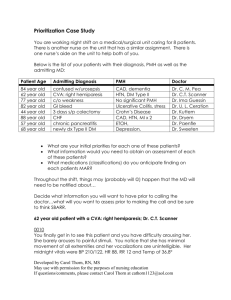
Prioritization Case Study You are working night shift on a medical/surgical unit caring for 8 patients. There is another nurse on the unit that has a similar assignment. There is one nurse’s aide on the unit to help both of you. Below is the list of your patients with their diagnosis, PMH as well as the admitting MD: Patient Age Admitting Diagnosis PMH Doctor 84-year-old 62-year-old 77-year-old 82-year-old 44-year-old 88-year-old 57-year-old 68-year-old confused w/urosepsis CVA: right hemiparesis c/o weakness GI bleed 3 days s/p colectomy CHF chronic pancreatitis newly dx Type II DM CAD, dementia HTN, DM Type II No significant PMH Ulcerative Colitis, stress Crohn’s Disease CAD, HTN, MI x 2 ETOH, Depression, Dr. C. M. Pea Dr. C.T. Scanner Dr. Ima Guessin Dr. U. L. Ceration Dr. Kuttem Dr. Dryem Dr. Paenfle Dr. Sweeten 1. 62-year-old patient with a CVA: right hemiparesis; Dr. C.T. Scanner 0010 You finally get in to see this patient and you have difficulty arousing her. She barely arouses to painful stimuli. You notice that she has minimal movement of all extremities and her vocalizations are unintelligible. Her midnight vitals were BP 210/122, HR 88, RR 12 and Temp of 36.8° 2. 77-year-old patient with c/o weakness; Dr. Ima Guessin 0100 This patient is complaining of not being able to get to sleep. He states that he usually takes something at home every night to help him sleep. He wants you to call the doctor and get something for him. 3. 84-year-old confused patient with urosepsis; Dr. C. M. Pea 0210 Aide comes to tell you that the patient is very confused, trying to get out of bed…” was a little confused at the beginning of the shift but nothing like this”. The patient is now screaming that people are ‘trying to kill him’ and waking up all the other patients on the unit. You need to notify the doctor of this change…what are you going to tell him/her? Unable to get vital signs or assessment at this time. 4. 88-year-old patient with CHF; Dr. Dryem 0245 The patient calls you in to tell you that she is having difficulty ‘getting enough air’. You notice that her respirations are much more labored and wet sounding than your earlier assessment. 5. 82-year-old patient with GI bleed; Dr. Butts 0330 The aide tells you that she just got this patient back to bed after needing to use the bathroom. The patient was weak and shaky on the way back to bed, stating he thought he was going to pass out. Now feels better after lying down. His vitals were stable at midnight. 6. 44-year-old patient 3days s/p colectomy; Dr. Kuttem 0400 The aide comes to tell you that the patient’s vital signs are different than when she took them at midnight. The temperature is now 103.8 with a pulse of 126. 7. 57-year-old patient with chronic pancreatitis; Dr. Paenfle 0430 The aide comes to tell you that your patient is getting dressed in the room and says he is ‘going home’ because he can’t get enough pain relief here. You are unable to give more pain medication at this time. The patient wants to sign out AMA unless something is done. 8. 68-year-old patient with newly diagnosed Type II DM; Dr. Sweeten 0545 The aide comes to tell you that the patient’s CBG is 408 and the patient is sleepy. You have an order for sliding scale insulin coverage, but the order says to notify the MD for any blood glucose > 400. Questions 1. What are your initial priorities for each one of these patients? For the 84 y.o. pt with urosepsis, my priorities would be to initially assess for a fever, obtain a urine specimen for a culture, administer antibiotics intravenously or orally as prescribed after the 3-5 day afrebrile period. For the 62 y.o. pt with CVA: right hemiparesis, my priorities would be to initially assess for airway patency, slow and bounding pulse rate, cheyne-stokes respirations, hypertension, facial drooping, dysphagia, and speech, writing changes, and cranial nerves V, VII, IX, X, and XII, etc. For the 77 c/o weakness, my priorities would be to initially assess through Palliative questions: such as what brings it on? What were you doing when you first noticed it? What makes it better? Worse? Quality: How does it feel? How intense/severe is it? Region: Where is it? Does it spread anywhere? Severity Scale: How bad is it on a scale of 1-10? Is it getting better, worse, staying the same? Timing: Onset, exactly when did it firs occur? Duration: how long did it last? Frequency, how often does it occur? Understand Patient’s Perception of the problem: what do you think it means? For the 82 y.o. with GI bleeds, my priorities would be to initially asses vital signs, signs of bleeding, pain, hematemesis, signs of anemia such as weakness, fatigue, hemoglobin and hematocrit levels For the 44 y.o. with 3 days s/p colectomy, my priorities would be to Monitor for infection and pain. I would initially assess the site for abnormal bleeding, fever, increase pulse rate, tachycardia. Also, I would listen to bowel sounds, monitor intake/output and frequently assess pain levels, and administer pain medication For the 88 y.o. with CHF, my priorities would be to assess pulmonary edema, such as restlessness, anxiety, increased crackles, tachypnea, tachycardia, pink frothy sputum. Also, chronic fatigue, heart rhythm/sounds, pulse rate For the 57 y.o. with chronic pancreatitis, my priorities would be to assess for abdominal pain/tenderness in the left upper quadrant, steatorrhea, foul-smelling stools, weight loss, jaundice and signs of diabetes mellitus For the 68 y.o. newly dx Type II DM, my priorities would be to assess for Polyuria, polydipsia, blurred vision, slow wound healing, and signs of inadequate circulation to the feet 2. What information would you need to obtain on assessment of each of these patients? For the 84 y.o. pt with urosepsis, I would need to obtain information concerning the urinary system by assessing issues such as frequency, urgency, nocturia, dysuria, polyuria, oliguria, hesitancy, incontinence, and obtain history of urinary disease, kidney disease, kidney stones, urinary tract infections or pain in the groin, suprapubic region, or low back. For the 62 y.o. pt with CVA, I would need to obtain information of neurologic system by assessing issues such as history of seizure disorder, stroke, blackout, weakness, tic, tremor, paralysis, coordination problems, numbness, or tingling, memory disorder. For the 77 y.o c/o weakness, I would need to obtain information concerning the musculoskeletal system by assessing for issues such as deformity, limitation of motion, weakness, gait problems or problems with coordination, limited range of motion. For the 82 yo with GI bleeds, I would need to obtain information concerning the GI system by assessing for ulcer formation, nausea, vomiting, black stools, and flatulence For the 44 y.o. with 3 days s/p colectomy, I would need to obtain baseline information such a pain levels, last bowel movement, activity level, current medications, nausea, vomiting, rectal bleeding, and current nursing orders For the 88 y.o. with CHF, I would need to obtain information concerning the cardiac system by assessing chest pain, palpitation, cyanosis, dyspnea when walking one flight of stairs, edema, hypertension, or coronary artery disease For the 57 y.o. with chronic pancreatitis, I would need to obtain information concerning the GI system by assess family history, alcohol use, biliary tract disease, peptic ulcer disease, hyperlipidemia, hypercalcemia, and labs For the 68 y.o. newly dx Type II DM, I would need to obtain information concerning diet, exercise, kidney function, urine specific gravity, and glucose monitoring 3. What medications (classifications) do you anticipate finding on each patients MAR? For the 84 y.o. pt with urosepsis the medication classifications that I would anticipate finding on the MAR are: Urinary Tract Antiseptics (Cinoxacin, Methenamine, Nalidixic acid, Nitrofurantion), Fluoroquinolones (Ciprofloxacin, Enoxacin, Gemifloxacin, Levofloxacin, etc), Sulfonamides (Sulfadiazine, sulfamethizole, Sulfamethoxazole, etc For the 62 y.o. pt with CVA, the medication classifications that I would anticipate finding on the MAR are: Anticoagulant (heparin) Antiplatelet (Aspirin), Thrombolytics (plasmingogen activator), Osmotic Diuretics (mannitol) or Diurectics (Lasix). For the 77 y.o. pt c/o weakness, I would not anticipate finding medication classifications on the MAR, but I would anticipate finding nursing orders that say: increase fluids, cluster activities ( for rest), active range of motion exercises, and eating balance meals/or liquid nutritional supplements For the 82 y.o. with GI bleeds, the medication classifications that I would anticipate finding on the MAR are: H2-receptor antagonist (Cimetidine, Famotidine, Nizatidine, Ranitidine), Proton Pump Inhibitors (Esomeprazole, Lansorprazole, Omeprazole, etc), and mucosal barrier protectants For the 44 y.o. with 3 days s/p colectomy, the medication classifications that I would anticipate finding on the MAR are: opioid analgesics, antibiotics/anti-infective to help decrease bowel flora and reduce infection, stool softeners or laxatives, H2-receptor antagonist, Proton Pump Inhibitors For the 88 y.o. with CHF, the medication classifications that I would anticipate finding on the MAR are: ACE inhibitors, Angiotensin II receptor blockers, Diuretics, Digoxin, Vasodilators, or Morphine For the 57 y.o. with chronic pancreatitis, the medication classifications that I would anticipate finding on the MAR are: Pancreatic Enzyme Replacements, Insulin/hypoglycemic medications For the 68 y.o. newly dx Type II DM, the medication classifications that I would anticipate finding on the MAR are: oral antidiabetic meds, or Insulin therapy Decide what information you will want to have prior to calling the doctor…what will you want to assess prior to making the call and be sure to think SBAR. 62 year old patient with a CVA: right hemiparesis; Dr. C.T. Scanner 0010 You finally get in to see this patient and you have difficulty arousing her. She barely arouses to painful stimuli. You notice that she has minimal movement of all extremities and her vocalizations are unintelligible. Her midnight vitals were BP 210/122, HR 88, RR 12 and Temp of 36.8° S- Dr. Scanner, this is Aneva Taylor, Student nurse on neuro unit. I am calling you about a 62 y.o. pt with a decrease level of conscious. I have difficulty arousing her. She barely arouses to painful stimuli, has decrease movement, and her vocalizations are unintelligible. B- A 62 y.o. female patient who presents with a CVA right hemiparesis. A- Most recent VS: BP 210/122, HR 88, RR 12 and Temp of 36.8° R- The pt could benefit from an emergency team STAT for her decrease conscious level and a follow up to reassess her neurological status. 77 year old patient with c/o weakness; Dr. Ima Guessin 0100 This patient is complaining of not being able to get to sleep. He states that he usually takes something at home every night to help him sleep. He wants you to call the doctor and get something for him. S- Dr. Guessin, this is Aneva Taylor, Student nurse on the Med Surg unit. I am calling about a 77 y.o. pt that is complaining of not being able to get to sleep. B- A 77 y.o. pt with c/o weakness, and not being able to get to sleep. A-The pt is unable to get to sleep. R- The pt could benefit from a sleep aid to help improve his rest and a follow up to reassess his medication treatments 84 year old confused patient with urosepsis; Dr. C. M. Pea 0210 Aide comes to tell you that the patient is very confused, trying to get out of bed…”was a little confused at the beginning of the shift but nothing like this”. The patient is now screaming that people are ‘trying to kill him’ and waking up all the other patients on the unit. You need to notify the doctor of this change…what are you going to tell him/her? Unable to get vital signs or assessment at this time. S- Dr. Pea, this is Aneva Taylor, Student nurse on the Med Surg unit. I am calling about a 84 y.o. pt very confused, and is trying to get out of bed. The situation has worsened since the beginning of the shift and, currently, the pt is now screaming that people are “trying to kill him” and waking up all the other pt’s on the unit. B- A 84 y.o. confused pt admitted with urosepsis who condition has worsen since the beginning of the shift A-The pt is confused and currently showing signs of delusions R- The pt could benefit from a neurological exam and follow up for a psych evaluation as well 88 year old patient with CHF; Dr. Dryem 0245 The patient calls you in to tell you that she is having difficulty ‘getting enough air’. You notice that her respirations are much more labored and wet sounding than your earlier assessment. S- Dr. Dryem, this is Aneva Taylor, Student nurse on the Med Surg unit. I am calling you about an 88 y.o. pt that is having difficulty getting enough air. Also, I notice that her respirations are much more labored and wet sounding than my earlier assessment B- A 88 y.o. pt admitted with CHF A-The pt currently displays wet sounding and labored respirations R- The pt could benefit from respiratory therapy and reevaluation for medications treatment as well 82 year old patient with GI bleed; Dr. Butts 0330 The aide tells you that she just got this patient back to bed after needing to use the bathroom. The patient was weak and shaky on the way back to bed, stating he thought he was going to pass out. Now feels better after lying down. His vitals were stable at midnight. S- Dr. Butts, this is Aneva Taylor, Student nurse on the GI unit. I am calling you about an 82 y.o. pt that needed to use the bathroom and on the way back to bed, the pt was weak and shaky and stated that he thought he was going to pass out. But he said that he feels better after lying down B- 82 y.o. pt admitted with GI bleed A- The pt vitals were stable at midnight R- The pt could benefit from more lab work and an evaluation for a colonoscopy 44 year old patient 3 days s/p colectomy; Dr. Kuttem 0400 The aide comes to tell you that the patient’s vital signs are really different than when she took them at midnight. The temperature is now 103.8 with a pulse of 126. S- Dr. Kuttem, this is Aneva Taylor, Student nurse on the GI unit. I am calling you about a 44 y.o. pt whose temp is now 103.8 with a pulse of 126 B- 44 y.o. pt 3 days s/p colectomy, Temp. 103.8 with a pulse of 126 A- The pt’s’ temp is now 103.8 and pulse of 126 since midnight R- This pt could benefit from blood cultures, and an infectious team evaluation 57 year old patient with chronic pancreatitis; Dr. Paenfle 0430 The aide comes to tell you that your patient is getting dressed in the room and says he is ‘going home’ because he can’t get enough pain relief here. You are unable to give more pain medication at this time. The patient wants to sign out AMA unless something is done. S- Dr. Peanfle, this is Aneva Taylor, Student nurse on the GI unit. I am calling you about a 57 y.o. who is experiencing pain and says that he wants to sign out AMA unless he gets more pain relief B- 57 y.o. pt admitted with chronic pancreatitis. Patient is currently experiencing severe pain A- pt states that he can’t get enough pain relief R- This pt could benefit from reevaluation for pain medications 68 year old patient with newly diagnosed Type II DM; Dr. Sweeten 0545 The aide comes to tell you that the patient’s CBG is 408 and the patient is really sleepy. You have an order for sliding scale insulin coverage but the order says to notify the MD for any blood glucose > 400. S- Dr. Sweeten, this is Aneva Taylor, Student nurse on the Med Surg unit. I am calling you about a 68 y.o. pt with a CBG of 408. The order says to notify the MD for any blood glucose > 400 B- 68 y.o. pt admitted with newly diagnosed Type II DM. The pt’s glucose level are currently > 400 A- The pt is really sleepy and blood glucose 408 R- The pt could benefit from a an increase in diabetic medication and a diabetic consultation as well