University of Colorado Hospital Policy and Procedure
advertisement

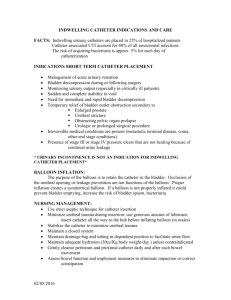
University of Colorado Hospital Policy and Procedure Insertion, Removal and Care of an Indwelling Urinary Catheter Related Policies and Procedures: Hand Hygiene – Outside the Surgical Setting Approved by: Professional Practice, Policy and Procedure Committee Effective: 9/04 Revised: 12/12 Description: This policy provides the procedure to ensure the safe, sterile placement and removal of the indwelling urinary catheter (IUC). It also provides guidelines for catheter care and specimen collection from the catheter. Accountability: The prescribing provider (e.g. physician, physician assistant, nurse practitioner) is responsible for writing the order for placement of the IUC. Only properly trained persons (registered nurse, licensed practical nurse, advanced care partner, emergency medical technician or paramedic) who know the correct technique of aseptic catheter insertion and maintenance is responsible for placing an IUC. The above personnel must have demonstrated the knowledge and skills to perform this procedure as evidenced by verification on a competency checklist. Insert IUC only for appropriate indications and leave in place only as long as needed (HICPAC/CDC Guidelines) (see Appendix A) Consider using alternatives to IUC as appropriate (e.g. commodes, external catheters for males, urinals, incontinence pads) Table of Contents: A. Policies/Procedures: ................................................................................................................ 2 B. General Insertion Procedures .................................................................................................. 2 C. Female Insertion Procedure .................................................................................................... 2 D. Male Insertion Procedures ...................................................................................................... 3 F. Directions for Removal ........................................................................................................... 4 G. Fill and Pull ............................................................................................................................. 4 H. Bladder Scanning: ................................................................................................................... 4 I. Patient Care and Considerations ............................................................................................. 5 J. Infection Control Considerations ............................................................................................ 5 K. MRI Procedures for Temperature Sensing IUC...................................................................... 6 References: ...................................................................................................................................... 6 Appendix A ..................................................................................................................................... 9 c253312 Page 1 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter A. Policies/Procedures: 1. Identify the patient using the required two patient identifiers. 2. Verify that the patient is not allergic to latex, iodine or betadine. If the patient is sensitive or allergic to latex, replace the catheter in the kit with a silicone catheter. If the patient is allergic to iodine or betadine, use an alternate cleanser such as chlorhexidine. 3. Gather equipment: IUC kit (use non-latex for patients with latex allergies). a. Use the smallest size catheter that is appropriate. b. If temperature sensing IUC is clinically indicated, it should be utilized in the Operating Room, Emergency Department and Critical Care Units only. 4. Explain the procedure to the patient and maintain the patient’s privacy and dignity. 5. Perform hand hygiene immediately before and after insertion or with any manipulation of the IUC. 6. Documentation of placement of the foley can be done in the EHR by creating a new LDA and documenting placement date and time. B. General Insertion Procedures 1. Visually inspect the product for any imperfections or surface deterioration prior to use. If any damage is noted or the package has been opened, do not use. 2. Don protective eye wear. 3. Wash the patient’s genital area before the procedure if visibly soiled. Don non-sterile gloves, wash patient’s genital area with foam body cleanser (4:1 body cleanser), or Ready cleanse™ wipes. Remove gloves and perform hand hygiene. 4. Using aseptic technique, open the outer plastic wrap to form a sterile field and place the underpad beneath the patient, plastic side down. 5. Apply non-sterile gloves and cleans genital area with soap provided in IUC kit. Remove gloves. Perform hand hygiene. 6. Don Sterile gloves 7. Position the sterile fenestrated drape around the patient’s genitalia. 8. Use aseptic technique and sterile equipment for the IUC insertion. 9. Before insertion, dispense the lubricating gel into the kit tray. Remove the plastic sleeve from the catheter and lock the sterile water syringe into the port. DO NOT PREINFLATE THE BALLOON PRIOR TO INSERTION. 10. Open the antiseptic swab sticks. Use each swab stick for one swipe only in cleansing genital area. 11. Using the dominant, sterile hand to handle the catheter, cover the tip of the catheter with lubricant. Insert the IUC through the urethra into the bladder. a. Instruct the patient to inform the nurse if any discomfort is felt with inflation of the balloon. If discomfort is felt, the catheter is probably in the urethra and will need to be deflated and advanced. Inflate the balloon slowly, using the entire 10 mL of sterile water. Withdraw the catheter slowly to the point of resistance at the bladder neck. C. Female Insertion Procedure 1. Position female patient into a frog-leg pose. c253312 Page 2 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter 2. Separate the labia using the non-dominant hand and visualize the meatus. Cleans with antiseptic swab sticks, cleanse one side of the labia from top to bottom and discard swab stick away from the sterile field. Repeat on the opposite side and then wipe down the middle using the third swab stick. 3. Insert the catheter approximately three inches, wait to see if urine flows, then advance another 2 inches before inflating balloon. 4. For unconscious female patients or those with decreased sensation (i.e. paralyzed), insert the catheter slightly further than three inches, to make certain the catheter is in the bladder. D. Male Insertion Procedures 1. Position male patients into a supine pose. 2. Retract the foreskin, if present, and hold the shaft of the penis with the non-dominant hand. Grasp one antiseptic swab stick and using a circular motion, wipe the glans from the meatus outward. Discard the swab stick away from the sterile field. Repeat with two more swab sticks. Grasp the penis in an upright position and insert the lubricated catheter firmly into the meatus, advancing the catheter to the bifurcation at the ‘Y’ of the catheter. A slight lean toward the umbilicus may be necessary if resistance in advancing the catheter is met at the prostate. 3. The return of urine does not assure that the catheter is placed correctly in males, since there is residual urine in the penis. Inserting the catheter to the bifurcation of the Y is the standard for assurance of proper placement. 4. If the foreskin was retracted, reposition it after placement. 5. If catheter placement is in question (i.e. no urine return or unable to fully insert the catheter), do not inflate the balloon and contact the physician. 6. If resistance is met, do not attempt forceful catheter insertion; apply continuous gentle pressure and ask the patient to take slow deep breaths to help relax or instruct the patient to try to void to open the sphincter and allow the catheter to pass. E. Complete the Procedure 1. Secure the catheter to the patient’s thigh with hospital-approved catheter securement device (ie: Stat Lock) to prevent movement, urethral traction, and irritation. To improve urine flow, some men may need to have the catheter secured slightly upward. For males with long-term catheters, the catheter should be secured to the abdomen to prevent damage to the inferior urethra. 2. Position the collection bag to avoid urine reflux into the bladder, kinking, or gross contamination of the bag. For inpatient setting, position the bag hanger on the bed rail near the foot of the bed using the clip to secure the drainage tube to the sheet. Keep the bag below the level of the bladder at all times to prevent the backflow of urine and decrease the risk for infection. Never leave the catheter hanging to be pulled by the weight of the bag. Do not leave the bag laying on the floor unless necessary due to patient positioning (i.e. Trendelenberg position in the Operating Room). 3. Periodic observations of the system should be made to ensure that urine is flowing freely. If a standing column of urine is observed, check for correct positioning of the bag and then for a physical obstruction, such as a kink in the tubing. 4. If correct positioning of the bag or removal of physical obstruction does not allow free flow, the bag may have to be changed. c253312 Page 3 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter F. Directions for Removal 1. Deflate the catheter balloon by negative pressure. Exercise the plunger of a luer-tipped 10 ml syringe by moving up and down within the syringe barrel. Pull back 0.5 ml air in the syringe to prevent adherence of the plunger to the end of the syringe barrel, then insert the syringe into the balloon port. (This allows for automatic flow of instilled liquid and balloon deflation via negative pressure in the syringe.) Never use more force than is required to make the syringe “stick” in the valve. Use gentle aspiration, only if needed, to encourage deflation. 2. Allow the pressure within the balloon to push the plunger back and fill the syringe with water. 3. NEVER FORCE THE WATER INTO THE SYRINGE. Vigorous aspiration may collapse the inflation lumen, preventing balloon deflation. Allow 30 seconds for the balloon to deflate. 4. If there is slow or no deflation, re-seat the syringe gently. 5. If the retention balloon still does not deflate, reposition the patient to ensure catheter is not in traction or compressed within the bladder. 6. If this fails, contact the prescribing provider. 7. Consider alternatives for elimination (e.g. bedside commode, urinals, external catheters, incontinence pads, nursing rounds to offer elimination options) if the patient is not fully ambulatory. G. Fill and Pull 1. Fill and Pull is a procedure ordered by the prescribing provider prior to IUC removal only for patients who have had surgery around the outlet of their bladder or are experiencing urethral swelling. 2. Prescribing provider order is required. 3. Using aseptic technique disconnect plastic drainage tube from the indwelling urinary catheter (IUC). 4. Insert a Toomey tip syringe into the end of the (IUC). Fill bladder with up to 250 mL of sterile normal saline unless patient complains of pain or discomfort. Notify prescribing provider if unable to instill 250 mL. 5. Passively deflate the balloon on IUC using a 10 mL syringe; ensure all fluid is removed from balloon (some catheters are filled with more than 10 mL). 6. Gently remove the IUC. 7. Wait for the patient to void. 8. Immediately after patient urinates, check post void residual (PVR) using bladder scanner. 9. Contact prescribing provider with PVR and voided amount to determine if the patient needs replacement of IUC catheter or any other interventions (If PVR is more than150 mL, IUC may need to be replaced). H. Bladder Scanning: 1. If the patient does not void within 4-6 hours of removing the IUC, a bedside bladder scan ultrasound should be performed. 2. If the bladder volume is less than 500 mL, encourage the patient to void by using techniques to stimulate bladder reflex (cold water to abdomen, stroke inner thigh, run water, flush toilet). Continue to assess the patient and repeat the bladder scan in 2 hours if the patient has not voided. c253312 Page 4 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter 3. If the bladder volume is greater than 500 mL, catheterize for residual urine volume rather than place an IUC. I. Patient Care and Considerations 1. Always use aseptic technique and sterile equipment when inserting a IUC Document the following: a. Indication for IUC insertion b. Date and time of IUC insertion c. Name and credentials of who inserted IUC if other than person documenting procedure. d. Procedure, including the size of the catheter placed, the color, amount, and clarity of urine returned after the initial placement, and patient response. e. Catheter removal. f. Use of the bladder scanner, amount of residual volume, need for intermittent catheterization. 2. Record urine output as ordered. 3. Assess the patient for pain during and after procedure. Provide pain relief measures as indicated and document response. J. Infection Control Considerations 1. Perform hand hygiene immediately before and after any manipulation of the catheter site or drainage bag. 2. Clean the perineal area and catheter tubing in a proximal to distal motion, with foam body cleanser (4:1 body cleanser) or Ready cleanse™ wipes daily and after every bowel movement. The periurethral area should not be aggressively cleansed with antiseptic solutions as this can lead to aggravation and increase the likelihood of infection. The nurse should provide daily reminders to the prescribing provider recommending the removal of the IUC (unless the IUC is still indicated). See Appendix A for indications for continued IUC usage. Provide patient and family education regarding the benefits of removing the IUC. Encourage use of the bedside commode or bathroom within 4-6 hours after IUC removal. 3. For daily care and maintenance, use a chlorhexidine gluconate wipe (CHG) wipe to clean the perineum and wipe down the catheter. If the patient has gross contamination with stool or other body fluids, first cleanse the perineum with 4:1 foam cleanser, followed by CHG wipes. All CHG clothes should be disposed of in the trash, never flushed. When applying lotion, only use CHG compatible products such as dimethicone skin protectant, or calazime ointment. Never microwave CHG cloths, as this will deactivate the CHG.If redness or broken skin such as IAD or burns are present, discontinue use of CHG wipes, as this can further irritate skin. Documentation of use CHG wipes can be done in two places in the EHR. Under the interventions tab in the Hygiene section or under the LDA tab for urethral catheter care. 4. To obtain a urine specimen, clean the sample port with alcohol and aspirate urine using a 10 mL syringe. 5. A sterile, continuously closed drainage system should be maintained. If the catheter must be disconnected from the tubing, disinfect the catheter-tubing junction before separating. c253312 Page 5 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter 6. Empty the collection bag at least every 8 hours, when the drainage bag is 2/3 full to avoid traction on the catheter from the weight of the drainage bag and prior to transporting/ambulating patient to prevent infection. Take care not to contaminate the drainage port by touching the collection container or floor when emptying. 7. When transporting patient, maintain position of drainage bag below the level of the patient’s bladder, to prevent reflux of contaminated urine from the bag to the bladder. Transport personnel should be instructed to wash their hands prior to transporting a patient with an IUC. The catheter bag should be empty prior to transport to prevent reflux. 8. If possible, do not place more than one patient with a urinary catheter in the same room to prevent cross contamination. 9. If IUC is to remain indwelling for greater than 30 days, obtain an order for IUC and bag change at 30 day intervals. 10. Do not irrigate an IUC unless indicated for post urology /genitourinary trauma, surgery, or to relieve obstruction. K. MRI Procedures for Temperature Sensing IUC 1. Bard Latex Free Temp Sensing IUCs and the Latex Temp Sensing IUC are MRI compatible. a. The IUC with temperature sensor should not be connected to the temperature monitoring equipment during the MRI procedure. 2. If the IUC with temperature sensor has a removable catheter connector cable, it should be disconnected prior to the MRI procedure. 3. Electrically conductive material that must remain in the bore of the MRI system should be prevented from contacting the patient through the appropriate use of thermal and /or electrical insulation between the material and the patient. 4. The catheter should be positioned in a straight configuration down the center of the patient table to prevent cross points and conductive loops or coils. 5. The wire and connector of the catheter should be positioned so that it is not in contact with the patient during the MRI procedure. 6. To prevent excessive movement of the clamp located on the outlet tube, the clamp should be fixed in position using appropriate means (e.g. tape). 7. MRI technologists will refer to Conditions 5 and 6 referenced in the current edition of the Reference Manual for Magnetic Resonance Safety, Implants, and Devices by Frank G. Shellock, Ph.D., regarding the Temp Sensing Catheters. References: 1. Ackley, B.J., Ladwig, G.B., Swan, B.A. & Tucker, S.J. (2008). Evidence-Based Nursing Care Guidelines: Medical Surgical Interventions. St. Louis: Mosby Elsevier. (LOE VI) 2. Apisarnthanarak, A., et al. (2006). Effectiveness of multifaceted hospital wide quality improvement programs featuring an intervention to remove unnecessary urinary catheters at a tertiary care center in Thailand. Infection Control and Hospital Epidemiology, 28 (7), 791798. (LOE V) 3. BARD Instructional Video. Preventing UTI: Care and Catheterization Techniques. 2010. (LOE VI). c253312 Page 6 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter 4. Boccola A. Mark, Sharma, Anant et al. The Infusion Method Trial of Void vs. Standard Catheter Removal in the Outpatient Setting: A Prospective Randomized Trial. 2011 BJUI Supplements 3, 43-46 (LOE II) 5. Ingber M, Sandip V, Moore C, et al. Force of Stream after Sling Therapy and Efficacy of Rapid Discharge Care Pathway Based on Subjective Patient Report. 2011 The Journal of Urology 185, 993-997 (LOE IV) 6. Johnson D, Lineweaver L, Maze L.M. (2009) Patients’ bath basins as potential sources of infection: A multicenter sampling study. AJCC 18(1); 31-40 (LOE III) 7. Kleeman S, Goldwasser S, et al. Predicting Postoperative Voiding Efficiency After Operation for Incontinence and Prolapse. 2002 Division of Urogynecology and Reconstructive Pelvic Surgery 187 (1) 49-52 (LOE IV) 8. Lee, Y. Y., Tsay, W. L., Lou, M. F., & Dai, Y. T. (2006). The effectiveness of implementing a bladder ultrasound program in non-surgical units. Journal of Advanced Nursing, 57 (2), 192-200. (LOE III) 9. Lo, E., et al. (2008). Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infection Control and Hospital Epidemiology, 29 (supplement 1), S41-S50. (LOE I) 10. Makic M.B, VonRueden K.T., Rauen C.A., Chadwick J. (2011) Evidence-based practice habits: Putting more sacred cows out to pasture. Critical Care Nurse 31(2); 38-62 (LOE VI) 11. Powers J, Peed J, Burns L, et al. (2012) Chlorhexidine bathing and microbial contamination in patients’ bath basins. AJCC 21(5); 339-342 (LOE IV) 12. Robinson, S. et al. (2007). Development of an evidence-based protocol for reduction of indwelling urinary catheter usage. MedSurg Nursing, 16 (3), 157-161. (LOE VI) 13. Society of Urologic Nurses and Associates (SUNA) Clinical Practice Guidelines Task Force. (2006). Care of the patient with an indwelling catheter. Urologic Nursing, 26(10): 80-81. (LOE VI) 14. Shellock, Frank G. (2011). Reference Manual for Magnetic Resonance Safety, Implants, and Devices: 2011 Edition, pp 267-272, p 407. Biometical Research Publishing Group, Los Angeles, CA . (LOE VI) 15. Sievert D, Armola R, Halm M.A. (2011) Chlorhexidine gluconate bathing: does it decrease hospital-acquired infections? AJCC 20(2); 166-170 (LOE I) 16. Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for Prevention of Catheter-Associated Urinary Tract Infections: Healthcare Infection Control Practices Advisory Committee (HICPAC). 2009 pp 1-67. Available at: http://www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf (LOE V) 17. Hooten TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases 2010;50:625-663. (LOE V) 18. Gray M. Reducing catheter-associated urinary tract infection in the critical care unit. AACN Advanced Critical Care, 2010;21(2):247-257. (LOE V) 19. Parker D, Callan L, Harwood J, Thompson DL, Wilde M, Gray M. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: Part 1: Catheter selection. J Wound Ostomy Continence Nurs.2009;36(1):23-34. (LOE V) 20. Willson M, Wilde M, Webb ML, Thompson DL, Parker D, Harwood J, Callan L, Gray M. Nursing interventions to deduce the risk of catheter-associated urinary tract infection: Part 2: c253312 Page 7 of 9 Insertion, Removal and Care of an Indwelling Urinary Catheter Staff education, monitoring, and care techniques J Wound Ostomy Continence Nurs. 2009;36(2):137-154. (LOE V) c253312 c253312 Page 8 of 9 Appendix A Algorithm for Appropriate Insertions of Indwelling Urinary Catheters Admission/Shift change assessment of Urine Output Management Is there a need for an indwelling urinary catheter? Please read the following criteria for appropriate use of Foley catheter and check your reason for ordering the Foley catheter for this patient. Drainage: Urinary obstruction (distal urinary tract) Urinary retention (not managed with intermittent catheterization) Monitoring: Alteration in the blood pressure or volume status (unstable patient) requiring urine volume measurement. Accurate monitoring of intake and output in a patient unable to cooperate with urine collection by other means. Peri-procedure: Preoperative insertion for emergency surgery Major trauma patients Placement by urology for procedure or surgery Therapy: Continuous bladder irrigation Management of urinary incontinence with stage 3 or greater pressure ulcerations Comfort care for the terminally ill YES, the reason appears above. NO, the reason does not appear Insert catheter above. (A catheter may not be indicated for this patient.) Consider: Re-evaluate continued need each shift. Consider removal if indications no longer met. 1. 2. 3. 4. 5. 6. c253312 Straight Catheterization (for Sterile specimen if needed) Commode Urinal Bed pan Incontinence Pads Toileting with assistance Page 9 of 9