NTG - Energeyes Association
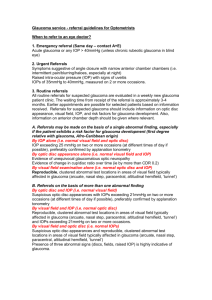
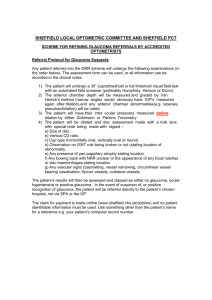
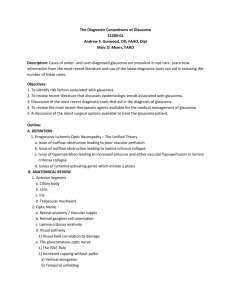
advertisement
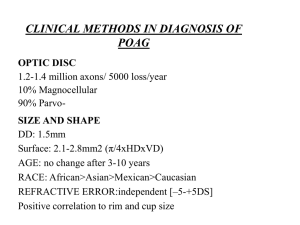
GEORGE T. BANYAS, OD, FAAO High pressures Rim defects, typically Pre- perimetric defects Classic field defects Typically no ocular or systemic history Family history Race Low pressures Normal anatomy Often good discs since slowly progressive Masquerade syndrome? No symptoms until late in disease Is it really glaucoma? Africans Elderly High myopes/ large disc Elevated IOP Positive family history Low systolic BP with reduced perfusion Thinner central corneas Autonomic dysregulation Untreated IOP typically < 21mm Open , non-pigmented filtration angles Acquired progressive “glaucomatous” injury Progressive “glaucomatous” field loss Females, autonomic dysregulation A different type of optic neuropathy? 1/3 of glaucoma patients possess NTG 1/3 of NTG patients have unilateral cupping Progression is slow. No hasty decisions! Chairside presentation will always include IOP 21 or less Systemic disorders not required Systemic disease may be the cause Juvenile optic atrophy Simple congenital optic atrophy Recessive optic atrophy Leber’s disease (through age 80) Burned out pigmentary glaucoma Past history of steroid use Severe blood loss/cardiac surgery Post –traumatic optic neuropathy Old BAO Systemic beta blocker use Past subdural hematoma Old ION Posterior ciliary infarct Intrasellar tumor Syphilitic optic neuritis RBON Subacute angle closure Nocturnal hypotension Systemic beta blocker use Toxic optic neuropathy Compression ( pituitary adenoma, meningioma) Sleep apnea (low O2 partial pressure) Diurnal or nocturnal IOP swings Pachymetry under 550 um Pigment dispersion or pseudoexfoliation Compression by ICA or anterior cerebral artery ICA and anterior cerebral disorders - abnormal juxtaposition - sclerosis - aneurysms - pituitary tumors, craniopharyngiomas, meningiomas , sarcoidosis, Wegener’s MRI with contrast is the imaging mode of choice for sellar and chiasmal lesions Intracavernous sinus lesions - thrombosis/ blood dyscrasias -infection - ICA aneurysm - inflammation Company kept includes III, IV, VI, V1, V2, and oculosympathetic fibers. IF note a Horner’s in unilateral “NTG” eye, must R/O cavernous s. Sarcoid, pseudotumor Acromegaly (pituitary hypersecretion of HGH) Paget’s disease – 1% of adults over 50, may see angioid streaks Pial vessels, posterior ciliary and short posterior ciliary vessels, CRA, ophthalmic a. Thrombosis, inflammation, autonomic dysregulation, infection , metabolic syndrome resulting in ischemia genuine ischemic optic neuropathy Sarcoid Autoimmune disease Anemia Hypotension Hypertension/diabetes Vasospasm Paraproteinemias Hyperhomocysteinemia RETINA - perfusion retinal arteries - retinal veins – CRV – cavernous s. UVEA/ciliary body – aqueous outflow 2 long posterior ciliary arteries - several anterior ciliary arteries – short posterior ciliary arteries choroidal plexus – vortex veins – superior and inferior orbital veins – cavernous s. Sclera/episclera/conjunctiva/canal of Schlemm anterior ciliary arteries – surface arterioles - venous plexus of sclera/episclera/conjunctiva – anterior ciliary veins – inferior/superior orbital vein – cavernous sinus Wax and Associates found high titers of antibodies against retinal proteins - rhodopsin - heat shock proteins C/D may be meaningless Large disc has large cup Small disc has small cup Average size disc is consistent with 5 degree spot size on direct Disc size does not determine susceptibility to glaucoma Normal disc shape is oval Vertical diameter is 10 degrees greater than horizontal Optic disc shape does not increase susceptibility High astigmia may alter appearance Thickness – inferior -> superior-> nasal-> temporal ( ISNT rule ) Inferior and superior temporal rim effected first With advanced glaucoma, only nasal sector remains So, vertical margins effected first Various shades of pink and symmetric Pseudophakes appear more pale If advanced, pallor more an artifact due to excavation Pallor that exceeds cupping requires neuroophthalmic work up Rarely, pallor may exceed cupping Cup is defined by contour , not color Stereoscopic viewing Disc shape is vertical, however cup shape is usually horizontal Place emphasis on the rim! Glaucoma experts assess disc better than OCT! Disc hemorrhages are not typically normal Detected in less than 8% of glaucoma patients Greater association with NTG than other glaucomas Indication of progression Peripapillary chorioretinal atrophy may be associated with glaucoma Central beta (RPE atrophy and visible choroidal vessels) Peripheral alpha (pigmentary changes and CR atrophy) Greater with damage? A.D. disc drusen may result in NFL loss and field defects identical to glaucoma Disc drusen might mask cupping Single most common cause of glaucoma without cupping B scan or auto fluorescence to diagnose Crescents Tilts Physiologic differences Very slow progression Disc drusen Most early cases will be missed! Add FDT screening fields and may capture a few Perform routine pachymetry and may capture some Add threshold perimetry and may capture a few more Discs that do not respect ISNT caught Managing a condition with unknown pathogenesis May be secondary to systemic disease Systemic disease may result in morbidity/mortality if not managed Disorder may progress regardless of your intervention Very good history - previous history of any IOP elevation - ocular trauma/ inflammation/ steroid use -sleep apnea (may need to ask spouse) -nocturnal BP dips - erectile dysfunction drugs -hemodynamic crisis (blood loss, hypotension, anemia, syncope, blood transfusions, surgery (usually open chest) Weakness in extremities, dizziness, headache, loss of consciousness, diplopia Color vision testing, ruling out dyschromatopsia, particularly if asymmetric cupping Pupil testing Systemic medications Gonioscopy CBC to rule out anemia ESR – rarely elevated, but more to R/O ION RPR, if positive then FTA-ABS ANA to rule out collagen vascular AP Abs, rhodopsin Abs, HSP Abs Serum immunofixation for monoclonal gammopathy….10% of NTG patients C reactive protein…. Often high in NTG Chest X-ray to rule out sarcoidosis, superior vena cava obstruction Carotid Doppler to rule out carotid insufficiency Scanning Which one? - the anatomic site - the pathophysiology - the cost Who should order? - the person treating - suggestions are welcomed Disc drusen – CT CT for Grave’s – axial and coronal views with contrast CT for vascular abnormalities – varices, hemangiomas, and lymphomas Pseudotumor – CT or MRI Optic nerve tumor – MRI with fat suppression and contrast * Contrast presumed in all instance of CT MRI is choice for sellar and chiasmal lesions Craniopharyngiomas, pituitary adenomas, and meningiomas Intracavernous lesions – look for constriction of the carotid arteries ICA or anterior cerebral artery abnormalities MR angiography – evaluates flow CT angiography – evaluates blood volume Either good for aneurysms Can not definitively R/O aneurysm Not good for lesions < 5mm Catheter angiography is still the gold standard Done before gonioscopy Preferably before dilation At least two hours after awakening Stability following contact lens wear? Normal population 544+ 34um 2.5-3.5mm per 50um 3 readings with SD of 5um or less 37 published studies have demonstrated CCT is a risk factor for progression to glaucoma German study determined relationship between CCT and field loss NTG patients tend to have thinner CCT “thin” cornea may be masking POAG Optic nerve photos before LASIK? Structural changes before functional changes OHTS demonstrated 93% chance of not developing glaucoma with normals Greatly expanded database heightens sensitivity May identify changes in visual fields up to 8 years earlier Disc and nerve fiber layer Baseline images to compare patients to norms Detection of progression may disagree with perimetry Irregularities, even before field change may be predictors Still possible to have field loss before structural changes! Functional changes may precede structural Diagnostic ability demonstrated to be less accurate than disc assessments by a glaucoma specialist Tells how much tissue is there, but is it healthy 5,000 axons lost on average per year Variable normal disc topography Specificity not 100% for glaucoma Required! Possible to have field loss before structural changes C30-2 SAP SWAP may provide earlier diagnosis – stimulus V blue (440 nm) on yellow, that’s about all FDT matrix may provide earlier diagnosis than SWAP and SAP. That’s about all Right field is WNL. Left finds correlation between the two Not looking for: Focal defects are not uncommon Defects are closer to fixation often Defects are deeper Less slope from seeing to non-seeing Collaborative NTG Group Study showed slow or non-progression in NTG Risk factors such as migraine or disc hemorrhage should be followed closely With conclusive demonstration of progression consider treatment 50% of eyes without progression showed no progression by 7 years Reduce IOP 30% Assess ocular environment Most common comorbidity in glaucoma patients is dysfunctional tear syndrome DTS present in 8-20% of population Topical glaucoma therapy daily, for years, may further compromise the surface 48% of glaucoma patients report mild to severe symptoms Would you give a pill to someone that can’t swallow? Nafl tear BUT Corneal/conjunctival staining Meibomian gland inspissation Anterior blepharitis - Steri-lid HS - warm compresses/massage - antibiotic or antibiotic/steroid ung HS - soft preserved tears daytime Posterior blepharitis - Steri-lid HS - warm compresses/massage - steroid/antibiotic ointment HS x 1-2 weeks - cyclosporin BID if MGD appears primary - doxycycline 100mg QD - omega 3’s ( fish oil/flax), good hydration - soft preserved lubrication daily 60 times better penetration than other topical antibiotics Topical 1% solution (Azasite, Inspire Pharma) Warm compresses/massage with 1% Azasite BID x2days, then QD x 12 days Well documented anti-inflammatory activity 75% of patients Macrolides have demonstrated antiinflammatory properties by inhibiting MMPs Lacrimal gland disease - soft preserved tears daily such as Systane - gels HS - consider cyclosporin - omega 3’s, good hydration - question systemic medications - plugs Canthal tendon laxity - poor tear ejection - ectropion - floppy eyelid syndrome Conjunctivalchalasis Pinguecula EBMD – muro 128 drops/ung/debridement Allergies - Patanol BAK – a detergent that disrupts cell membranes - reduced TBUT -conjunctival fibrosis - concentration-dependent cell mortality - goblet cell reduction/loss of microvilli - basement membrane damage - not all patients suffer Benzododecium bromide – timolol gel Purite – brimonidine Sofzia – travoprost Newer reduced concentration - Lumigan 0.1% Unit doses - Timoptic - Zioptan - Cosopt PF Shown to lower IOP 15-30% in NTG Interestingly, not utilized in the CNTGS Little circadian variation in IOP Some work better than others in some patients non-BAK option – Travoprost/Zioptan Could exacerbate inflammation with OSD Travoprost has shown efficacy beyond 24 hours DuBiner et.al. observed IOP significantly reduced out to 84 hours. Sit et.al. showed efficacy 41-63 hours Peace et.al. showed travoprost with and without BAK effectively lowered IOP at all times out to 60 hours Partially reversible after a few months Safe systemically, really, but use Betoptic QD dosing usually enough Should be reconsidered for NTG. Possible reduction in perfusion to disc, where Betoptic shown to possibly enhance optic nerve perfusion OK for patients with asthma. Clear with their physician first. May be neuroprotective (increased ganglion cell survival in rat optic nerve crush injury) Concern about reduced perfusion Good peak effect, reduced trough effect with short duration of action Less effect between midnight and 6 a.m. Tachyphylaxis / allergy Dorzolamide – increased retinal blood flow in humans Brinzolamide (Azopt, Alcon) Better 24 hour efficacy vs. B blockers or alpha agonists Diamox – may be necessary when intervening in surface disease May be better adjunctive drug to use with prostaglandins Prostaglandins and…… CAI> alpha agonists> beta blockers Prostaglandins + CAB Cosopt – dorzolamide /timolol maleate Xalacom – latanoprost / timolol (not here) Combigan – brimonidine / timolol (adjunct) travoprost/timolol - (not here) the presence of beta blockers might contraindicate use with NTG Antihypertensives in AM Seek to maintain diastolic no less than 80mm Tell MD to change their regimen or else Non-adherence to medications Inability to lower IOP 30% Impression of greater diurnal shift Surface disease Progression Cognitive impairment Patient characteristics Provider characteristics Characteristics of the medical regimen Situational/logistical factors, including cost Difficulty detecting non-compliance Non-compliance increases with increasing meds, dosages Tsai and colleagues identified 20 specific barriers that patients reported interfered with using glaucoma meds Provider communication and concern about future consequences drive adherence 13,956 patients 89% claimed taking meds daily Medication possession ratio revealed an average of drug taken 64% of time Drug taking ranged from 36% of time to 100% of time Only 10% fit the 100% category Google OHTS risk calculator I phone app for glaucoma risk calculator LET’S EAT!