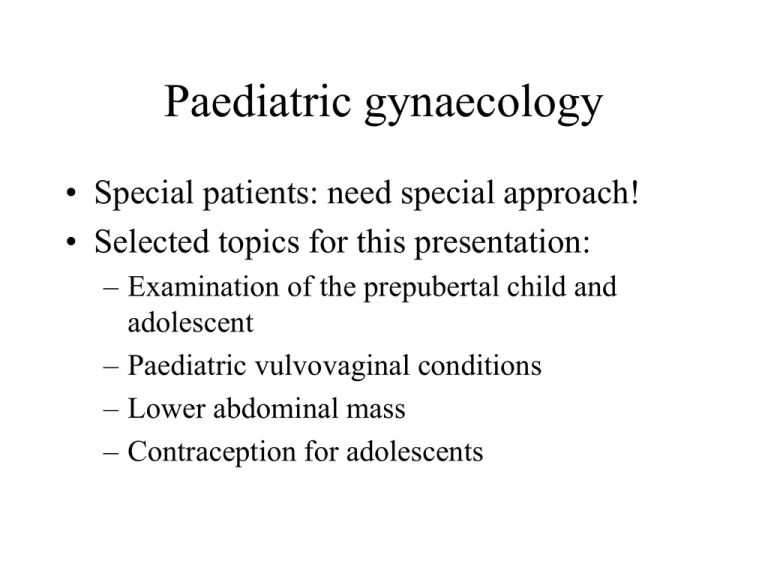
Paediatric gynaecology
• Special patients: need special approach!
• Selected topics for this presentation:
– Examination of the prepubertal child and
adolescent
– Paediatric vulvovaginal conditions
– Lower abdominal mass
– Contraception for adolescents
Examination of the prepubertal
child
2
• Principles: Trust will lead to improved cooperation
– Private, peaceful, unhurried: respect wishes of the child
• History: from parents/care providers and child herself
–
–
–
–
–
Key issues: --Growth and development
Childhood and other illnesses
Family structure
Friends, play patterns, “best friend”
Molestation
Examination
3
• Do not press child down!
• Remember anatomical differences between child
and adult
• Standard systemic examination
• Gynaecologic examination: frog-legged position (on
bed or parent’s lap) better than knee-chest
– Thin catheter: MCS specimens
– Single finger PR when required
– EUA if trauma or office examination does not work out
Examination of adolescent
4
• Principles: teach patient concept of doctor-patient
relationship and privacy
– See patient on her own, let her speak
• History: standard systemic history
– Key issues: pubertal development, menstruation,
tampon use, sexual activity (voluntary or not)
• Examination: standard technique
– Occasional use of “virgo” speculum
– PR or 1 finger PV
Vulvovaginal conditions
5
• Common; can usually sort out with simple
tests
• 1 Bleeding
– Vaginitis: Shigella, Strept, E coli, threadworm,
candida may all cause blood stained discharge
• Usually preceding watery diarrhoea
• Rx; Antibiotics + topical oestrogens for 1
week
Bleeding (continued)
6
– Foreign body: chronic discharge with bleeding.
Perform PR and MCS of discharge, and for
vaginoscopy if in doubt. Remove objects, requently
under GA. Assist healing with topical oestrogen
– Trauma
– Sarcoma botryoides: rare; mass with bleeding: refer
– Urethral mucosal prolapse: common, looks like
tumour. Oedema, necrosis, inflammation. Caused by
hypo-oestrogenism. Rx: oestrogen cream 2 weeks, if
necrotic excise dead tissue
Vulvovaginal conditions
7
• 2 Abnormal appearance
– Labial adhesions: hipo-oestrogenism and mild
vulvitis: 80% asymptomatic, noted by mother. May
separate at examination, assist with oestrogen cream.
– Imperforate hymen and hymen variants/cysts
– Lichen sclerosus
– Condylomata acuminata
Vulvovaginal conditions
(continued)
8
• 3 Discharge
–
–
–
–
Threadworm
Chemical irritants
Candidiasis
Pyogenic infection: gram + and – organisms,
chlamydia and anaerobes: specimen for culture
and then specific Rx.
Lower abdominal mass in a child
9
• Clinical: asymptomatic swelling / bladder
symptoms / pain / hormonal changes /
complications
• Tests: ultrasound, beta-hCG
• Principles of treatment: most are benign:
longitudinal incision, inspect, washing, USO.
Preserve fertility if possible. If malignant: refer for
chemotherapy
Contraception for adolescents
10
• Problems: adolescent sexual behaviour irregular,
unplanned, fears and anxieties, poor compliance
• Law: what can doctor do
• Principles: by the time help is required, patient is
already sexually active
– Information on sex, STD, HIV, pregnancy
– Motivate for proper pill use and follow-up
– Motivate for abstinence: do not moralise