Thoracic Outlet Syndrome
advertisement

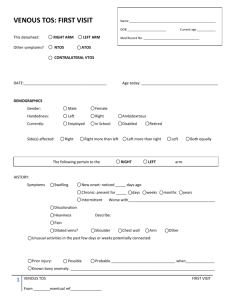
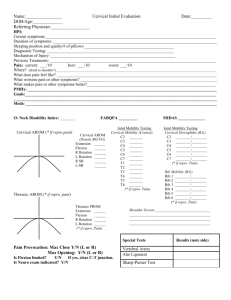
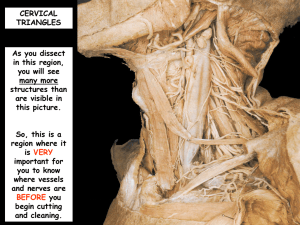
Thoracic Outlet Syndrome Wilbourn’s Classification 1. Vascular i. Arterial – major and minor ii. Venous 2. Neurogenic i. True ii. Disputed Arterial 1-2% Acute events such as thrombosis easy to diagnose (pain, pallor, pulselessness and parasthesia) May present with coolness of hand, claudication, unilateral Raynauds or fingertip ulcerations Affected arm has a lower BP of >20mmHg difference (a reliable indicator of arterial involvement) Full developed cervical rib seen in 50% Other 50% thought to have some other type of bony anomaly Venous 2-3% sudden effort induced thrombosis (Paget-Schroetter syndrome) or at rest with the extremity in a compromised position for a prolonged period may develop large superficial collaterals with more chronic disease Acute cases present with cyanosis, swelling and pain Mostly seen in muscular young males after exercise True Neurogenic 1:1,000,000 A typical patient is a young, thin female with a long neck and dropping shoulders usually C8-T1 distribution Hypothenar atrophy, decreased grip and sensation present as isolated hand intrinsic muscle atrophy without any pain (GilliatSumner hand) Disputed Neurogenic Wide range of complaints No objective findings on electrodiagnostics or imaging. Epidemiology Overall F>M 3.5:1 Neurologic - Female-to-male ratio approximately 3.5:1 Venous - More common in males than in females Arterial - No sexual predilection Much more common in countries where TOCS is a legitimate work related condition Some morphotypes predispose to the syndrome: poor muscular development, droop of scapula, obesity and breast hypertrophy. Anomalous cervical ribs seen in 0.17-0.74%, with a higher percentage of cervical ribs in women Anatomy 3 areas of compression 1. interscalene triangle 2. costoclavicular triangle 3. pectoralis minor/subcoracoid space most common compression sites in patients with TOS are within the scalene triangle and the subcoracoid space Interscalene Triangle Boundaries 1. Anterior – scalenius anterior 2. Posterior – scalenius medius 3. Inferior – 1st rib Compressed by 1. Cervical rib 0.5% of population bilateral in 50-80% may be compressed by complete rib or anlage from incomplete rib Cervical rib growth is suppressed by full contribution of lower spinal nerve roots to plexus – association between cervical ribs and a prefixed plexus. 2. Abnormal scalene insertion V shape or U shape insertions of scalenius anterior and medius Increased downslope of 1st rib – more common in women Costoclavicular space Boundaries 1. Anterior – clavicle, subclavius and costocoracoid ligament 2. Posteromedial – 1st rib 3. Posterolateral – superior border of scapula Compressed by 1. Hypermobile shoulder movements 2. Hypertrophied subclavius muscle Subcoracoid space Compression by 3 mechanisms 1. Arm abduction stretches neurovascular bundle around coracoid 2. External scapular rotation – further stretches the same 3. Abduction also tenses the pectoralis minor tendon Clinical Neurologic Chronic insidious pain involving shoulder girdle, neck and upper back Pain, particularly in the medial aspect of the arm, forearm, and the ring and small digits Paresthesias, often nocturnal, awakening the patient with pain or numbness Loss of dexterity Cold intolerance Headache Venous Pain, often in younger men and often associated with strenuous work Arterial Pain Claudication Often in young adults with a history of vigorous arm activity Examination Posture Slouch forward Large breasted Shoulder droop Masses in supra/infraclavicular fossae Percussion test Sensation Dermatomal Motor Reflexes Provocative Tests In general unreliable as 90% of asymptomatic patients will be positive neurological response (paresthesias) appears more valuable than the vascular response (reduced radial pulse intensity). The most predictive maneuver seems to be the abduction/external rotation of the arm 1. Adson’s test / scalene test With arm at side, patient hyperextends neck, turns face towards affected side and inhales deeply Test Positive test = diminution or obliteration of radial pulse 2. Halstead Maneuver/costoclavicular test Both arms at side, patient moves shoulders downwards and backwards – protruding chest to draw clavicle against 1st rib test was modified by Halstead to include downward traction of the patient's arms by the examiner and monitoring of the radial pulse 3. Wright’s Hyperabduction Maneuver Arm is externally rotated and abducted 180 and patient inhales Only flex elbow minimally (minimise cubital tunnel) Positive if symptoms occur <1min Indicated subcoracoid impingement 4. Roo’s/ EAST test 90 abduction and external rotation (stick-up test) pumps hands open/close quickly for 3 minutes evaluates all 3 types of thoracic outlet syndrome Positive test if reproduce symptoms or rapid fatiguibility Although a single positive test is probably meaningless, more than 2 positive responses is significant and should be combined with history, other findings and diagnostic studies Scalene muscle block-temporary relief of symptoms following anterior scalene muscle infiltration with 4 cc of 1% lidocaine appears a useful diagnostic tool for TOS. Furthermore, there isa high correlation between good response to the block and improvement following scalenectomy. Investigations Xrays Cervical spine Chest Color flow duplex scanning 92% sensitive in vascular TOCS CT Useful to help rule out other pathologies (Pancoast tumor, disc prolapse) Arteriogram (indications) Evidence of peripheral emboli in the upper extremity Suspected subclavian stenosis or aneurysm (eg, bruit or abnormal supraclavicular pulsation) Blood pressure differential greater than 20 mm Hg Obliteration of radial pulse during EAST Venography (indications) Persistent or intermittent edema of the hand or arm Peripheral unilateral cyanosis Prominent venous pattern over the arm, shoulder, or chest Identification of significant collaterals may help with operative planning, and may determine the type of exposure used in order to limit damage to these collaterals Electrophysiology Nerve conduction evaluation via root stimulation and F wave is the best direct approach to evaluation of neurologic TOS. Electromyography (EMG) is unreliable and does not provide objective evidence of TOS. Management Nonoperative First line treatment in disputed neurogenic type Arterial type unlikely to respond Physical therapy Postural exercises, stretching, abdominal breathing used to relieve muscular tension and pain are beneficial. Pain control Medications TENS Heat/ice packs Approximately 60% of patients improve significantly with conservative treatment alone and avoid surgery The indication for surgical treatment of neurogenic TOS is the failure of conservative treatment in a patient with disability so severe that the patient is unable to work or live comfortably. Most physicians prescribe 3-12 months of physical therapy prior to considering surgical decompression of the thoracic outlet. venous TOS–related effort thrombosis that relies on anticoagulation and arm elevation leaves 74% of patients with residual disability and 12% with significant complication. Thrombolytic therapy generally is preferred over venous thrombectomy; however, thrombectomy still may have a role in some cases with low surgical risk and contraindication to thrombolytic therapy. Although thrombolytic therapy alone is superior to simple anticoagulation in patients who present with venous TOS, the patients who achieve the best results are those who are treated with thrombolytics and surgical decompression. Surgical Indications 1. Impending or acute vascular catastrophe (vascular TOS) 2. Intractable pain 3. Failure of conservative treatment 4. Significant neurologic deficit Approaches 1. Transaxillary Most used, popularised by Roos a transverse incision is made over the 3rd rib just inferior to the axillary hairline and deepened between the pectoralis major and the latissimus dorsi to the chest wall. Preserve intercostobrachial nerve 2. Supraclavicular horizontal incision is made parallel and 2cm above the clavicle, extending from the sterno-cleido-mastoid muscle (SCM) to the anterior border of the trapezius infraclavicular counter-incision can be performed for added exposure After platysma incision, the clavicular head of SCM is either retracted medially or incised and then repaired at the end of operation. The supraclavicular pad of fat, of varying bulk, is dissected from below upward; the omo-hyoid muscle is incised; the cervical transverse vessels may be ligated. One reaches the plane of the anterior scalene muscle; the phrenic nerve coursing obliquely on the surface of the muscle must be protected in order to perform the anterior scalenectomy. Beware risk of phrenic (lateral to medial over scalenius anterior) and long thoracic nerve (exits posterior border of scalenius medius) injury 3. Posterior subscapular incision between the medial border of the scapula and the cervicodorsal spinous processes, division of trapezius and rhomboid muscles, exposure of the posterior upper rib cage, resection of 1st rib and of posterior and middle scalene muscles. The BP is approached from behind, at the level of spinal nerves and trunks. This approach, extensive in regard to muscle incision, is reserved to "complicated TOS" Surgical recommendations 1. Excise and release all anomalous anatomy 2. Resection of 1st rib 3. Release /excision of anterior/middle scalene 4. Neurolysis of brachial plexus as indicated Arterial TOS Supra/infraclavicular approach. Transaxillary does not give adequate exposure Need to excise anomalous rib and arterial reconstruction as required Venous TOS Thrombolysis followed by 1st rib resection For occlusions older than 10-14 days, chances for a successful thrombolysis are poor A lesion longer than 2 cm may require venous bypass or a jugular vein turndown procedure. A consensus statement favored conservative treatment with anticoagulation under these circumstances and concluded that venous bypass should be reserved for only those patients with disabling symptoms and serious complications. Neurogenic TOS Removing the anomaly Release/remove anterior and middle scalene Excise 1st rib Complications 1. Recurrence 5-25% Lowest recurrence in those undergoing combined 1st rib resection and scalenectomy 2. Nerve injuries Phrenic, long thoracic, and sympathetic nerves 3. lymph leak 4. bleeding