Septic Shock Unfolding Case Study - NC-NET
advertisement

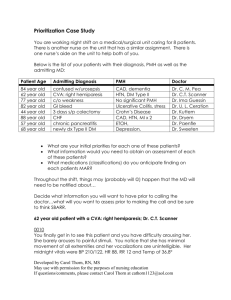
Septic Shock Unfolding Case Study (2 parts) Concept: Perfusion You are receiving the following report from the off going nurse: In room #1 is Melody Bloom. She is a 56 year old woman who has been here for 8 days. She initially went to the med/surg unit post-operatively after an exploratory laparotomy for a perforated bowel due to ulcerative colitis. She came to the unit with symptoms of peritonitis and pneumonia which progressed despite antibiotics and she is now suffering from septic shock. Also, her WBC’s continue to go up and are now at 32,000 despite the antibiotics she has been on. She is on vasopressors as well as receiving fluid boluses to keep her blood pressure up above 85 systolic. Yesterday she received a total of 4.5 liters of fluid to maintain her pressure. She is on the ventilator to help support her respiratory status. We have added PEEP to her vent settings as there are signs that she is going into ARDS…but the PEEP is negatively affecting her hemodynamic status. We are walking a tight rope trying to titrate her fluids, vasopressors and PEEP to keep her blood pressure within an acceptable range. Unfortunately she may also be developing multi-system organ failure as it now seems her kidneys may be failing and her gut is not working. Her husband comes in everyday but his visits are becoming shorter and shorter as her condition declines. He just wants her suffering to end and to be taken off the ventilator. We aren’t sure her condition is irreversible at this time so it’s a tough one to deal with. The nurses have noticed that ever since his visits have become shorter, she is becoming more and more withdrawn…so you never know what he may be saying to her when they are alone in the room. He’s probably just telling her to give up already. Her son is across country, calls several times per day but can’t come visit until next week. He gives every indication that he thinks his mom is a survivor and can pull through this. The patient and her husband have no children together. Answer the following questions: Are there any ethical, cultural or age-related issues associated with this patient? If so, what are they? What would you anticipate noticing when you walk into the patient’s room? What medical treatment/nursing interventions would you anticipate finding on the plan of care? What medications would you anticipate finding on the patient’s medication administration record (MAR)? If you could ask the off-going nurse only 3 questions, what would they be and why? Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com If you were going to do a focused assessment on this patient, what would you concentrate on and why? What issues can you identify as being a priority in caring for this patient? What are some potential complications that could occur in this patient that the nurse needs to be aware of/monitor for? What members of the multi-disciplinary team have been/or will be involved in the care of the patient in the case study and what was their role? Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com Septic Shock Unfolding Case Study – Part II 2 hours later: Alarms in your patient’s room start to sound. In going into the room you find that your patient is in severe respiratory distress despite being on the ventilator. Her current oxygen saturations are 72% however they may be inaccurate due to the use of vasopressors. Her BP is 78/35, HR 118/m and respiratory rate of 26/minute. Your coworkers come in and immediately begin to bag her with the ambu-bag while you notify the physician. Prior to leaving the room, you notice that her chest has uneven expansion and when you listen to her lungs, you hear minimal breath sounds on the right side of her chest. Answer the following questions: What do you think is going on with this patient? What might have caused this complication? What additional assessment do you need to perform for this patient? What lab/diagnostic tests do you believe will be ordered? What do you anticipate them showing? What can an RN initially do for this patient? What do you need to tell the MD what calling him/her? Utilize the SBAR format to provide information to the physician. Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com