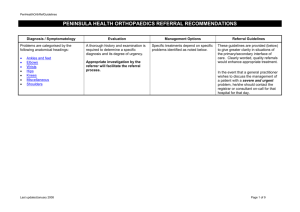
Referral Guidelines
advertisement

REFREC016 ORTHOPAEDICS REFERRAL RECOMMENDATIONS Diagnosis / Symptomatology Problems are categorised by the following anatomical headings: Ankles and feet Back Elbows Hands and wrists Hips Knees Miscellaneous Neck Shoulders Last updated February 2006 Evaluation A thorough history and examination is required to determine a specific diagnosis and its degree of urgency. Appropriate investigation by the referrer will facilitate the referral process. Management Options Referral Guidelines Specific treatments depend on specific problems identified as noted below. These guidelines are provided (below) to give greater clarity in situations of the primary/secondary interface of care. Clearly telephone/fax communication/e-mail would enhance appropriate treatment. In the event that a general practitioner wishes to discuss the management of a patient with a severe and urgent problem, he/she should contact the registrar or consultant on-call for that hospital for that day. Page 1 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Ankles and feet Arthritis Analgesics/anti inflammatories. Physiotherapy. Activity modification. Walking aids. Consider steroid injection. Refer if functional impairment despite conservative treatment after six months. Routine Category 4. Standard history and examination. Modification footwear. X-rays standing. Orthoses. Weight-bearing AP. Consider steroid injections for intermetatarsal bursal/neuroma. Refer for routine assessment Category 4 if severity of symptoms warrants after three months conservative treatment. Modification footwear. Orthoses. Physiotherapy. Consider steroid injection. Refer for routine assessment Category 4 if severity of symptoms warrants after three months’ conservative treatment. Standard history and examination. Physiotherapy. AVOID steroid injections. Heel cups/raise. Refer for routine assessment Category 4 in three months if conservative treatment fails or if patient has tender nodule. Standard history and examination. Physiotherapy. X-rays. X-rays allow exclusion of some diagnoses. NB: Plantar spurs on an x-ray does not infer plantar fascitis. Steroid injections for plantar fascitis. Heel cups/raise. Standard history and examination. Pain and deformity in forefoot (including bunions) Pain and instability in hind foot. Standard history and examination. Achilles tendon pathology. Heel Pain. X-rays. X-rays. X-rays. Refer as routine Category 4 after failure to respond to three months of conservative treatment. Ankles and feet (paediatric deformities) Club Foot Features to be looked for are fixed equinus and varus. Calcaneo Valgus Foot Almost always correctable to neutral, but check the hips for stability. Flat Feet Under the age of three years, flat feet Last updated February 2006 Refer immediately Category 1. Reassurance. If not flexible or not looking normal by three weeks, should be referred Category 2. Page 2 of 10 REFREC016 are normal. Ask the child to stand on tip toes. If the arch corrects, the foot is normal. In Toeing Standard history and examination. Diagnosis / Symptomatology Reassurance. Evaluation Management Options Only for a second opinion beyond walking age – Category 4. Referral Guidelines Back Mechanical low back pain without leg pain. Key points: Activity modification. Analgesics and NSAIDs. Duration of symptoms. Functional impairment. Time off work. Treatment to date. Previous spinal surgery. General medical condition and medication. Persistent severe symptoms refer as category 4 (See ACC Guidelines Booklet). Investigations: X-rays. FBC ESR Biochemistry. (Consider calcium and phosphate, electrophoresis, immunoglobulins, PSA, Rheumatoid serology in specific cases.) Mechanical low back pain with leg pain but without neurological deficit Key points: Note key points above Weight loss Loss of appetite Lethargy Fevers and sweats Last updated February 2006 If these symptoms present, refer as category 2 If these symptoms absent, refer as category 4 Page 3 of 10 REFREC016 Back pain and sciatica with neurological deficit. Spinal stenosis with limitation of walking distance. Back pain secondary to neoplastic disease or infection. Previous malignant disease Urinary difficulties As above. Diagnosis / Symptomatology Refer as Category 2. Evaluation Management Options Referral Guidelines Elbows Tendonitis. Standard history and examination. Consider Cortisone injection. Anti inflammatories. Bands. Refer as routine Category 4 if fails to respond to treatment after four weeks or recurrence. Locking. Standard history and examination. None. Routine Category 4 referral with x-ray, but consider occupation and functional disability. Painful/stiffness in elbow. Standard history and examination. Anti inflammatories. Consider FBC & ESR. Physiotherapy. Refer routinely Category 4 if not responding to treatment after three months. Last updated February 2006 Page 4 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Hands and wrists Contractures. Dupuytrens. Refer progressive contractures (especially PIP contractures) with functional impairment as routine. Referral Category 4. Standard history and examination. Key points: Duration and speed of progression. Functional impairment. Family history of Dupuytrens. Previous surgery. General medical conditions (especially diabetes, epilepsy, liver disease). Medications (especially for epilepsy). Stenosing tenovaginitis (eg Trigger fingers, de Quervains). Standard history and examination. Rheumatoid conditions (cf Rheumatology Recommendations). Standard history and examination. Basal Thumb Arthritis. Standard history and examination xray. Consider injection with steroids. Refer as routine referral Category 4 if functional impairment or if unresponsive to treatment after one injection. Referral to Orthopaedic Surgeon is via Rheumatologist/General Physician. Anti inflammatories. Activity modification. Consider steroid injection. Refer after six months as routine Category 4 if fails to respond. Ganglia. Standard history and examination. Consider aspiration (18g needle) and injection of steroid. Refer as routine Category 4 for symptomatic ganglia. Cosmesis alone usually is not a reason for referral. Painful/Stiff Wrists. Standard history and examination. Anti inflammatories. X-rays to include scaphoid views. Trial of wrist splint. Refer as routine Category 4 after six months. Physiotherapy. Congenital upper limb abnormalities (cf Plastic Surgery Referral Recommendation). Last updated February 2006 Refer to local service as available. Page 5 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Hips Hip Arthritis Osteoarthritis. Inflammatory Arthritis. Post Traumatic Arthritis. Avascular Necrosis. Standard history and examination. Anti inflammatories. Key points: Analgesics. Physiotherapy. Walking distance. Rest pain and disturbance of sleep. Locking and/or instability Ability to put on shoes. Use of walking aids. Treatment including NSAIDs and analgesics. Previous joint surgery. General medical conditions and medication. History of recurrent infections and prostatism. Refer if significant pain, problems relating to mobility, sleep disturbance, and unresponsive to therapy over several weeks – Category 3. Activity modification including the use of a walking stick. Home modification and use of ADC. Investigations: X-ray (AP pelvis, AP affected hip showing proximal 2/3 femur, and lateral affected hip). (Note: NHC Criteria for major joint replacement.) Paediatric Hip Conditions (Perthes, SUFE, Synovitis). History, examination and x-ray. Beware of pain in the knee as a symptom of hip disease. Bed rest and simple analgesics. Acute referral for admission if systemically unwell, febrile, or on suspicion of SUFE – Category 1. Otherwise re-assess at 24 hours. Age ranges usually: Transient synovitis 18 months to 6 years. Perthes 4-10 years. SUFEs usually 8-14 years. If hip dysplastic, refer as Category 3. Last updated February 2006 Page 6 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Knees Anti inflammatories/analgesics. Osteoarthritis. Standard history and investigation. Key points: Physiotherapy. Inflammatory Arthritis. Walking distance. Post Traumatic Arthritis. Rest pain and sleep disturbance. Activity modification including the use of a walking stick. Avascular Neurosis. Use of walking aids. Home ADC. Treatment including NSAIDs and analgesics. Previous joint surgery. General medical condition and medication. Knee Arthritis: Refer if significant pain, problems relating to mobility, sleep disturbance and unresponsive to therapy over several weeks – Category 3. History of recurring infections and prostatism. Investigations: X-rays – four standard views plus standing AP total knees. (Note: NHC criteria for major joint replacement.) Last updated February 2006 Page 7 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Miscellaneous Consider one steroid injection for carpal tunnel. Splintage. Refer semi urgently – Category 3 – if muscle wasting, otherwise, after three months refer routinely – Category 4. Nerve Entrapment Syndromes. Standard history and examination. Bone and/or Joint Infection. Standard history and examination. Acute referral to Orthopaedics – Category 1. Bone and Soft Tissue Tumours. Standard history and examination. Refer urgently if tumour or suspicion of tumour – Category 2. Do not needle biopsy. Bursitis (Pre Patella, Trochanteric, Olecranon). Standard history and examination. Acute/inflammatory, consider aspirating for diagnosis. Will either be traumatic, gouty or infected. If acute, consider aspirating for relief of symptoms. Do not incise. If chronic, consider steroid injection. Refer if non responsive to treatment after three months, and symptomatic as routine assessment – Category 4. Apophysitis, eg Osgood Schlatters, Standard history and examination. Consider x-ray. Activity modification, reassurance. If second opinion or confirmation required only – Category 4. Standard history and examination. Reassurance. Refer for second opinion or severe deformity outside the normal age range – Category 4. Passive stretching by parent or physiotherapist. If failure to respond after one year of age, routine assessment – Category 4. JL Disease. Gait. Sterno Mastoid Tumour (congenital Muscular Torticollis). Symmetrical bow legs up to two years are usually physiological Knock knees from age 2 – 4 are also usually normal Angular deformities are usually pathological Standard history and examination. cf Paediatric Surgery Referral Recommendations. Last updated February 2006 Page 8 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Neck Mechanical neck pain without arm pain. Key points: Neck pain associated with referred pain to the upper arm without neurological deficit. Duration of symptoms. Work status. Treatment to date. General medical condition. Key points: Presence of neurological symptoms and signs including evidence of lower limb spasticity. Weight loss, appetite loss and lethargy. Fever and sweats. Previous malignant disease. Trial of soft collar. Activity modification. Analgesics and non steroidal antiinflammatories. If symptoms and signs persist more than 6 weeks – refer as Category 4. If any of these adverse features are present refer as category 2. If not present, refer as category 4. Investigations: X-ray. FBC & ESR. Biochemistry. (Consider calcium and phosphate, protein electrophoresis, immunoglobulins, PSA, Rheumatoid serology in specific cases.) Neck pain associated with radicular symptoms and neurological deficit. Cervical myelopathy. Neck pain secondary to malignant disease. Neck pain secondary to infection. Last updated February 2006 Routine history and examination noting the key points as above. Refer for an immediate opinion – Category 1. Page 9 of 10 REFREC016 Diagnosis / Symptomatology Evaluation Management Options Referral Guidelines Shoulders Rotator Cuff Tendonitis/Tears. Pain/stiffness in shoulder. AC joint problems. Recurrent dislocated shoulder/shoulder instability. Last updated February 2006 Standard history and examination particularly neurological examination. X-rays (standard views). Consider FBC & ESR. Ultrasound examination. Standard history and examination particularly neurological examination. X-rays (standard views). Consider FBC & ESR. Standard history and examination particularly neurological examination. X-rays (standard views). Consider FBC & ESR. Standard history and examination particularly neurological examination. In older patients difficulty elevating the arm following a dislocation. Consider ultrasound examination. X-rays (standard views). Consider FBC & ESR. Anti inflammatories. Physiotherapy. Consider Cortisone injections. Anti inflammatories. Physiotherapy. Consider Cortisone injections. Anti inflammatories. Physiotherapy. Cortisone injections. Shoulder rehabilitation programme (Physiotherapy) Refer if patient fails to respond to treatment after three months unless evidence of weakness suggestive of an acute rotator cuff tear which should be referred as Category 3. Refer after three months – Category 3. Refer after six months if persisting symptoms as Category 4. Refer as routine referral (Category 4) if recurrent functional instability and/or pain and has not responded to the rehab programme after three months. Consider referral after recurrent shoulder dislocation – Category 4. Rotator cuff tear following shoulder dislocation – Category 2 Page 10 of 10