Pulmonary Artery Catheters
advertisement
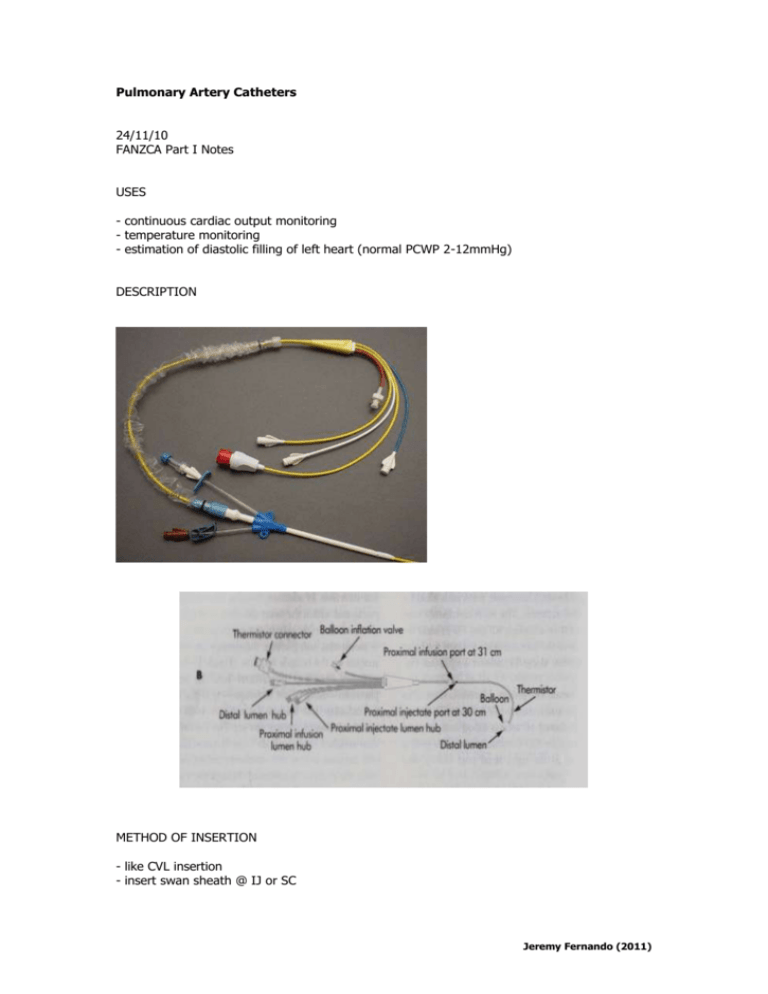
Pulmonary Artery Catheters 24/11/10 FANZCA Part I Notes USES - continuous cardiac output monitoring - temperature monitoring - estimation of diastolic filling of left heart (normal PCWP 2-12mmHg) DESCRIPTION METHOD OF INSERTION - like CVL insertion - insert swan sheath @ IJ or SC Jeremy Fernando (2011) - SVC/RA Pressure Length 0-6mmHg 15-17cm - inflate balloon with 1.5mL of air - tricuspid valive - RV - pulmonary valve diast syst - PA 25 0-25 35 5-15 15-30 2-10 40-50 - look for pressure waves to change OTHER INFORMATION Wedging - PA catheter tip -> small pulmonary artery (usually in RML or RLL) phasic blood flow & pressure ceases static column of blood between catheter tip & LA must be in West Zone III otherwise trace will show respiratory swing. checking in West Zone III: -> -> -> -> -> PAWP < PADP PAWP alters < than 50% of applied PEEP PAWP increases by < 50% of changes in alveolar pressure O2 saturation in wedged position greater than unwedged position (sucking back of oxygenated blood) CXR: below level of LA Thermal Dilution - injection of cold fluid - recording of change in temperature with time - advantages: cheap, non-toxic, arterial puncture avoided, absence of re-circulation - disadvantages: requires insertion of PAC, mixing with venous blood may be incomplete, PA blood flow varies greatly with respiration - causes of inaccuracies: catheter malposition, injection mistakes (volume, speed, temperature), inaccurate thermister, TR, intra-cardiac shunts, wrong computation constant Jeremy Fernando (2011) Measured values - Q: 4-8L/min CI: 2.5-4L/min CVP: 2-6mmHg PAWP: 8-12mmHg PAP: 25/10mmHg SvO2: 0.65-0.70 Temperature Derived values – use of formula: Q = MAP-CVP/SVR - SV: 50-100mL/beat SVI: 25-45mL/beat/m2 SVR: 900-1300 dynes-sec/cm5 SVRI: 1900-2400 dyne-sec/cm5 PVR: 40-150 dyne-sec/cm5 PVRI: 120-200 dynes-sec/cm5 Pulmonary Artery Wedge Pressure - PAOP or PWP = pressure within the pulmonary arterial system when catheter tip ‘wedged’ in the tapering branch of one of the pulmonary arteries. - in most patients this estimates LVEDP thus is an indicator of LVED volume (preload of the left ventricle) - normally 6-12mmHg (1-4mmHg less than the pulmonary artery diastolic pressure) - normally measured at the end of expiration - PCWP 18-20mmHg in the context of normal oncotic pressure -> APO likely Jeremy Fernando (2011) CIRCUMSTANCES WHEN PCWP > LVEDP - MS atrial myxoma pulmonary venous obstruction (fibrosis, vasculitis) MR non-zone III placement L to R shunt COPD IPPV +/- PEEP CIRCUMSTANCES WHEN LVEDP > PCWP - left ventricular failure raised intra-thoracic pressure (high PEEP) non-compliant LV AR COMPLICATIONS Early - arrhythmias heart block (6% RBBB) infection knotting pulmonary infarction hypotension hypoxia PA rupture air embolism valve damage Late - thrombosis PA rupture sepsis endocarditis ARGUMENTS FOR - in some populations (high risk cardiac surgery) helps to delineate different forms of shock. - may facilitate the early diagnosis of shock (ie. young patients that can maintain MAP in the face of decreasing Q). - if IABP used can still delineate Q (unlike PiCCO) - other monitors also have little data to support their use. - PACMAN study showed they were safe in non-cardiac patients admitted to ICU. ARGUMENTS AGAINST - risk of major vessel injury with large bore introducer sheath insertion for PAFC. Jeremy Fernando (2011) - risk of pulmonary artery haemorrhage. risk of dysrrhythmia on insertion and/or high grade block if already in LBBB. data error PAC in West Zone I. we don’t know what an adequate Q is. absence of data supporting an algorithm to maintain a certain cardiac output. EVIDENCE - RCT’s have not shown a positive effect of PAC. - early data showed increase harm. - PAC Man trial showed not change in in-hospital mortality. - better to use in really sick patients. - very invasive procedure with highly morbid complications (bleeding on insertion, PA rupture, arrhythmia, PE). - does change management in sick patients in the early resuscitation phase Management of a Pulmonary Haemorrhage Post-wedging of a PAC 25/11/10 - can be a life threatening situation Goals: (1) prevent further pulmonary haemorrhage (2) stop bleeding (3) resuscitate Call for help – anaesthetist, cardiothoracic surgeon, interventional radiology Resuscitate A – may have to be emergently intubated if not already B – FiO2 1.0, controlled ventilation, if able to recognize which lung is haemorrhaging may be able to perform lung isolation (insert single lumen tube into unaffected side or exchange for a double lumen tube), apply PEEP C – large bore IV cannulae, fluids, blood products, inotropes Treatment - stop anti-platelet and anti-coagulants - protamine for heparin - platelets for anti-platelet agents - blood products as indicated by FBC, coags and clinical state - withdraw pulmonary catheter 2-3 cm and refloat PAC with balloon inflated to occlude pulmonary artery (to try and tamponade bleeding) Jeremy Fernando (2011) - angiogram or bronchoscopy to isolate pulmonary vessel involved - if bleeding doesn’t settle will require a lobectomy MY APPROACH TO PAC USE - find them useful in undifferentiated, multi-factorial shock states (for Q and ScVO2) useful in right heart pathology and pulmonary hypertension perform careful patient selection (including a contraindication assessment) don’t wedge monitor for complications (predominantly on insertion) remove after 72 hours Jeremy Fernando (2011)