You are working nite shift on a med/surg unit caring for 8 patients
advertisement
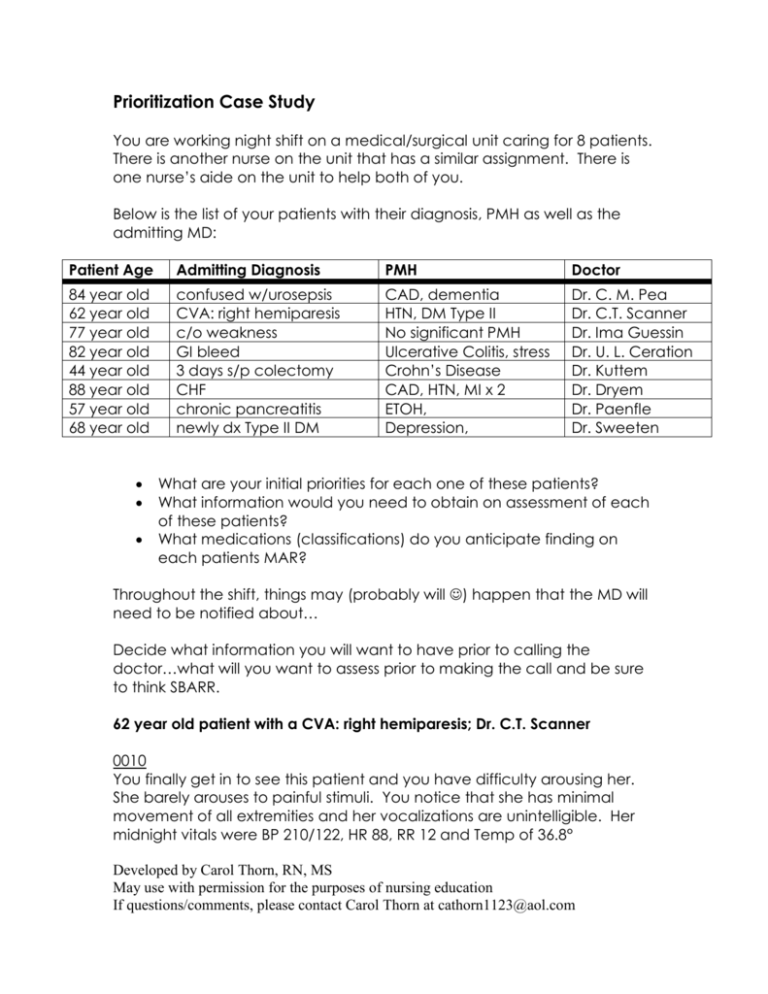
Prioritization Case Study You are working night shift on a medical/surgical unit caring for 8 patients. There is another nurse on the unit that has a similar assignment. There is one nurse’s aide on the unit to help both of you. Below is the list of your patients with their diagnosis, PMH as well as the admitting MD: Patient Age Admitting Diagnosis PMH Doctor 84 year old 62 year old 77 year old 82 year old 44 year old 88 year old 57 year old 68 year old confused w/urosepsis CVA: right hemiparesis c/o weakness GI bleed 3 days s/p colectomy CHF chronic pancreatitis newly dx Type II DM CAD, dementia HTN, DM Type II No significant PMH Ulcerative Colitis, stress Crohn’s Disease CAD, HTN, MI x 2 ETOH, Depression, Dr. C. M. Pea Dr. C.T. Scanner Dr. Ima Guessin Dr. U. L. Ceration Dr. Kuttem Dr. Dryem Dr. Paenfle Dr. Sweeten What are your initial priorities for each one of these patients? What information would you need to obtain on assessment of each of these patients? What medications (classifications) do you anticipate finding on each patients MAR? Throughout the shift, things may (probably will ) happen that the MD will need to be notified about… Decide what information you will want to have prior to calling the doctor…what will you want to assess prior to making the call and be sure to think SBARR. 62 year old patient with a CVA: right hemiparesis; Dr. C.T. Scanner 0010 You finally get in to see this patient and you have difficulty arousing her. She barely arouses to painful stimuli. You notice that she has minimal movement of all extremities and her vocalizations are unintelligible. Her midnight vitals were BP 210/122, HR 88, RR 12 and Temp of 36.8° Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com 77 year old patient with c/o weakness; Dr. Ima Guessin 0100 This patient is complaining of not being able to get to sleep. He states that he usually takes something at home every night to help him sleep. He wants you to call the doctor and get something for him. 84 year old confused patient with urosepsis; Dr. C. M. Pea 0210 Aide comes to tell you that the patient is very confused, trying to get out of bed…”was a little confused at the beginning of the shift but nothing like this”. The patient is now screaming that people are ‘trying to kill him’ and waking up all the other patients on the unit. You need to notify the doctor of this change…what are you going to tell him/her? Unable to get vital signs or assessment at this time. 88 year old patient with CHF; Dr. Dryem 0245 The patient calls you in to tell you that she is having difficulty ‘getting enough air’. You notice that her respirations are much more labored and wet sounding than your earlier assessment. 82 year old patient with GI bleed; Dr. Butts 0330 The aide tells you that she just got this patient back to bed after needing to use the bathroom. The patient was weak and shaky on the way back to bed, stating he thought he was going to pass out. Now feels better after lying down. His vitals were stable at midnight. 44 year old patient 3days s/p colectomy; Dr. Kuttem 0400 The aide comes to tell you that the patient’s vital signs are really different than when she took them at midnight. The temperature is now 103.8 with a pulse of 126. Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com 57 year old patient with chronic pancreatitis; Dr. Paenfle 0430 The aide comes to tell you that your patient is getting dressed in the room and says he is ‘going home’ because he can’t get enough pain relief here. You are unable to give more pain medication at this time. The patient wants to sign out AMA unless something is done. 68 year old patient with newly diagnosed Type II DM; Dr. Sweeten 0545 The aide comes to tell you that the patient’s CBG is 408 and the patient is really sleepy. You have an order for sliding scale insulin coverage but the order says to notify the MD for any blood glucose > 400. Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com