Medical versus Surgical Insertion of Peritoneal Dialysis Catheters
advertisement
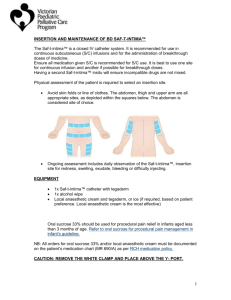
A54(W) MEDICAL VERSUS SURGICAL INSERTION OF PERITONEAL DIALYSIS CATHETERS: A RETROSPECTIVE COHORT STUDY Namagondlu, G1, Yiu, V2, Hiemstra, T2, Williams, P1,2. 1 Nephrology, Ipswich Hospital, Ipswich, 2Division of Renal Medicine, Addenbrooke's Hospital, Cambridge INTRODUCTION AND AIMS: Mandatory training in peritoneal dialysis (PD) catheter insertion is not a requirement of the current UK curriculum. The number of catheter insertions by nephrologists (medical insertion) is declining, and many renal units now rely exclusively on general or transplant surgeons for catheter insertion. Urgent surgical cases often take precedence, and increase waiting times for catheter insertion. In patients with rapidly declining renal function, such delays may necessitate haemodialysis and contribute to attrition of PD programmes. We compared the safety and efficacy of medical versus surgical PD catheter insertions in a single-centre (Ipswich Hospital) cohort study. Medical Insertions of PD catheter are performed using Trocar and Cannula method at Ipswich Hospital. METHODS: We performed a retrospective cohort study of medical insertion (MI) versus surgical insertion (SI) of PD catheters, performed at a single centre between January 2007 and December 2009. Data were abstracted from an electronic database and patient case records. The primary endpoint was catheter patency after 12 months. Patency rates were compared with international audit guidelines.1 Data are presented as mean (SD) or median (IQR) as appropriate. RESULTS: We identified 32 catheter insertions in 31 patients during the study period, of which 23/32 (72%) were MIs. Age did not differ between groups. More MIs were male (19/23) compared to SIs (3/9, P=0.013). One patient in the MI group died within 12 months, and 1 patient from each group received a kidney transplant. Of the remaining patients, 2/7 (29%) SIs and 0/22 MIs (7% overall) were no longer patent after 12 months (P=0.052). Combined Catheter patency at 12 months (censored for death and transplant) was 93% (ISPD recommendations suggests >80%). The mean eGFR at the time of catheter insertion was 7.7ml/min for MIs in comparison with 8.1ml/min for SIs. In our centre the time from listing to catheter insertion is usually significantly shorter for MIs(2-3weeks) compared to SIs (4-6 weeks). All MIs were performed under local anaesthetic. Rates of Immediate complications (less than 4 weeks) were similar in both the groups and comparable to ISPD recommendations. CONCLUSIONS: The combined data from all insertions at our centre compare favourably with ISPD recommendations. There was no significant difference in patency rates between surgically and medically inserted catheters. Waiting list times are shorter, with a lower requirement for general anaesthetic in patients receiving MIs. Our data indicate that medical insertion of peritoneal dialysis catheters is equivalent to surgical insertion in terms of safety and efficacy. We suggest that promotion of and training in medical insertion of peritoneal dialysis catheters is not only justified, but may provide benefit to patients 1. Figueiredo A, Goh BL, Jenkins S, et al. Clinical practice guidelines for peritoneal access. Perit Dial Int 2010;30(4):424-9.