Mohamed_Adam_Adam_MA
advertisement

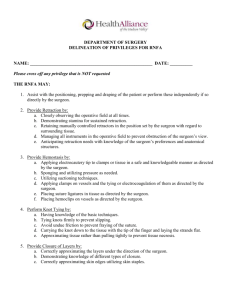
IS THERE A MINIMUM CASE VOLUME OF THYROIDECTOMIES ASSOCIATED WITH SUPERIOR OUTCOMES? Mohamed A. Adam MD, Samantha Thomas MS, Christopher Mantyh MD, Sanziana Roman MD, Julie A. Sosa MD Department of Surgery, Duke University Medical Center, Durham, NC 27710 Introduction: The surgeon volume-outcome association has been established for thyroidectomy; however, a threshold number of cases defining a ‘high-volume’ surgeon remains unclear. Our aim was to determine the minimum number of total thyroidectomies (TT) per surgeon/year that is associated with superior outcomes. Methods: Adult patients undergoing TT were identified from the Nationwide Inpatient Sample, 1998-2009. Multivariable modeling with restrictive cubic splines was utilized to examine the association between a minimum number of annual TT/surgeon and complications and costs. Results: Among 16,954 TT cases, 47% had thyroid cancer and 53% benign disease. 6% experienced complications. After adjustment for patient and disease characteristics, the likelihood of experiencing a complication decreased with increasing surgeon volume up to 25 cases/year (p<0.01), followed by no further improvement. 81% of patients had surgery by low-volume surgeons (<25 cases/year) (Figure 1). Median annual surgeon volume was just 7 cases. There were no differences in patient demographic, clinical, and pathologic characteristics between those who had surgery by low- vs. high-volume surgeons; patients undergoing surgery by low-volume surgeons were more likely to experience complications (6% vs. 4%), longer length of stay (2 vs. 1 days), and higher costs ($6375 vs. $5863), (all p<0.0001). Conclusions: This is the first study to identify a surgeon volume threshold (25 thyroidectomies/year) that is associated with improved patient outcomes. Identifying a threshold number of cases defining a high-volume thyroid surgeon is important, as it has implications for quality improvement, identification of criteria for referral and payers’ reimbursement, and surgical education. Figure 1. Smoothed restricted cubic spline plot of the adjusted log odds ratio of experiencing any complication vs. the number of total thyroidectomy performed by a surgeon in HCUP-NIS. Predicted hazards ratios were estimated from a proportional hazards model adjusting for covariates. The dotted lines represent the 95% confidence intervals about the predicted odds ratio (solid line). The dashed line represents the regression lines in the change point estimation. They intersect at a value of 25 cases per year, as indicated by the solid vertical line.