Neurosurgeon for brain mass, aneurysm
• Neuro-ophthalmologist for optic nerve fenestration, decompression surgery d.
Co-management by optometrist to monitor, VA/VF and PE resolution
B.
Pseudopapilledema (PPE): The false impression and appearance of papilledema. Accounting for 75% of diagnostically challenging disc anomalies
1.
Optic Nerve Head Drusen (ONHD) - Most common cause of PPE a.
Optic Nerve Head Drusen (ONHD) – key characteristics
• The discs are small with little to no cup, VA, EOM -normal
• +SVP in 80%, no hyperemia,
• Surface vessels are not obscured, anomalous patterns
• +/- VF defects, 73% of visible, 36% of buried b.
Diagnostic Dilemma - Now what to do about it??
• Bscan, VF, patient ed and management
• OCT, why is this diagnostic tool so helpful?
2.
Congenitally Full Disc (CFD) aka Crowded Disc – a.
Key characteristics
• bilateral or asymmetrical disc elevation, smaller than avg size
• Surface vessels are not obscured, little to no physiological cup
• Anomalous vascular patterns and tortuousity
• VF-Normal ---DDx from ONHD
• B-scan – Normal ---DDx from ONHD
• OCT – Normal, NO thinning, but may be slightly thicker
b.
Now what to do about it??
• Photodocument
3.
Malinserted /Oblique inserted a.
Key characteristics
• Nasal rim/margin is elevated (heaped up) with the temporal portion depressed
• Often seen with a scleral crescent or choroidal crescent
• Often associated w/ myopes and familial trait
• Possible VF defects b.
Now what to do about it?
• Photodocument
4.
Tilted Disc vs. Malinserted Disc a.
Key characteristics of tilted disc
• The vertical axis itself is tilted, disc appears to be tilted downward nasally
• Often Fuch’s coloboma = hypoplasia of the inferior nasal quadrant b.
Malinserted Disc:
• The disc is tilted along the vertical axis
• No Fuch’s coloboma c.
Tilted Optic Disc Syndrome
• Constellation of tilted ON with “Situs Inversus” and BI-Temp VF defect
• Optic disc usually appears to be tilted downward and nasally
• Inferior nasal crescent (Fuchs' coloboma) and inferior nasal ectasia d.
Now what to do about it?
• Photodocument and monitor VF
• Patient education
C.
Congenital nerves can become “swollen”
IV.
Case Presentations – Diagnostic Dilemma: "Is it or is it not swollen and now what to do about it?”
A.
Case #1 Early papilledema: disc photos, VF, OCT
B.
Case #2 ONHD: disc photos, VF, OCT, Bscan
C.
Case #3 CFD: disc photos, OCT, Bscan,
D.
Case #4 Malinserted disc w/ ONHD: disc photos, VF, Bscan, OCT
V.
References
A.
Brodsky, MC, Vaphiades,M.;MRI in Pseudotumor Cerebri;Ophtalmology 1998;105:1686-1693
B.
Wilkins J, Pomeranz H., Visual Manifestations of Visible and Buried Optic Disc Drusen. Journal of
Neuro- Ophtalmologgy 2004;24(2):125-129
C.
Schuman J., Puliafito C., Optical Coherence Tomography of Ocular Diseases. Slach Incorporated,
2004: 611-51.
D.
Roh S., Noecker R., Schuman J., Effect of Optic Nerve Head Drusen on Nerve Fiber Layer Thickness.
Ophthalmology 1998;105(5): 878-885.
E.
Byrne S., Green R., Ultrasound of the Eye and Orbit. Mosby, 2002:434-37.