Health Insurance Appeal Letter: Assistant Surgeon Denial
advertisement
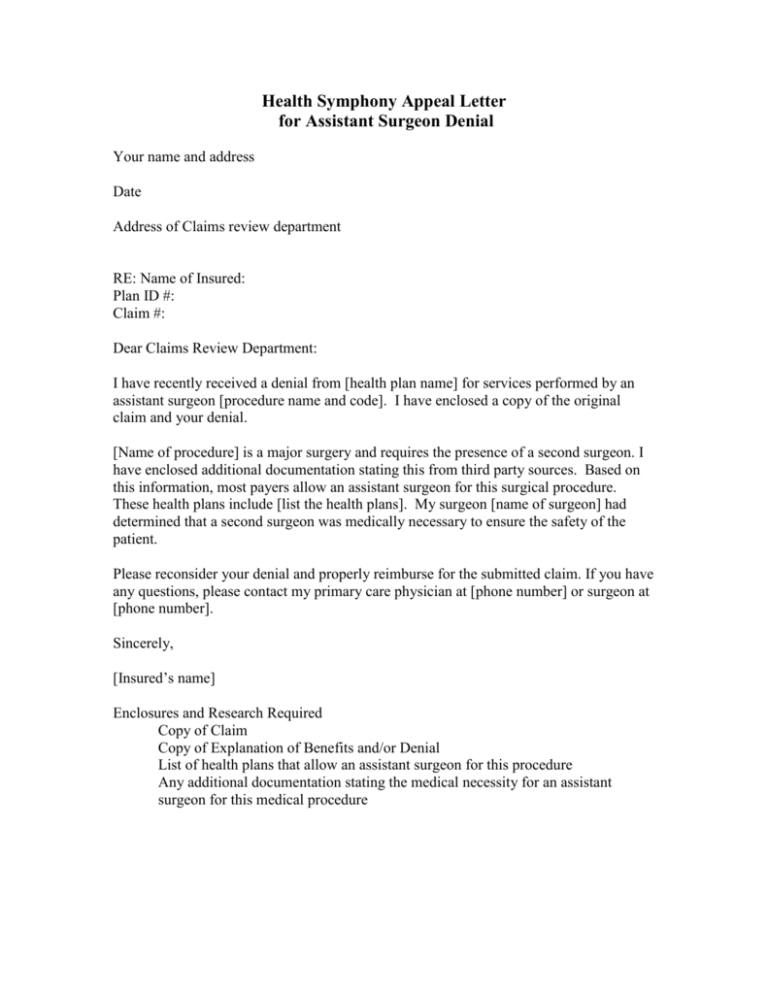
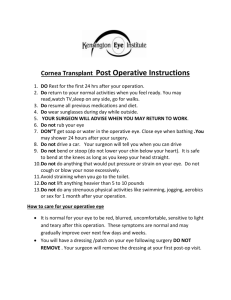
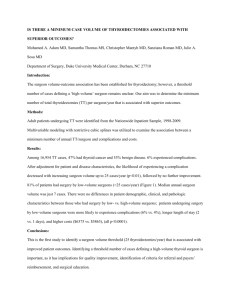
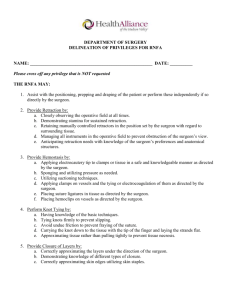
Health Symphony Appeal Letter for Assistant Surgeon Denial Your name and address Date Address of Claims review department RE: Name of Insured: Plan ID #: Claim #: Dear Claims Review Department: I have recently received a denial from [health plan name] for services performed by an assistant surgeon [procedure name and code]. I have enclosed a copy of the original claim and your denial. [Name of procedure] is a major surgery and requires the presence of a second surgeon. I have enclosed additional documentation stating this from third party sources. Based on this information, most payers allow an assistant surgeon for this surgical procedure. These health plans include [list the health plans]. My surgeon [name of surgeon] had determined that a second surgeon was medically necessary to ensure the safety of the patient. Please reconsider your denial and properly reimburse for the submitted claim. If you have any questions, please contact my primary care physician at [phone number] or surgeon at [phone number]. Sincerely, [Insured’s name] Enclosures and Research Required Copy of Claim Copy of Explanation of Benefits and/or Denial List of health plans that allow an assistant surgeon for this procedure Any additional documentation stating the medical necessity for an assistant surgeon for this medical procedure