IRB Homework Assignment
advertisement

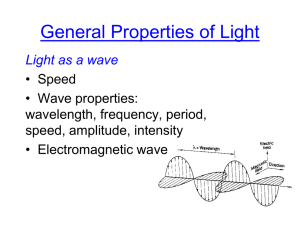
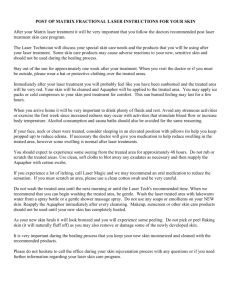
APPLICATION FOR IRB REVIEW University of Austin, Institutional Review Board Title: Optical clearing of the skin in conjunction with laser treatments Lead Researcher Name: Tim Wolf, MD, PhD SECTION 1: BACKGROUND AND PURPOSE OF THE RESEARCH Certain dermatologic entities that are treated with lasers require multiple treatments and variable results are achieved. Pulsed dye lasers (PDL) in combination with cryogen spray cooling (CSC) are the standard of treatment for Port Wine Stains (PWS) and other benign vascular lesions. Lasers typically used for treatment of vascular lesions have a wavelength of 585-595 nm, yellow light that is preferentially absorbed by the blood in the capillaries of the dermal vasculature. Preferential absorption by blood results in heating and coagulation of the capillaries, eventually reducing redness due to the superficial capillaries and improving the visual appearance of the patient’s Port Wine Stain. Multiple factors contribute to variability in laser treatment efficacy and the need for multiple treatments. However, one significant factor is the inability of current laser devices to deliver adequate light doses to the target because of energy loss resulting from tissue scattering. Skin is a highly turbid and light scattering medium because of refractive index differences between water and various inter/intracellular components. The skin surface scatters almost 5% of incident light (i.e., surface glare). In the dermis an additional 40% of light is scattered. Regardless of the indication and the laser device used for treatment, the clinical outcome for each treatment is any where from 30-40%. Although multiple factors contribute to the efficacy, the major one is the loss of light energy due to tissue scattering. The present clinical study will investigate a method of reducing light scattering and attenuation in in vivo human skin using a topically applied mixture of two investigational chemical polymers, which will aid index matching of cellular components. The chemicals have been tested in our lab on freshly excised human facial skin and been shown to affect the reflectance and transmission properties of the skin when applied on the intact epidermis as well as on the dermis. These chemicals are not FDA-approved. Chemical #1 is a polymer which has been under development across town for 10 years at Austin Institute of Technology and has demonstrated no harmful side effects when applied to primate skin for extended periods of time. Chemical #2 was developed in the laboratory of Dr. Wolf and has demonstrated no harmful visible side effects when applied to primate skin for less than 6 hours. When Chemical #2 was applied to the skin of primates for more than 6 hours, primate subjects experienced mild discomfort and loss of appetite. HYPOTHESIS: Our hypothesis is that topical application of a mixture of optically clearing investigational chemicals will reduce skin light scattering, increasing the amount of light reaching the target for diagnostic as well as therapeutic purposes. As such, we expect that application of the optical clearing agents for treatment of benign vascular lesions such as Port Wine Stain (PWS) will result in 1) decreased reflectance of the predominant color from the surface of skin (decreased red light scattering in case of benign vascular lesions, etc) as compared to the control group; 2) greater imaging depth as compared to the control group and 3) greater improvement in the treatment outcome, (decrease in redness following laser treatment of vascular lesions as compared to the laser alone group. Based on preliminary studies, we also hypothesize that 24 hour application of the optical clearing chemical agents versus 2 hour application will result in a significant difference in the aforementioned end points for treatment outcomes. Please note that all of the laser procedures to treat PWS are regularly performed in our laser clinic at the University of Austin Medical Center. SPECIFIC AIMS: Our specific aims are to evaluate the optical clearing effects of investigational chemicals. Effective optical clearing would result in 1) decreased light reflectance; 2) improved imaging depth and 3) improved laser treatment effect. This study also INSTITUTIONAL REVIEW BOARD REVISED 6/01 aims to determine if a longer application time (24 hrs vs. 2 hrs) will result in improved optical clearing effects and the relative efficacy of the two chemicals being considered. Subjects seeking laser therapy will receive the laser treatment only if they agree to participate in this study. Involvement in the study will require formal documentation of the treatment response in form of photographs, clinical assessment, imaging and light reflectance measurements (non-invasive measurements of light). INSTITUTIONAL REVIEW BOARD REVISED 6/01 SECTION 2: BACKGROUND AND EXPERTISE OF STUDY TEAM Tim Wolf, MD, PhD is a board-certified dermatologist and has completed a two and half year fellowship in laser surgery and medicine. He is now serving as an assistant professor and resident dermatologist at the University of Austin Medical Center. Dr Wolf is the lead researcher conducting this study and will also be responsible for data collection, analysis, and interpretation upon study conclusion. Dr. Wolf will also be performing laser therapy treatments. Brandon Simpson, MS is a senior graduate research assistant in the laboratory of Dr. Wolf. His current research projects include clinical evaluation of optical imaging for noninvasive characterization of vascular lesions and development of optical clearing for reduction of optical scattering in biological tissue. He will participate in performing delivery of the investigational polymer clearing agent as well as measurements on patients. SECTION 3: RESEARCH METHODOLOGY/STUDY PROCEDURES This is a one year study. Initially, twenty-five subjects will be recruited from patients seeking laser treatments for Port Wine Stain at the University of Austin Medical Center. Subjects will be enrolled and treated one time with the laser. Should they desire to continue treatment after 8 weeks of follow-up and if chemical application improved treatment results without adverse effects, subjects may receive additional treatments until completion of the study. Patients will be eligible for the study if their proposed treatment site measures 3 cm2 or more and is present on any body site. At each visit, documentation of the study site will be obtained by digital photography and OCT (optical coherence tomography) imaging. Reflectance measurements will be taken with a non-invasive probe that will be cleaned with an alcohol swab, applied gently to the study site and to the surrounding un-involved skin and measurements will be taken. This is similar to shining a flashlight on the skin and measuring the light. OCT imaging of the study site may also be performed. The light source for imaging is a regular white light source that scans a beam of light across the area under imaging and collects the back-scattered light. The light is then processed by the computer to generate an image of the skin resembling that of a vertical section of skin histology but with lower resolution. The device itself is not in contact with the subject's skin, rather at a particular distance away from the skin. OCT is a class I, FDA-approved device, is harmless and no risk of eye injury is involved. Hence no safety goggles will be worn during the imaging session. Visit #1. Pre-treatment Screening visit: Pictures of the study site and the individual test sections will be taken under special lighting conditions. The study site will be traced on a transparent template and divided into 4 different treatment areas (Areas 1-4): Area #1 #2 #3 #4 Treatment modality Laser Treatment alone Investigational chemical #1 + Laser Treatment Investigational chemical #2 + Laser Treatment Control, no treatment Subjects will be asked if they wish to receive treatment of the control site. In which case, treatment will be provided at the completion of the study at the expense of the subject. INSTITUTIONAL REVIEW BOARD REVISED 6/01 Subjects will then be randomly divided into 2 groups, group A and group B. A thick layer of chemical will then be applied on Areas 2 and 3 and covered with dermatological tape. The chemical agent will be applied for 2 hours on the study site of the subjects in group A and for 24 hours in group B. Subjects in group A will be treated the same day after 2 hours of application whereas subjects in group B will be sent home with instructions and will be requested to return the next day after 24 hours. If the subjects experience irritation or itching they cannot remove the tape but can contact the principal investigator by pager or cell phone at any time. A contact number will be included in the consent form. Laser Treatment Visit. The tape will be removed and the area will be cleansed with alcohol. Subjects will be asked whether they experienced any discomfort, itching, or burning. The test areas will also be evaluated clinically looking for any redness, scaling, swelling, blistering, scabbing, skin discoloration or scarring. Dr. Wolf and a nurse will grade the degree of each of these characteristics. If there is a discrepancy of more than 1 severity level for any of the graded characteristics, Dr. Wolf will provide an additional assessment. All the areas will be photographed, OCT imaging will be performed and reflectance measurements will be taken as described for pre-treatment visit # 1. The three test areas designated for laser treatment will be irradiated using standard laser treatment parameters utilized routinely in the clinic. Areas 1, 2 and 3 will be treated with exact same laser power. These are standard treatment parameters used in our clinic. Subjects and all personnel present will wear protective eye glasses to shield their eyes during the laser treatment. No post-op medications will be provided. Follow-up visit # 1 Patients will have 3 follow-up visits which will last approximately 30 minutes per visit. Subjects will be asked to return for a follow-up visit 24 hours after their treatment. Pictures will be taken with a digital camera. Reflectance measurements will be taken with a non-invasive probe and live skin imaging will be done with OCT of the areas. Subjects will be closely evaluated for the degree of redness, scaling, swelling, oozing, blistering, scabbing, skin discoloration or scarring. If any adverse effects are noted they will be treated until resolution at the expense of the patient. Follow-up visit #2 Subjects will be asked to return for a follow-up visit one week after their treatment. Pictures will be taken with a digital camera. The reflectance measurements will be taken with a non-invasive probe. OCT imaging will be performed. Once again the treated sites will be evaluated for the degree of redness, scaling, swelling, oozing, blistering, scabbing, skin discoloration or scarring. Follow-up visit #3. Subjects will be asked to return for the 3rd follow-up visit 8 weeks after the laser treatment. This will be the last research related visit of their participation in the study. If they choose to have further treatments to any portion of their skin because of improved response and no adverse effects, it would occur off-study at the expense of the patient. The subjects will be photographed and reflectance measurements taken as per previous visits. OCT imaging will be performed. Once again the treated sites will be evaluated for the degree of redness, scaling, swelling, oozing, blistering, scabbing, skin discoloration or scarring. DATA ANALYSIS: The data obtained will be analyzed qualitatively and quantitatively. Qualitative analysis will include the subjective evaluation of the treatment site at each visit grading degree of redness, scaling, swelling, oozing, blistering, scabbing, skin discoloration or scarring. Common statistical analysis will be performed on the qualitative results. Quantitative analysis of PWS lesions will include comparison of pre-treatment and final visit scores of 1) redness index obtained from the digital polarized photography on a scale of 0-100% with 0 being completely blanched or white area and 100% being maximum redness 2) red reflectance measurements 3) OCT imaging depth. Pre- and 8 week post-treatment scores for each of the 3 test sites will be compared by student's t-test. INSTITUTIONAL REVIEW BOARD REVISED 6/01 SECTION 4: SUBJECTS (PERSONS/CHARTS/RECORDS/SPECIMENS) This is a pilot study. Twenty five subjects will be enrolled in this pilot study as a preliminary evaluation of this technique. Subjects with Port Wine Stain diagnosis and seeking laser treatment for port wine stain will be candidates for enrollment. Those who satisfy screening procedures and inclusion/exclusion criteria will be enrolled in the study. Patient enrollment will include both sexes. Inclusion Criteria -Port Wine Stain diagnosis in an area measuring 3 cm2 or more on any body site -Apparent good health as documented by medical history and physical examination -Ability to understand and carry out subject instructions Exclusion Criteria - Age < 18: minors will be excluded from the initial study because the study procedures will prolong the laser treatment. Laser treatment is often more difficult for children because of increased anxiety. -History of cutaneous photosensitivity -Any therapy to the proposed treatment sites within the previous two months -Current participation in any other investigational drug or device evaluation -Inability to understand and carry out subject instructions SECTION 5: RECRUITMENT/INFORMED CONSENT Informed Consent will be obtained from all subjects. The lead researcher or co-researchers will explain the full details of the protocol, experimental procedures, possible side effects, risks and complications of the treatment to each participant before informed consent is sought and documented on the standard University of Austin consent form. The subject will then be given the opportunity to sign the informed consent form in the presence of the lead researcher. Patient will be informed that they may withdraw their consent at any time during the course of the study, but will have to reimburse the University for the cost of any treatments performed. The patient will be given a copy of the informed consent to keep, and a copy will be placed as a permanent record in the patient’s medical chart. SECTION 6: ANTICIPATED RISKS/RISK MANAGEMENT The chemicals chosen for the study are not FDA-approved drugs. Names of the chemicals are not given due to the proprietary nature of the chemicals- they will be referred to as Chemical #1 and Chemical #2. Chemical #1 is used in several investigational studies into topically applied medications for the treatment of acne or fungal infections. Chemical #2 is a drug developed in the lab of Dr. Wolf in collaboration with a pharmaceutical startup company. Possible side effects associated with topical application of these chemicals include: -redness -scaling -oozing -blistering -skin discoloration -scarring All lasers to be used in this study are FDA-approved: Potential side effects associated with laser treatment are: INSTITUTIONAL REVIEW BOARD REVISED 6/01 -scarring -pigmentary change - scabbing -infection -pain -edema -frostbite -local skin allergic reaction to cryogen The investigator in this clinical trial have extensive experience with the use of laser systems in dermatology. This is the most critical element in managing patient risk. Subjects will be followed closely during the course of the trial and will have access to the investigators at all times, via telephone or pager numbers. There may also be risks which are currently unforeseeable. Adverse Effects Reporting: Safety will be evaluated at each visit by asking the patient about any adverse effects and by evaluating the treatment area. Subjects will be informed to report any suspected study-related illness or injury to the study investigator immediately. SECTION 7: POTENTIAL BENEFITS The benefits for this study are unknown. SECTION 8: ALTERNATIVES TO PARTICIPATION Subjects seeking laser treatment may initially decide not to participate in the study. In such cases, standard treatment with a laser will be withheld until the patient agrees to application of the chemical agent prior to receiving the laser treatment. SECTION 9: ADVERSE EVENT REPORTING/MANAGEMENT Safety will be evaluated at each visit by asking the patient about any adverse effects and by evaluating the treatment area. Adverse events will be reported in writing to the University of Austin IRB within 10 working days of the onset of the event, followed by any appropriate follow-up reports on a timely basis. All serious adverse events (i.e. hospitalization or death) will be reported to the IRB office within 48 hours of the onset of the event, with a completed Adverse Event Report Form to follow within 10 working days. Subjects who are injured or become ill as a result of their participation in this study will be provided reasonable and necessary medical care to treat the illness or injury at minimal cost to them or to their insurers/third party payers. The subjects will be informed to report any suspected study-related illness or injury to the study investigator immediately. SECTION 10: COSTS INSTITUTIONAL REVIEW BOARD REVISED 6/01 Subjects will be required to pay for the cost(s) of their laser treatment. Subjects will only be receiving the laser treatment if they chose to participate in the study. The costs of the chemicals used for optical clearing of skin will not be charged to the patient or their health insurance. SECTION 11: COMPENSATION Compensation of $100 will be provided to the patients if they participate in the study for both chemical #1 and chemical #2. No compensation will be provided for patients only wishing to enter the study for chemical #1. SECTION 12: CONFIDENTIALITY OF RESEARCH DATA The subject's medical information will be entered in the Dermatologic Research Database (DRD) which is available to clinicians and researchers over the World Wide Web. Data obtained from the patient participation will be collected in a file containing the subjects name, age, race & ethnicity, social security number, and photographs of the patients face from the front and side. A code label for each patient will be kept in a log book and all records will be stored at the University of Austin Medical Center. The records and results of these studies will be identified as pertaining to a certain patient unless he/she specifically asks for confidentiality. Photographs will be maintained digitally in a computer. Photographs will be used for pre- and post treatment comparison. Photographs will also be used for presentation at medical conferences or publication in medical journals unless the patient specifically requests anonymity. Subjects will not be informed that any information derived from this research project which personally identifies them may be released or disclosed without their separate consent. The research team, authorized University of Austin personnel, and other regulatory entities may have access to the study records to protect subject safety and welfare. INSTITUTIONAL REVIEW BOARD REVISED 6/01