Christy Ermak (with Akane Seki)
advertisement
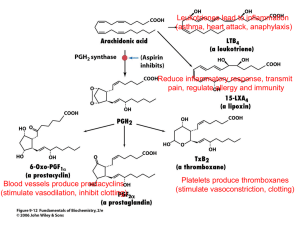
Is Celebrex as Detrimental to the GI Tract as Non-selective NSAIDs and Is There An Increased Risk of Cardiovascular Events With The Use of Celebrex? An Argument Paper for Pfizer Pharmaceutical Representatives Akane Seki and Christine Ermak Spring 2005 Issue The recent controversy surrounding Vioxx has triggered many questions about the safety of other COX-2 inhibitors such as Celebrex. Many studies have shown the statistical significance in which Vioxx demonstrated the increased risk of acute myocardial infarction (See Table 1). The incidence of stroke was greater with Vioxx than with other anti-inflammatory prescription medications as well. Celebrex is in the same COX-2 inhibitor class as Vioxx and is still being prescribed for similar purposes. Vioxx was thought to be the most effective COX-2 inhibitor, but because of its discontinuation many physicians have instead substituted Celebrex for Vioxx regimes. It is important to investigate the safety of Celebrex because it is a widely prescribed medication not only for arthritis patients, but for patients with severe migraines, dysmennorhea and to treat post-surgical procedures. Although Celebrex and Vioxx are in the same COX-2 class they have different functional groups within their chemical structures (see Figure 2). They also differ in their potency, specificity of COX-2 inhibition, pharmacokinetics and metabolism. Thus, the question at hand is how much do 1 these differences actually affect the physiological mechanisms in which risks of heart and gastrointestinal complications are increased? An understanding that the effectiveness of Celebrex is not what has caused so much controversy must be recognized. There were many studies reviewed by the FDA concerning Celebrex before it ever was put on the shelf, which showed it was just as effective as non-selective NSAIDs at decreasing inflammation (Crawford et al.2002 and Nachimuthu et al. 2001). The argument here is concerning the safety of the drug in terms of cardiovascular and gastrointestinal side effects. Despite studies that have inferred risks of Celebrex use, after sifting through a large portion of the current research that has been published about Celebrex, it is safe to say that this drug is gentler on the GI tract as well as safe for cardiovascular health than non-selective NSAIDs that are available on the market today. Table 1. Evidence that the issue is unresolved Celebrex Safe in terms of Cardiovascular risks Celebrex unsafe in terms of Cardiovascular safety Celebrex safe on the GI tract Chenevard et al. (2003) Rabausch et al. (2005) Simon et al. (1999) Celebrex not any safer on the GI tract than nonselective NSAIDs Crawford et al. (2002) Levesque et al. (2005) Solomon et al. (2005) Silverstein et al. (2000) Nachimuthu et al. (2001) Mamdani et al. (2002) Brief Overview of COX-2 Inhibitors COX-2 inhibitors are manufactured with the specific purpose of gastrointestinal safety in mind. The COX-2 inhibiting drugs, such as Vioxx and Celebrex, have proved to be 2 involved in directly alleviating inflammation with less gastrointestinal complications than non-selective NSAIDs. Prostaglandin G/H synthase, the enzyme that catalyzes prostaglandins and thromboxanes which specify pain and platelet aggregation, is inhibited by both non-selective NSAIDs and COX-2 inhibitors. Inhibiting the COX-2 enzyme may be of therapeutic advantage, since this isoenzyme is almost certainly involved in prostaglandin production at the site of inflammation but not at other sites such as the gastrointestinal tract and kidney. Non-selective NSAIDs target the COX-1 enzyme activity in gastrointestinal mucosa and platelets as well as COX-2 enzyme activity. However, COX-2 inhibitors such as Celebrex do not interfere with the COX-1 receptor. COX-1 enzymes are responsible for producing the protective mucous lining in the GI tract as well as decreasing levels of HCl secretion in the stomach and stimulating intestinal motility. It also is the constitutive isoform found in the blood vessels, stomach and kidney. COX-2 enzymes on the other hand are induced in settings of inflammation by cytokines and inflammatory mediators. Consequently, this inhibition of both COX isoenzymes and prostaglandins has been related to gastrointestinal tract toxicity and the long-term use of non-selective NSAIDs is therefore limited by gastrointestinal effects such as abdominal pain, constipation, dyspepsia, nausea, vomiting and constipation (See Table 2). It is worth noting to hear that it is not the actual medication itself that is responsible for eating a hole through the mucosal lining of the stomach. Rather the COX-1 receptors are compromised with the use of the non-selective NSAID’s, which significantly decreases resilience of the mucosal lining of the stomach. It is then the individual’s own stomach acid which irritates the stomach wall and can cause an ulcer. 3 Table 2. Adverse events cccurring in ≥2% of Celebrex patients (From Celebrex Premarketing Controlled Arthritis Trials) Abdominal Pain Diarrhea Dyspepsia Flatulence Nausea Celebrex (100-200 mg BID or 200 mg QD) (n=4146) Placebo (n=1864) Naproxen 500 mg BID (n=1366) Diclofenac 75 mg BID (n=387) Ibuprofen 800 mg TID (n=345) 4.1% 5.6% 8.8% 2.2% 3.5% 2.8% 3.8% 6.2% 1.0% 4.2% 7.7% 5.3% 12.2% 3.6% 6.0% 9.0% 9.3% 10.9% 4.1% 3.4% 9.0% 5.8% 12.8% 3.5% 6.7% Because prostaglandins are the most abundant chemical messenger in the body, affecting activity in each body system, the pharmaceutical industry has long targeted research involving selective control of them (See Figure 1). Figure 1. Synthetic pathway and sites of actions of prostaglandins. Studies Promoting the Cardiovascular Safety of Celebrex Despite Celebrex’s being in the same COX-2 class as Vioxx, there are many studies promoting the cardiovascular advantages of Celebrex (Silverstein et al. 2000, 4 Chenevard et al. 2003, Levesque et al. 2005, Sower et al. 2005, Aw et al. 2005). Specifically, the study performed by Levesque et al. (2005) found that Vioxx increased cardiovascular events, but this was not the case with Celebrex. The results of these findings are able to be extrapolated to a larger population due to an extremely large subject size (n=113,927) for an at risk elderly population. In addition, Sower et al. (2005) and Aw et al. (2005) confirmed these findings when their results revealed that Vioxx does increase blood pressure, but Celebrex does not. The different chemical makeup of Celebrex and Vioxx may explain how these two drugs can perform the same anti-inflammatory actions with very different physiological outcomes such as increased cardiovascular risks. Celebrex and Vioxx differ in their pharmacokinetics as a result of differing functional structural characteristics which may provide an explanation for the safety of Celebrex. Both Celebrex and Vioxx have two benzane rings, but have different functional groups (See Figure2). Celebrex is 97% bound to plasma protein and in turn the remaining 3% is distributed throughout the body. On the other hand, Vioxx is 87% bound to plasma protein leaving 13% to be released in the body. Celebrex also has a shorter half-life of 11 hours versus a half-life of 17 hours for Vioxx, leaving the duration of action of Vioxx in the body an additional 6 hours longer than Celebrex. Because of the shorter half-life of Celebrex it is easier to control plasma levels because it is cleared from the blood more rapidly than Vioxx and needs to be given in frequent doses in order to develop and maintain a sufficient concentration in the blood to be therapeutically effective. In turn the possible side affects Figure 2. Chemical Composition of Celebrex (left) and Vioxx (right) 5 due to Celebrex are easier to control because of its shorter half life. Currently, Celebrex has been used in studies to find if there are any other conditions in which Celebrex may not only be used as an inflammatory preventative but as helping cardiovascular function. While Vioxx and Celebrex still act in a similar manner in terms of inflammation, they do not necessarily act the same way when it comes to platelet coagulation. A study that was performed recently found that Celebrex actually improved endothelial-dependent vasodilation in high risk patients who had advanced coronary artery disease (Chenevard et al. 2003). Celebrex can help lower risk of heart complications by lowering oxidized LDL (ox-LDL), improving flow-mediated dilation, lowering high-sensitivity C-reactive protein (hs-CRP) that aggregate atherogenesis and lower oxidative stress and chronic inflammation in the arteries of the heart (See Figure 3). Figure 3. A. Flowmediated vasodilation was significantly increased after 14 days of treatment with celecoxib (P=0.026 vs placebo). B.Endotheliumindependent function as assessed by nitroglycerine-induced vasodilation remained unchanged (P=0.75 vs placebo). C. High-sensitivity CRP was lowered after 14 days of treatment with celecoxib (P=0.019). D. COX-2 inhibition with celecoxib decreased oxidized LDL plasma levels (P=0.028 vs. placebo) 6 In turn Celebrex, reduces the oxidative stress placed on the arteries as is evident by the decrease in the highly indicative oxidative stress markers CRP and oxidative LDL. Studies Opposing the Cardiovascular Safety of Celebrex Celebrex’s cardiovascular safety has been closely assessed and although most studies promote its cardiovascular safety, there are a few studies that have not agreed with the majority. There has been evidence in one study (Solomon et al., 2005) which found that Celebrex actually increases the risk of cardiovascular events in patients who were administered the drug. The idea behind their research was that Celebrex was responsible for promoting a prothrombotic (platelet coagulation) state and would therefore cause a higher incidence of heart attacks, strokes and/or heart failure. This is good research, but it needs to be known that any patient with a family history or even a personal history of such cardiovascular events would naturally be at a higher risk. In the study performed by Solomon et al. (2005), Celebrex was found to increase the risk for a cardiovascular event in comparison to a placebo group by 1.3% - 2.4% depending on the dose administered (200 mg BID or 400 mg BID) (See Table 3). End Point Placebo (n=679) Celebrex 200 mg BID (n=685) Celebrex 400 mg BID (n=671) Both Celebrex groups (n=1,356) Death from cardiovascular cause 1(0.1) 3(0.4) 6(0.9) 9(0.7) Nonfatal myocardial infarction 3(0.4) 9(1.3) 9(1.3) 18(1.3) Nonfatal stroke 3(0.4) 3(0.4) 5(0.7) 8(0.6) Nonfatal heart failure 2(0.3) 1(0.1) 4(0.6) 5(0.4) Table 3. Incidence of Individual Cardiovascular and Fatal Events for different doses of Celebrex. There is a dose-dependent increase in the risk of cardiovascular events. Number of Patients (percent) 7 It is more common for a doctor to treat a patient with a dose closer to 200 mg BID than it is to treat a patient with the higher dose. Those higher doses (400 mg BID) are often reserved for the patients afflicted with much more aggressive inflammation. In the case of those patients, the benefits would most likely out weigh the risks. For these select individuals, it comes down to one simple issue questioning a cost-benefit relationship of Celebrex. What quality of life do I want? On the other hand, there have been studies done that question the safety of COX-2 inhibitors as a whole class. Because class effects are placed on every drug in a class it is difficult to overlook negative outcomes for one specific member of this class. A few weeks after Vioxx was withdrawn from the market the National Cancer Institute announced the premature termination of a Celebrex study, Adenoma Prevention with Celecoxib (APC), because of significant excess of cardiovascular death, myocardial infarction, and stroke (See Figure 4). Figure 4. Event Rates of Cardiovascular Death, Myocardial Infarction, and Stroke in the Adenoma Prevention With Celecoxib (APC) Trial. The difference for events between the 400mg and 800 mg dose was not significant but was significant between the placebo and 400 mg dose. 8 Rabausch et al. (2005) also found that COX-2 inhibitors as a class lowered the levels of thrombodulin by inhibiting vascular formation of prostacyclin. However, this study was not preformed in vivo, but rather on tissue samples and cannot be considered strong enough evidence to pull Celebrex from the shelf. Just because other drugs in the same class pose adverse cardiovascular affects, it does not mean others in the same class necessarily will. Thus, the question of its safety must be resolved as soon as possible. Studies Promoting the Gastrointestinal Safety of Celebrex Several studies have reported a significantly lower incidence of ulcers in patients who were treated with Celebrex rather than non-selective NSAIDs (Mamdani et al.(2002), Emery (1999)., Ekenel et al (2003), Simon et al. 1999. Silverstein et al., 2000). It has been found that even though Celebrex does not completely eliminate incidence of ulcers, when it is compared to popular non-selective NSAID treatment it is obvious that Celebrex greatly reduces the incidence of ulcers (See Figure 5). When compared to the Figure 5. Incidence of Gastroduodenal Ulcers Over 12 Weeks of Treatment. An ulcer was defined as any break in the mucosa at least 3 mm in diameter with unequivocal depth. For each patient there were 3 possible outcomes: known ulcer, known no ulcer, and unknown. Any endoscopic finding other than ulcer was categorized as unknown if the data were obtained before the 12-week visit. Naproxentreated patients had a significantly greater incidence of gastroduodenal ulcers than did patients treated with either celecoxib or placebo (P<.001). The incidences of gastroduodenal ulcers in the celecoxib treatment groups were similar to that in placebo-treated patients (P>.40. Celecoxib and naproxen were both administered twice daily for all dosages. 9 common rheumatoid arthritis treatment of Diclofenac, Celebrex takers revealed an 11% decrease in the incidence of ulcers (Emery et al. 2003). When compared to Naproxen Celebrex decreased the incidence of ulcers by 20% (Simon et al. 1999). The Celecoxib Long-term Arthritis Safety Study (CLASS), consisting of two oneyear double-blind studies, performed by Fred E. Silverstein et al (2000) revealed that Celebrex, at dosages greater than those indicated clinically, was associated with a lower incidence of symptomatic ulcers and ulcer complications combined, as well as other clinically important toxic effects, compared with non-selective NSAIDs at standard dosages (See Figure 6). This study included a large subject pool consisting of subjects of adults of all ages with any type of arthritis. Figure 6. Data are pulled from 12-week placebo controlled trials. Celebrex significantly lower than Naproxen. Ulcer incidence in patients with rheumatoid arthritis 30 Patients with ulcers (%) 25 20 15 % 10 5 0 Placebo 50-400 mg Celebrex BID 500 mg Naproxen BID Drug doses (mg) Studies Opposing the Gastrointestinal Safety of Celebrex When it comes down to the GI safety of Celebrex, it is virtually impossible to find any completed research-based studies that found conclusive results to show Celebrex is detrimental to the GI tract. This phenomenon is not surprising because Celebrex was 10 specifically designed to be gentler on the stomach and intestines than non-selective NSAIDs. There have been a few case studies in which patients have been documented as having developed severe ulcers which may be due in part to Celebrex use (Nachimuthu et al. 2001, Crawford et al. 2002). While case studies are an excellent way to observe an individual and provide research on a more personal level, the results from these studies are not able to be extrapolated to a larger population. A perfect example of this is the research report given by Nachimuthu et al (2001) that found Celebrex may actually be harmful to the GI tract. The patient that was being observed in this particular study was a 67 year old woman who was admitted to the hospital for severe upper abdominal pain. She had multiple medical problems such as hypertension, diabetes, congestive heart failure and gastrointestinal bleeding secondary to peptic ulcer disease. Due to all of these ailments, she was taking several prescription drugs everyday and Celebrex happened to be one of them. Therefore, due to the incredibly high daily ingestion of several different medications, it was no surprise when doctors found ulcers in this individual’s stomach. However, it is impossible to be certain that Celebrex was the cause of the ulcerations since several medications were taken on a regular basis and the patient had a history of bleeding ulcers before ever taking Celebrex. An almost similar case was also reported in a 67 year old man who was admitted to the hospital due to an adverse reaction to a vaccination he had received a week prior to his admittance to the hospital (Crawford et al., 2002). Similarly, this individual had a lengthy health history that included several medical problems and he was taking seven different medications everyday to control his ailments. Included in his mini-pharmacy were the drugs Celebrex and aspirin. It is known that regularly taking aspirin can cause ulcerations and GI bleeding so it is 11 impossible to definitively conclude that Celebrex was the sole contributor in this individual’s development of ulcers. It is worth noting that this older man was taking an extremely large dose of Celebrex (600 mg daily) and for an extended period of time (14 weeks) which is rarely prescribed to any patient. If however, Celebrex is in fact responsible for these ulcerations and has become so popular because of its so-called GI advantages and these advantages do not exist, patients should merely stick to taking traditional NSAIDs that do not pose additional problems. Strengths and Limitations of Research The biggest strength of the research supporting the safety of Celebrex was that we had at least 1,000 participants in all of the studies except for one. A study performed on fourteen males who had severe coronary artery disease (Chenevard et al. 2003) was the smallest group of individuals we included. Although this study “broke” our rules by having a very small subject size, it was decided that we would use the findings in our research because the techniques used were very invasive an it would not be practical to have an extremely large group of individual that were willing to participate in this type of research. It is also important to include this research because it showed that Celebrex can actually be cardiovascularly beneficial to some individuals. Our research was also very inclusive and strong because we did not single out one particular type of ailment. Because this is a drug that has many different uses, anyone who is taking Celebrex would potentially be at risk for developing ulcers and cardiovascular complications. If there were strong enough evidence to prove that there were serious adverse side effects to this medication it would be important to look at every type of individual who could be prescribed Celebrex. Included in our research were 12 studies that had participants who had rheumatoid as well as osteoarthritis, cancer patients, patients with coronary artery problems and individuals with a history of colorectal adenoma just to name a few. Yet another strength of the research which has been conducted was that we also chose to include an extremely large age range (18 - ≥ 66 years of age) which allowed us to account for any age dependent risk factors such as increased cardiovascular risks in the elderly population. Age also played a role in our decision making process. The youngest subject that was included was 18 years old and we went clear past 66 years old on the other end of the spectrum. This was important to us because the risks that may be associated with taking this drug would be evident on or after the fifth day since this is when the Celebrex obtains its highest concentration in the plasma. If we would have narrowed our search down to one specific age group the potential of missing a population that was at an increased risk of developing adverse side effects would have been ignored. By including all of the research groups that we did, we were able to get a much better idea of the true safety of Celebrex. In terms of limitations, there was only one big setback. Since the cardiovascular safety of Celebrex is a fairly new idea, there have not been a lot of long term studies published concerning this topic. However, Vioxx was voluntarily pulled off the market by its manufacturer Merck because on going research found that it was detrimental to cardiovascular health after 18 months of continued use. Thus, in order to pursue safer research it is understood that there should be stricter precautionary guidelines concerning duration of studies on Celebrex. When it comes to the safety on the GI tract there is no question that there is a decreased risk of developing ulcers while using Celebrex instead 13 of a non-selective NSAID. In order to mend this limitation more research is needed in this particular area of interest in order to further reinforce our findings. Additional benefits of COX-2 inhibitors With the recent attention from the media on the COX-2 inhibitor drug family, many new beneficial research conclusions are being overlooked. Not only is Celebrex great in terms of reducing inflammation, but it has also proved to be useful in treating other medical conditions such as cancer and traumatic brain injuries. Certain types of cancer in which the patient was prescribed Celebrex found that its physiological mechanisms actually aided patients’ bodies by not allowing the mutated cells (hematopoietic and epithelial cells) to multiply (Waskewich et al. 2002). One mechanism that researchers feel is responsible for these findings is that the COX-2 inhibitors are helping the CD8+ t cells (killing cells) get into the actual tumor easier and are then able to aid in the elimination of the growth. Another hot topic that has been introduced to the medical community is the benefits of using a COX-2 inhibitor in the treatment of traumatic brain injuries. In a rat model, when a COX-2 inhibitor was given within six hours of the brain injury, there was marked improvement in the outcome of the subject. Researchers believe that this is due in part to the reduction in the inflammation of the tissue surrounding the neurons of the brain and therefore oxygen was allowed to remain at high levels. If more studies can be performed in these different areas of research, Celebrex may just be getting of the ground. 14 Conclusion After examining all aspects of Celebrex’s safety, it is clear that Celebrex is much safer than Vioxx both in terms of GI safety and cardiovascular risks. There have been more studies with strong results that exhibit the safety of Celebrex than the studies that imply that it may be unsafe. The bigger issue that now needs to be looked at is the over prescribing of the drug. Many physicians are impressed with the effectiveness of Celebrex and it has quickly become the drug of choice when it comes to fighting inflammation. Thus, Celebrex must remain dispensed for the patients it was originally intended for-those with extensive gastrointestinal problems who are in dire need of an anti-inflammatory medication regime. Obviously, it is important for all physicians to become aware of their clients’ health history and make educated decisions accordingly, but this problem is not solely a doctors’ responsibility. Patients must assume greater responsibility for themselves and take medications the way they were intended to be taken. Most importantly, the risks and benefits of taking any kind of medication must be weighed very carefully. 15 REFERENCES: Aw, T., Haas, S., Liew, D., Krum, H. Meta-analysis of cyclooxygenase-2 inhibitors and their effects on blood pressure. American Medical Association. (2005). 165:490-496. Baker, Christopher S.R.; Hall, Roger J.C.; Evans, Thomas J.; Pomerance, Ariela; Maclouf, Jacques; Creminon, Christophe; Yacoub, Magdi H.; Polak, Julia M. Cyclooxygenase-2 Is Widely Expressed in Atherosclerotic Lesions Affecting Native and Transplanted Human Coronary Arteries and Colocalizes With Inducible Nitric Oxide Synthase and Nitrotyrosine Particularly in Macrophages. Arteriosclerosis, Thrombosis & Vascular Biology. (March 1999).19(3):646-655. Chang, Ingrid J.; Harris, Raymond C. Are All COX-2 Inhibitors Created Equal? Hypertension. (February 2005). 45(2):178-180. Chenevard, Remy; Hurlimann, David; Bechir, Markus; Enseleit, Frank; Spieker, Lukas ; Hermann, Matthias; Riesen, Walter; Gay, Steffen; Gay, Renate E.; Neidhart, Michel; Michel, Beat; Luscher, Thomas F; Noll, Georg; Ruschitzka, Frank, Selective COX-2 Inhibition Improves Endothelial Function in Coronary Artery Disease. Circulation. (January 2003). 107(3):405-409. Crawford, A., White, J. Celecoxib-induced upper gastrointestinal hemorrhage and ulceration. Southern Medical Journal. (2002). 95:1444-1446. Deeks JJ, Smith LA, Bradley MD. Efficacy, tolerability, and upper gastrointestinal safety of celecoxib for treatment of osteoarthritis and rheumatoid arthritis: systematic review of randomised controlled trials. BMJ. (September 2002). 325(7365):619. Ekenel, Meltem, Avsar, Erol, Imeryuz, Nese, Yuksel, Meral, Haklar, Goncagul, Kocakaya, Ozan, Tozun, Nurdan. Effects of selective COX-2 inhibitors on the gastric permeability of sucrose: a controlled study with placebo and ibuprofen. European Journal of Gastroenterology and Hepatology. (2003). 15:403-406. Emery P, Zeidler H, Kvien TK, Guslandi M, Naudin R, Stead H, et al. Celecoxib versus diclofenac in longterm management of rheumatoid arthritis: randomised double-blind comparison. Lancet (1999). 354:210611. Gopez, J., Yue, H., Vasudevan, R., Malik, A., Fogelsanger, L., Lewis, S., Panikashivili, D., Shohami, E., Jansen, S., Narayan, R., Strauss, K. Cyclooxygenase-2-specific inhibitor improves functional outcomes, provides neuroprotection, and reduces inflammation in a rat model of traumatic brain injury. Congress of Neurological Surgeons. (2005). 56:590-604. Juni P., Rutjes A., Dieppe P. A. Are selective COX 2 inhibitors superior to traditional non steroidal antiinflammatory drugs? BMJ. (2002). 324:1287-1288. Kim P.S, Reicin A.S, Rofecoxib, Merck, and the FDA. NEJM. (December 2004). 351:2875-2878. Konstam M.A, Weir M.R, Reicin A, Shapiro D, Sperling R.S, Barr E, Gertz B.J. Cardiovascular Thrombotic Events in Controlled, Clinical Trials of Rofecoxib. Circulation: American Heart Association. (2001). 104: 2280. Langton P.E, Hankey G.J, Eikelboom J.W, Cardiovascular safety of rofecoxib (Vioxx): lessons learned and unanswered questions. Medical Journal of Australia. (2004). 10:524-525. Levesque, Linda E. BScPhm, MSc; Brophy, James M. MD, PhD; Zhang, Bin MSc The Risk for Myocardial Infarction with Cyclooxygenase-2 Inhibitors: A Population Study of Elderly Adults. Annals of Internal Medicine. (April 5, 2005).142(7):481-489. 16 Mamdani M, Rochon P, Juurlink DM, et al. Effect of selective cyclooxygenase 2 inhibitors and naproxen on short-term risk of acute myocardial infarction in the elderly. Arch Intern Med (2003). 163:481-486. Mamdani M, Rochon P, Juurlink DM, Kopp A, Anderson GM, Naglie G, Austin P, Laupacis A., Observational study of upper gastrointestinal hemorrhage in in elderly patients given selective cyclooxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs. BMJ (2002) 325:624. Mukherjee D, Nissen SE, Topol EJ.Risk of cardiovascular events associated with selective COX-2 inhibitors. The Journal of the American Medical Association. (2001). 8:954-9. Nachimuthu, S., Volfinzon, L., Gopal, L. Acute hepatocellular and cholestatic injury in a patient taking celecoxib. Postgrad Medical Journal. (2001). 77:548-550. Pascucci R.A. Use of nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 (COX-2) inhibitors: indications and complications. The Journal of the American Osteopathic Association. (2002). 102: 487489. Patel, T. N., Goldberg, K. C. Use of Aspirin and Ibuprofen Compared With Aspirin Alone and the Risk of Myocardial Infarction. Arch Intern Med. (2004). 164: 852-856. Rabausch, K., Bretschneider, E., Sarbia, M., Meyer-Kirchrath, J., Censarek, P., Pape, R., Fischer, J., Schror, K., Weber, A. Regulation of thrombomodulin expression in human vascular smooth muscle cells by COX-2-derived prostaglandins. Circulation. (2005). 96:e1-e6. Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: A randomised controlled trial. JAMA (2000). 284: 1247-1255. Anti-inflammatory and Upper Gastrointestinal Effects of Celecoxib in Rheumatoid Arthritis. Lee S. Simon, MD; Arthur L. Weaver, MD; David Y. Graham, MD; Alan J. Kivitz, MD; Peter E. Lipsky, MD; Richard C. Hubbard, MD; Peter C. Isakson, PhD; Kenneth M. Verburg, PhD; Shawn S. Yu, PhD; William W. Zhao, PhD; G. Steven Geis, PhD, MD. JAMA. (1999); 282:1921-1928. Solomon DH, Glynn RJ, Levin R, Avorn J. Nonsteroidal Anti-inflammatory Drug Use and Acute Myocardial Infarction. Arch Intern Med. (2002).162:1099-1104. Solomon D H, Schneeweiss S, Glynn R J. Relationship between selective cyclooxygenase-2 inhibitors and acute myocardial infarction in older adults. Circulation. (2004). 109:2068-2073. Solomon D H, Avorn J. Coxibs, Science and the Public Trust. Arch Intern Med. (2005). 165:158-160 Solomon, SE., McMurray, J., Pfeffer, M., Wittes, J., Fowler, R., Finn, P., Anderson, W., Zauber, A., Hawk, E., Bertagnolli, M. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. NEJM. (2005). 352:1071-1080. Sowers, James R. MD; White, William B. MD; Pitt, Bertram MD; Whelton, Andrew MD; Simon, Lee S. MD; Winer, Nathaniel MD; Kivitz, Alan MD; van Ingen, Hein MD; Brabant, Thomas MD; Fort, John G. MD; for the Celecoxib Rofecoxib Efficacy and Safety in Comorbidities Evaluation Trial (CRESCENT) Investigators The Effects of Cyclooxygenase-2 Inhibitors and Nonsteroidal Anti-inflammatory Therapy on 24-Hour Blood Pressure in Patients With Hypertension, Osteoarthritis, and Type 2 Diabetes Mellitus. Arch Intern Med. (January 2005). 165(2):161-168. Tanaka, T., Delong, P., Amin, K., Henry, A., Kruklitis, R., Kapoor, V., Kaiser, L., Albelda, S. Treatment of lung cancer using clinically relevant oral doses of the cyclooxygenase-2 inhibitor rofecoxib. Annals of Surgery. (2005). 241:168-178. 17 Tive L. Celecoxib clinical profile. Rheumatology (Oxford). (December 2000). 39 Suppl 2:21-8; discussion 57-9. Topol, Eric J. Failing the Public Health - Rofecoxib, Merck, and the FDA. New England Journal of Medicine. (October 2004).351(17):1707-1709. Waskewich, C., Blumenthal, R., Li, H., Stein, R., Goldenberg, D., Burton, J. Celecoxib Exhibits the Greatest Potency amongst Cyclooxygenase (COX) Inhibitors for Growth Inhibition of COX-2-negative Hematopoietic and Epithelial Cell Lines. Cancer Research. (2002) 62:2029-2033. Wooltorton, E. What's all the fuss? Safety concerns about COX-2 inhibitors rofecoxib (Vioxx) and celecoxib (Celebrex). Canadian Medical Association Journal. (June 25, 2002). 166 (13). Wright J.M. The double-edged sword of COX-2 selective NSAIDs. Canadian Medical Association Journal. (2002). 167: 10. 18