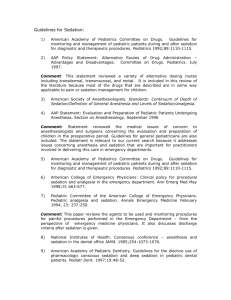
Pediatric Sedation Newsletter – March, April 2002
advertisement

Pediatric Sedation Newsletter – March, April 2002 Departments of Anesthesiology and Pediatrics, Dartmouth Hitchcock Medical Center, Lebanon, NH Editors: Joseph Cravero MD (joseph.cravero@hitchcock.org), George Blike MD george.blike@hitchcock.org Website = http://an.hitchcock.org/PediSedation/ Circulation 3022 Correspondence: In the last issue we asked our readers what type of sedation they provide for children undergoing abdominal CT scans with enteral contrast. We received several responses – I will reprint two here that are representative of the variety of opinions we received. #1 Letter: The last Sedation newsletter asked for input about abdominal CT scans with contrast and sedation. We have taken the approach of instituting a protocol (using propofol sedation) for patients who need sedation during such scans and then using our Sedation Unit database to look for complications. Our protocol is as follows. 1. The patient must have no GI obstructive symptoms, nausea, or vomiting. (This essentially reduces the candidate pool of patients to asymptomatic tumor follow-up patients) 2. If the patient will drink the contrast, they are given it 2 hours before the scan. (Sounds similar to your experience but unfortunately most of our patients that need sedation for a short CT scan are not of a mind to cooperate by drinking either) 3. If the patient will not drink the contrast, the patient is sedated first. An NG is placed and the contrast (we have negotiated a reduced volume with our Radiologists) is given by gravity. The patient stays sedated with their head elevated for about 30 minutes before being scanned. Our sedation unit statistics show that the biggest risk in our hands of needing to bag the patient is with initial institution of sedation. This approach of giving the contrast after sedation of course does not eliminate the risk of aspiration if the patient gets into trouble later but at least decreases the known highest risk period. We have performed 64 contrasted abdominal CT's in this manner since the middle of 2000 and compared the incidence of any of our predefined complications to abdominal CT's without contrast and sedation patients as a whole. Three patients with contrast had decreased O2 saturation that responded to increased FIO2, two patients exhibited mild stridor that responded to head positioning during the scan. This comes out to about an 8% incidence of any complication compared to our 6% incidence overall and 3% in the non-contrasted abdominal CT patients. We have had no incidence of problems during the contrast administration period. Numbers are small and we're playing with fire but so far so good. I'll be interested in hearing what other institutions have done. Thanks, Lia Lowrie, MD (Pediatric Critical Care Medicine) # 2 Letter: Joe, With regard to the sedation and oral contrast issue, this has been a hot one for many years. I will tell you what we do, but it is based solely on experience and not on science. In patients in whom we have to give oral contrast we ask them to arrive in radiology early and have them drink the contrast - we then sedate them - we don't wait 2 hours because the contrast is too far along - usually the delay is not longer than 15 minutes. Now the question is how safe is this practice. We have not had (in the 18 years that our nursing chief has been here) any "significant" aspiration. I am sure that some patients have vomited, but in light of the chloral hydrate or sodium pentobarbital sedation (both of which I consider deep sedation) we have had no recognizable complications and we have followed this policy in thousands of patients. Yes, I know that many of these are elective, but again, it is hard to argue with success. I know from having been at Cincinnati Children's Hospital for many years that they do it the same way and they have experience with thousands of patients as well. I will be interested to hear the nay-sayers from the anesthesiology perspective. George Bisset MD (Pediatric Radiologist) Comments and Summary: Several other letters from non-anesthesiologists described similar protocols. Clearly there is a difference in the “delay” time between administration of contrast and the performance of the scan in different medical centers. This seems to be due to variances in exactly what people are looking for on the scan and the preference of each radiology department. We also had many individuals comment on how frequently children will refuse to drink all the contrast. Like Dr. Lowrie, many providers sedate children for placement of the NG tube in cases where children will not drink. Almost all of the institutions that responded allow sedation without airway control after oral contrast administration in one way or another – all exclude certain high-risk groups such as those with possible bowel obstruction. Interestingly, we did not receive many notes from anesthesiologists so it is hard to give a good idea of how this segment of the sedation community feels about this issue – but that will not stop us……. We asked the question of how best to manage these patients with anesthesiologists at our own institution and others. We believe there are still two camps among anesthesiologists when it comes to this particular “full stomach” issue. About half of the anesthesiologists polled would sedate these children without securing the airway and half would intubate any child in this clinical scenario. When pressed about their answers, most anesthesiologists recognize that this situation may not be exactly similar to the situation presented by the consumption of food, and therefore the dictates of our usual protocols for “NPO” may not be absolutely appropriate. Clearly, the implication here is that these providers are weighing the relative risks of intubation (low in expert hands) with the risk of aspiration in this situation (apparently low as well). After careful consideration of these opinions, we are not really surprised by the comments we have received. Anesthesiologists are familiar with the equipment, techniques, and drugs used to perform intubation in a way that radiologists (and most other specialists) may not be. Therefore the choice of securing the airway with an endotracheal tube does not present a significant logistical difficulty – and is very low risk. In cases such as this (where there is no clear data to determine the appropriate course of action), intubation may actually represent the course of greatest familiarity and comfort for anesthesiologists. Conversely, sedation without securing the airway may represent the only feasible answer to this clinical need and (in the absence of any reports of serious injury) may be cost effective and appropriate for services struggling to accommodate a large number of these procedures without the ready availability of anesthesia expertise. We have not been able to find any large reported series of these procedures, so Dr. Lowrie’s data may be the best we have at the moment. The numbers are so small it is really hard to say much about safety; but the lack of any reports of serious problems in institutions performing thousands of these procedures makes us think that the incidence of aspiration is indeed very low even without securing the airway. In the final analysis, we have no clear recommendations for practice based on the collected opinion of our readership. It would be safe to assume, however, that you have plenty of company if your institution is performing oral contrast CT scans with sedation in the absence of airway control (with exclusion criteria for very high-risk patients). Those who choose to intubate all patients for these procedures (we believe) are also not alone. Only time and large multicenter trials will tell us if there is truly added safety to this practice. Next Question: As anesthesiologists, we are frequently faced with the decision of what to do with the neonate or very young infant who has received anesthesia. There is good data to indicate that the incidence of post-anesthesia apnea and bradycardia is significantly increased in the youngest (less that 2 week old) term neonates, and in the former premature infants under 55-60 weeks post conceptual age. We are also asked to care for similar patients having sedation for diagnostic procedures. We would like to know how the readers of this newsletter handle these patients. Are there any age criteria that cause you to keep a patient in the hospital after “sedation” to observe for apnea or bradycardia? Are former prematures considered differently than term infants in your practice? Please send us your thoughts and we will condense them for the next newsletter. Literature Review: The correlation of the bispectral index monitor with clinical sedation scores during mechanical ventilation in the pediatric intensive care unit. Author: Berkenbosch JW. Fichter CR. Tobias JD Anesthesia & Analgesia. 94(3):506-11; 2002 Mar. Abstract: In patients who are mechanically ventilated in the pediatric intensive care unit (PICU), sedative and/or analgesic medications are routinely provided and titrated to effect based on clinical assessment of the patient. The bispectral index (BIS) monitor uses a modified electroencephalogram to quantify the effects of central nervous system-acting drugs on the level of consciousness. To evaluate the usefulness of the BIS monitor to predict clinical sedation levels in the PICU, the authors compared BIS values with simultaneously obtained clinical sedation scores in 24 mechanically ventilated pediatric patients aged 5.7 plus minus 6.1 yr. For each sedation scale used, the BIS value correlated with increasing depth of sedation (P < 0.0001) and was independent of the drug(s) used for sedation. To differentiate adequate from inadequate sedation, a BIS value <70 had a sensitivity of 0.87--0.89 and a positive predictive value of 0.68-0.84. To differentiate adequate from excessive sedation, a BIS value <50 had a sensitivity of 0.67--0.75 and a positive predictive value of 0.07--0.52. We conclude that the BIS monitor may be a useful adjunct for the assessment of sedation in PICU patients. IMPLICATIONS: We demonstrate the usefulness of the bispectral index monitor for assessing sedation in pediatric intensive care unit patients. The bispectral index monitor correlated with clinically assessed sedation levels and was useful for differentiating adequate from inadequate sedation, which would be of value when the clinical examination is unavailable. Commentary: Since the advent of the practice of sedation and anesthesia, there has been a search for the “Holy Grail” of consciousness monitoring – a simple machine that could indicate how deeply “asleep” a patient is at any time. The bispectral index monitor (BIS) is currently the most widely used “depth of anesthesia” monitor. As described in the abstract above, this monitor is designed to process an EEG signal into a single number (0-100) that indicates depth of unconsciousness. This instrument has been aggressively marketed to anesthesiologists and there is a wealth of literature on its use in the OR setting. We can not even begin to summarize all the findings of these studies involving BIS technology but we believe it would be fair to say that the instrument “works” as a consciousness monitor; it is less clear as to whether or not it really improves anesthesia delivery to a significant extent. Among some anesthesiologists and institutions the BIS is used as a “standard” monitor and is applied to most patients, while in other locations it has been slow to catch on. (At our institution, it is used in 10% or fewer cases). The study described above represents a trial of the monitor in the pediatric ICU setting, and should be commended for taking on this complex issue. The authors try to answer the questions as to whether this monitor of consciousness can work in the pediatric ICU environment and how its performance compares to standard sedation scales. They also compare the performance of the BIS in the ICU to that in the OR. As with many ICU studies, difficulties in methodology include the variety of patient pathology that is involved, lack of true “blinding” during data collection, and relatively small numbers. The results indicate that the monitor is relatively good at identifying inadequate sedation but fairly inaccurate for indicating “over sedation”. It does track well with clinical sedation scores. Interestingly, opioids appear to affect the BIS reading more in the ICU setting than in the OR – a finding which may relate to the degree of illness these patients were experiencing compared to elective surgery patients. Of note, the discussion section is worth reading for anyone interested in the emerging field of sedation depth monitoring. The authors recognize the limitations of their work and put forth reasonable arguments for their conclusions. After reading this paper we are left with the question, "What is the future of the BIS in pediatric sedation?" The authors of this paper suggest that in ICU patients receiving muscle relaxants, the monitor could be used to assure adequate depth of sedation (since these patients can not be assessed clinically). Unfortunately, based on the results of this study, the BIS would not be very useful for warning us about too much sedation. It is not certain that this monitor offers much advantage over clinical evaluation in patients who are not relaxed. The question for providers of pediatric sedation outside the ICU would be whether or not a monitor such as the BIS could be used to “titrate” sedation to a given number and avoid the need for provocative testing of sedation depth ( i.e. “Johnny can you hear me?”). Stay tuned, as we are sure this will be the thrust of future investigations in this area. Please let us know about any experience you have with the BIS and sedation monitoring! Close Call and Critical Incident Reports We invite those receiving the newsletter to submit cases to this "Close Calls" section aimed at the key safety issues associated with providing pediatric procedural sedation. The cases have been "sanitized" such that the date, patient identifiers, institutional identifiers, provider information, etc. will not violate the privacy of the patient or care providers. Case #10 A 6yo child with a seizure history needed an MRI scan performed. At the reporting institution, pediatric MRIs are performed with propofol sedation. The sedation team elected to induce anesthesia in an “induction room” at a location a short distance from the MRI scanner using nitrous oxide and then sevoflurane. This was uncomplicated. Within 5 minutes an IV was placed, nitrous oxide, sevoflurane stopped, and propofol started intravenously. An MRI compatible pump was being used that had excellent performance in the MRI scanner area. It was much more accurate than using a propofol gravity drip or other available syringe pump technology. The child was transferred to the MRI gurney and monitors placed (EKG, SpO2, CO2, NIBP). A warm blanket was place on the child and a Velcro strap used to secure the child’s arms. Deep sedation was being performed with IV propofol. No airway was required, and the child had no airway obstruction or snoring. A button was pushed that automatically “loads” the patient into the scanner bore. As the child was deep into the scanner, the IV tubing was noted to be under tension “like a guitar string” and a senior anesthesia provider told the MRI tech to stop the patient’s entry as the IV was going to be pulled out. The MRI tech did not hear the anesthesia provider due to noise. The anesthesia provider did not know how to stop the gantry from moving into the MRI tube so he unclamped the IV pump from its pole and moved it into the scanner to relieve tension on the IV tubing. As he did, the pump flew into the scanner. The outcome is withheld at the request of the submitting organization. Comments: This case highlights important issues regarding hazards of providing sedation in the MRI environment. It would be easy to attribute this case to “incompetent anesthesia provider” or “dangerous IV pump” - this hazard is common to all institutions providing MRI imaging (i.e., this could happen to all of us). We will address several points: 1) terminology as a hazard; 2) “invisibility” of hazards; 3) behaviors as a hazard; and 4) using a behavioral rule-based countermeasure to reduce risk and improve safety. 1) Terminology as a hazard. We all know that metal objects should not be brought into the MRI scanner room. When we asked an MRI expert what “MRI compatible” meant, we received an answer that was different from that given by the anesthesiologists and nurses who support patients medically while being scanned. The radiologists described materials that fall into three categories: a) “truly or completely MRI compatible” - like plastics that are inert and safe anywhere in the room including the center of the magnetic bore; b) “MRI incompatible” - need to be outside the 10 gauss line as they are highly magnetic and will become high velocity projectiles depending on their weight and other physical properties when close enough to the bore; and c) “mostly MRI compatible” - which includes a large variety of items made of materials that are weakly magnetic; magnetic but fixed to a non-movable object; composite of non-magnetic and magnetic components; or compatible from a magnetic point of view, but nonfunctional in the magnetic field. In contrast to this detail, sedation providers could identify only two categories, “compatible” and “not compatible.” In this case, the IV pump was classified as “mostly MRI compatible”. The company had referred to it as compatible in terms of function, but advised that it should be fixed to a pole and no closer than a certain magnetic field. A label on the pump read as follows: May be used in static magnetic fields up to 150 Gauss When Secured to Non-Movable Object. We tested the pump using our 1.5 Tesla shielded MRI system and found this pump is much less magnetic than our Bard infusion pump that was being used prior to procuring this pump. Ironically the Bard stops working a great distance from the bore and omits a continuous tone indicating it is “locked up”. Sedation providers are therefore not tempted to bring the pump too close to the magnet. The new pump is much safer in that dosing and delivery are superior to the Bard when held much closer to the magnet; however this led clinicians to assume it was safe to bring it very near to the bore. We currently use this pump and have fixed a new, more detailed label to it. We also have tried to make the sedation providers more aware of “mostly compatible” objects in the scanner room that we need to be mindful of (laryngoscopes, stethoscopes, glasses, endotracheal tube stylets, etc.) Device will become FLYING OBJECT @ 5feet from scanner 2) Invisibility as a hazard. In this particular case, the pump was not magnetic if you tested it with an external magnet on the components. However, when we talked to the company and checked some of the internal components, it became clear that the battery pack (which is custom made and has a chip included so that battery charge can be displayed) is the magnetic component that allowed the pump to become a flying projectile. In addition, the magnetic field is “invisible”. At our hospital we have two MRI scanners that are 1.5T, but are now going to acquire a 3T magnet. Our radiologists could not immediately tell us where the field was “150 gauss”. To address this issue we consulted the experts at our institution and have put a line on the floor of the room to signify the 10 gauss line and are working on a 100gauss line. We also have added a magnetic chain to the pump such that the chain pulls towards the bore when you are getting too close (a tell-tail of sorts). 3) Hazardous behavior and 4) Behavioral rules as a safety intervention. Ultimately, we found it is not a simple matter to determine what is safe and unsafe in the MRI scanner, what objects you can bring into the scanner, or how close you can come to the bore. We are left with the question of what can we do to create a safer care system? We have chosen to assume that all items we use in the scanner are only “mostly compatible”. We therefore have recommended that it is NEVER SAFE TO GO INTO THE BORE to manage a situation, but rather we should ALWAYS BRING THE PATIENT OUT…no matter how severe the situation. We have labeled the buttons and components of the patient gantry to facilitate this behavior and strategy. We have also developed a short video that has been sent by e-mail to all sedation providers to allow all of us to learn from this type of case before it happens to us. NOTE-This is a new link changed and updated 1/30/03. To play the digital-streaming movie, click rtsp://april.dartmouth.edu:554/ray/MRI_CC4.rm The button to eject a patient is now labeled clearly. The handle that disengages the gantry allowing the patient to be pulled out rapidly is also labeled and demonstrated on the video. PUSH BUTTON to EJECT PATIENT TWIST and PULL (to remove patient) Conclusions: As a result of this report, we hope to alert sedation providers to one of the hazards associated with working in the MRI environment. Thanks for submitting reports; please keep them coming so that we all can learn from them.