Low lever laser therapy (LLL) in chronic venous insufficiency
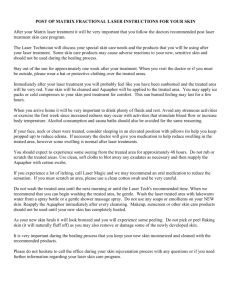
advertisement

LASER : PHOTO - BIOMODULATION Acta Chir Acad Sci Hung. 1976;17(1):49-55 Laser stimulation of wound healing Mester E, Nagylucskay S, Doklen A, Tisza S Serum complement activity, immunoglobulin levels and the circulatin auto-antibodies were studied in the course of laser treatment of 20 cases of crural ulcer. After temporary changes a normalization of the humoral immune response was observed in the healing cases, while in the stagnating ones opposite trend was manifest. In none of the groups were detected circulating auto-antibodies against the investigated antigens. Vestn Khir Im I I Grek. 1982 Dec;129(12):64-6 Use of laser irradiation in the treatment of trophic ulcers of the lower limbs Iupatov SI, Smotrin SM, Anufrik SS Results of the complex treatment of 65 patients with trophic ulcers of lower extremities resulting from chronic venous insufficiency with the use of laser irradiation of the ultraviolet range are reported. The laser irradiation was shown to exert a stimulating effect upon the regeneration of trophic ulcers. Its use was found to give considerably better results of the complex treatment. Vestn Khir Im I I Grek. 1984 Jan;132(1):69-71 Use of the helium-neon laser in the treatment of crural varicose ulcers Usik VS Results of the laser therapy of varicose ulcers of the crus in 45 patients were analyzed. The laser therapy is considered by the author to favourably influence the healing of the ulcers, to reduce pain, edema and skin hyperemia. Dermatologica. 1984;168(4):157-62 In vitro fibroblast and dermis fibroblast activation by laser irradiation at low energy. An electron microscopic study Bosatra M, Jucci A, Olliaro P, Quacci D, Sacchi S The effects of laser irradiations have been estimated both from the clinical point of view (rate of reduction of the ulcerated area) and in ultrastructural terms. The modification produced by laser in human fibroblasts in culture have also been investigated. Under our clinical and experimental conditions, laser stimulates the secretion of fibroblasts, both in vivo and in vitro, for reasons that are still the object of research. After irradiation the formation of periodic collagen fibrils is not observed, so that complete ' restitutio ad integrum' of the dermal matrix does not occur. Photodermatol. 1984 Oct;1(5):245-9 Inadequate effect of helium-neon laser on venous leg ulcers Santoianni P, Monfrecola G, Martellotta D, Ayala F A study to determine whether laser radiation of low-power photon density would really affect the healing of venous leg ulcers in man was performed. The ulcers were irradiated 6 d per wk with a helium-neon laser (wavelength 632.8 nm). Energy densities of 1 J/cm2 (16 patients) and 4 J/cm2 (17 patients) were administered daily. The control group (28 patients) received only antiseptic local compresses as treatment. No statistically significant difference between the laser-treated group and the control group was found. It was concluded that helium-neon laser radiation has no advantages over standard local treatments, at least with the dosage schedules and protocols employed. Vestn Khir Im I I Grek. 1985 Feb;134(2):55-8 Treatment of trophic ulcers and non-healing wounds with CO2 laser Koshelev VN, Glukhov EI, Barkhatov LN The authors used high and low intensity CO2 lasers for the treatment of 140 patients with trophic ulcers and continuously non-healing wounds. Choice of the method of treatment, parameters of laser radiation are based on concrete values of indices of the regeneration processes in the wounds and ulcers. In 83,6% of patients there was a complete recovery of the wounds, in 16,4% the recovery was partial. Health Phys 1989 May;56(5):691-704 Photobiology of low-power laser effects Karu T Quantitative studies have been performed to determine the action of low-intensity visible monochromatic light on various cells (E. coli, yeasts, HeLa, Chinese hamster fibroblasts and human lymphocytes); also irradiation conditions (wavelength, dose and intensity) conducive to vital activity stimulation have been examined. Respiratory chain components are discussed as primary photoacceptors. The possible ways for photosignal transduction and amplification are discussed. It is proposed that enhanced wound healing due to irradiation with low-intensity visible laser light (He-Cd, He-Ne and semiconductor lasers) is due to the increasing proliferation of cells. G Ital Dermatol Venereol. 1989 Jun;124(6):317-9 Defocused CO2 laser in the treatment of leg ulcers. Preliminary results Campolmi P, Lotti T, Bonan P, Tsampau D, Palleschi GM, Andreassi L We studied the therapeutic action of CO2 Laser on leg ulcers due to chronic venous hypertension in 30 subjects. Our findings show good results in reducing pain and leg oedema and wound healing. Ortop Travmatol Protez. 1989 Oct;(10):66-70 Experimental and clinical substantiation of laser therapy of wounds and trophic ulcers Rakcheev AP, Kiprenskii IuV The authors have studied the results of 120 experiments on 60 guinea-pigs and 110 rabbits who received the treatment of modelled fenestrated musculocutaneous wounds and trophic ulcers respectively on the replanted extremity and on the back with helium and neon laser until they healed completely. The authors have demonstrated that the laser therapy accelerates the process of reparative regeneration. In 50 intact rabbits who received local irradiation with helium and neon laser there was an increase in the activity of lysosome enzymes and in the protein metabolism values in the blood serum. The use of the helium and neon laser with the specific density of the irradiation rate of 2.5 mWt/cm2 and the exposition during 5 minutes in the treatment of trophic ulcers and persistent wounds in 56 patients as well as in 38 patients with consequences of injuries to the main blood vessels, the nerve trunks, the muscles and the tendons of the extremities before and after the reconstructive operations testifies to its high efficacy. Khirurgiia (Mosk). 1989 Sep;(9):97-9. Treatment of acute thrombophlebitis of the lower limbs with laser irradiation Dudenko GI, Zaliubovskii VI Low-intensity helium-neon laser (LG-75) radiation produces a marked analgesic, desensitizing, hypocoagulative, and immunostimulating effect, which can be used in the treatment of acute thrombophlebitis of the lower limbs. Laser therapy alters the phase course of the wound process and in this way improves microcirculation and oxygenation of the tissues, shortens the terms of wound healing, and may be used as the method of choice in the treatment of trophic ulcers of the lower limbs. Ann Vasc Surg 1990 Mar;4(2):179-81 The use of infrared laser therapy in the treatment of venous ulceration Sugrue ME, Carolan J, Leen EJ, Feeley TM, Moore DJ, Shanik GD Management of intractable venous ulceration remains an unrewarding task which is increasingly delegated to the realm of the vascular surgeon. The purpose of this pilot study was to assess the ulcer-healing effects of the newest form of biostimulation--the low power laser. Twelve patients with chronic venous ulcers unresponsive to conservative measures were treated with infrared laser irradiation for twelve weeks. Two ulcers healed completely and there was a 27% (p less than 0.01) reduction in size of the remaining ulcers. Treatment resulted in a 44% (p less than 0.01) increase in ulcer floor area occupied by healthy granulation tissue. The most dramatic effect of laser treatment was the reduction in ulcer pain, from 7.5 to 3.5 (linear analogue scale) (p less than 0.001). Laser irradiation had no effect on TcPO2, number of skin capillaries or pericapillary fibrin deposition in the lipodermatosclerotic area around the ulcer. The results of this pilot study are encouraging and a carefully controlled randomized study is indicated to compare low power laser irradiation to conventional treatment in the management of venous ulcers. Khirurgiia (Mosk) 1990 May;(5):105-8 Treatment of trophic ulcers of the lower extremities in elderly patients Iupatov SI, Smotrin SM, Gavcrilik BL, Sten'ko VG The article analyses the results of treatment of trophic ulcers of the lower extremities consequent upon chronic venous insufficiency in 199 elderly patients. Concomitant diseases were encountered in 82% of patients, which called for a differential approach to the choice of the method of treatment. Combined laser therapy in the system of complex treatment in 83 patients proved to be highly effective. Khirurgiia (Mosk) 1990 Dec;(12):93-6 Treatment of non-healing wounds and trophic ulcers by low- intensity laser irradiation in an outpatient clinic Georgadze AK, Karpov VI, Kuznetsov EV, Soldatov AV, Rukosuev VP Experience in treating 351 patients with persistent wounds and trophic ulcers by lowintensity laser radiation in out-patient clinics is generalized. Complete epithelialization of the wound or ulcer surface occurred in 236 patients. There were 246 patients aged 60, all were treated without leave from work. Thus, the inclusion of laser therapy in the complex of measures for persistent wounds and trophic ulcers is a highly effective method which may be applied in preoperative management and which will reduce considerably the term of in-patient treatment. Scand J Plast Reconstr Surg Hand Surg. 1991;25(3):249-51 Effect of low power gallium arsenide laser on healing of venous ulcers Malm M, Lundeberg T The healing of venous ulcers of the leg with and without gallium arsenide laser treatment was studied in 42 patients randomly divided into two groups. One group received standard conservative treatment and gallium arsenide laser, and the other received the same standard treatment and placebo laser treatment. There were no differences in results between the two groups. Ann Plast Surg. 1991 Dec;27(6):537-9 Low-power HeNe laser treatment of venous leg ulcers Lundeberg T, Malm M Clinical observations have suggested that low-energy lasers, mainly helium-neon (HeNe) lasers, might stimulate wound healing. A controlled study of the effects of low-power HeNe laser was performed in conjunction with a standard treatment for healing chronic venous leg ulcers on 46 patients divided randomly into two groups. All patients received standard treatment (paste-impregnated bandage and a self-adhesive elastic bandage) plus either HeNe laser (wave-length, 632.8 nm; beam power, 6 mW; continuous emission, energy density, 4 J/cm2) or placebo HeNe laser twice weekly for 12 weeks. The areas of healing were examined and compared percentage-wise after 2, 4, 6, 8, and 12 weeks. There were no significant differences in the proportion of healed ulcers or ulcer area in the HeNe group compared with the placebo group. Klin Khir. 1992;(3):47-9 The use of helium-neon laser radiation in the treatment of trophic disorders in patients with diabetes mellitus Zubkova ST The effectiveness of laser therapy in trophic skin disorders (ulcer, diabetic bulla, hematoma, skin chap) in patients with diabetes mellitus was studied. The foci of trophic disorders and biologically active points were irradiated by means of heliumneon laser installations. The technique was employed in a hospital and in out-patient treatment in the complex with medicamentous therapy and without that in patients resistant to medicamentous therapy. A high effectiveness of laser therapy has been established. Clin Podiatr Med Surg. 1992 Jul;9(3):709-19 The efficacy of carbon dioxide laser surgery for adjunct ulcer therapy Chromey PA This article focuses on the application of the carbon dioxide (CO2) laser at various levels of power density to achieve a level of efficacy in tissue ablation for cutaneous and deep indolent ulcerations that afflict the lower extremities. This article also supports theories of the CO2 laser generating a sterile nonpathogenic environment within ulcers. A cross section of various ulcer types are used to determine duration of healing. Khirurgiia (Mosk). 1992 Jul-Aug;(7-8):30-3 Treatment of suppurative wounds in patients with diabetes mellitus by magnetic field and laser irradiation Kuliev RA, Babaev RF, Akhmedova LM, Ragimova AI The efficacy of including a magnetic field, low-intensity laser beam, and their combination in the complex of therapeutic measures was studied in 119 patients with suppurative wounds and diabetes mellitus. With the use of magnetic field or laser beam intoxication diminished, the organism's immunological status was stabilized within a shorter time, the wound process followed a quicker course, and treatment took less time. The magnetic-laser effect has advantages over separate use of these factors. Biomed Tech (Berl) 1993 Jul-Aug;38(7-8):168-71 LILAB, a new system for superficial application of low intensity laser beams in medicine Sommer A, Franke RP Laser energy densities between 1 and 4 J/cm2 evoked a significant biostimulation in human tissues. Lower energy densities had no apparent effect, but higher energy densities resulted in cell damage. In principle, low energy densities can be applied with high-energy lasers in combination with laser beam diverging lenses, or with low-power lasers in combination with scanning devices. High-energy lasers are undesirable because of their high cost. Low-energy lasers in combination with conventional scanners also suffer from high cost, and these scanners have another major disadvantage: the energy density at the edge of the application field may be up to five times as great as in the center. A new laser beam distribution system for medical applications is introduced here. Because of its moderate price it is well-suited for use with low-energy lasers. Any desired geometrical shape of the application field is easily created, and with a homogeneous energy density. Phys Ther. 1994 Sep;74(9):812-23; discussion 824-5 Comparison of ultrasound/ultraviolet-C and laser for treatment of pressure ulcersin patients with spinal cord injury Nussbaum EL, Biemann I, Mustard B Background And Purpose: The purpose of this study was to compare in patients withspinal cord injury the effect on wound healing of nursing care alone with the effect on wound healing of nursing care combined with either laser treatment or a regimen of ultrasound and ultraviolet-C (US/UVC). Subjects: Twenty patients (22 wounds) were randomly assigned to the treatment groups. Methods: All patients received standard wound care consisting of wound cleaning twice daily, application of moist dressings, and continuous relief of pressure until the wounds were healed. The laser protocol consisted of three treatments weekly using a cluster probe with an 820-nm laser diode and 30 superluminous diodes (10 each at 660, 880, and 950 nm), and energy density of 4J/cm2, and a pulse repetition rate of 5,000 pulses per second. The US/UVC regimen consisted of five treatments weekly, alternating the treatment modality daily. The pulsed US was applied at a frequency of 3 MHz and a spatial average-temporal average intensity of 0.2 W/cm2 (1:4 pulse ratio) for 5 minutes per 5 cm2 of wound area. The UVC dosage (95% emission at 250 nm) was calculated each session according to wound appearance. The dosage level was E1 for clean/granulating areas, E3 for purulent/slow-granulating areas, E4 for heavily infected areas, and 2E4 for wound debridement. Wounds were traced every 14 days, and surface areas were calculated using the Sigma-Scan Measurement System. Weekly percentage changes in wound area were compared. Results: Results showed that US/UVC treatment had a greater effect on wound healing than did nursing care, either alone or combined with laser. Conclusion And Discussion: Ultrasound/ultraviolet-C may decrease healing time and may allow faster return to rehabilitation programs, work, and leisure activities for patients with spinal cord injury who have pressure ulcers. Am J Phys Med Rehabil. 1997 Jul-Aug;76(4):288-96. Combined ultrasound, electrical stimulation, and laser promote collagen synthesis with moderate changes in tendon biomechanics Gum SL, Reddy GK, Stehno-Bittel L, Enwemeka CS The biomechanical, biochemical, and ultrastructural effects of a multitherapeutic protocol were studied using regenerating rabbit Achilles tendons. The multitherapeutic protocol was composed of low-intensity Ga:As laser photostimulation, low intensity ultrasound, and electrical stimulation. Achilles tendons of 63 male New Zealand rabbits were tenotomized, sutured, immobilized, and subjected to the multitherapeutic protocol for five days, after which casts were removed and the therapy was continued for nine more days without electrical stimulation. The tendons were excised and compared with control tendons. Multitherapy treatment produced a 14% increase in maximal strength, a 42% increase in load-at-break, a 20% increase in maximal stress, a 45% increase in stressat-break, a 21% increase in maximal strain, and a 14% increase in strain-at-break. Similarly, multitherapy treatment was associated with an increase in Young's modulus of elasticity of 31%, an increase in energy absorption at maximum load of 9%, and an increase in energy absorption at load-at-break of 11%. Biochemical analysis of the tendons showed an increase of 23% in the total amount of collagen in the multitherapytreated tendons, with fewer mature crosslinks (decrease of 6%). Electron micrographs revealed no ultrastructural or morphologic changes in the tendon fibroblasts or in the extracellular matrix. The improvements measured in tendons receiving multitherapy were consistent but less remarkable compared with our earlier works with single modality protocols. The results warrant the hypothesis that the beneficial effects of ultrasound and laser photostimulation on tendon healing may counteract one another when applied simultaneously. Lasers Surg Med. 1998;22(5):281-7. Laser photostimulation of collagen production in healing rabbit Achilles tendons Reddy GK, Stehno-Bittel L, Enwemeka CS Background And Objective: Low energy laser photostimulation at certain wavelengths can enhance tissue repair by releasing growth factors from fibroblasts and stimulate the healing process. This study was designed to evaluate the influence of laser photostimulation on collagen production in experimentally tenotomized and repaired rabbit Achilles tendons. Study Design/Materials And Methods: A total of 24 male New Zealand rabbits, ages 10-12weeks, were used. Following tenotomy and repair, the surgical hind limbs of therabbits were immobilized in customized polyurethane casts. The experimental animals were treated with a 632.8 nm He:Ne laser daily at 1.0 J cm(-2) for 14 days. Control animals were sham treated with the laser head. On the fifth day after repair, the casts were removed to allow the animals to bear weight on the lower extremity. The animals were euthanized on the 15th postoperative day, then, the Achilles tendons were excised, processed and analyzed. RESULTS: Biochemical analyses of the tendons revealed a 26% increase in collagen concentration with laser photostimulation indicating a more rapid healing process in treated tendons compared to controls. Sequential extractions of collagen from regenerating tissues revealed that the laser photostimulated tendons had 32% and 33% greater concentrations of neutral salt soluble collagen and insoluble collagen, respectively, than control tendons suggesting an accelerated production of collagen with laser photostimulation. A significant decrease (9%) in pepsin soluble collagen was observed in laser-treated tendons compared to controls. There were no statistically significant differences recorded in the concentrations of hydroxypyridinium crosslinks and acid soluble collagen between treated and control tendons. Conclusion: This study of laser photostimulation on tendon healing in rabbits suggests that such therapy facilitates collagen production in a manner that enhances tendon healing. Diabetes Care. 1998 Apr;21(4):580-4 Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy Schindl A, Schindl M, Schon H, Knobler R, Havelec L, Schindl L Objective: Diabetic foot problems due to angiopathy and neuropathy account for 50% of all nontraumatic amputations and constitute a significant economic burden to society. Low-intensity laser irradiation has been shown to induce wound healing in conditions of reduced microcirculation. We investigated the influence of low-intensity laser irradiation by means of infrared thermography on skin blood circulation in diabetic patients with diabetic microangiopathy. Research design And Methods: Thirty consecutive patients with diabetic ulcers or gangrenes and elevated levels of glycosylated hemoglobin were randomized by blocks of two to receive either a single low-intensity laser irradiation with an energy density of 30 J/cm2 or a sham irradiation over both forefoot regions in a double-blind placebocontrolled clinical study. Skin blood circulation as indicated by temperature recordings over the forefoot region was detected by infrared thermography. Results: After a single transcutaneous low-intensity laser irradiation, a statistically significant rise in skin temperature was noted (P < 0.001 by ANOVA for repeated measurements), whereas in the sham-irradiated control group, a slight but significant drop in temperature (P < 0.001) was found. Subsequently performed contrasts for comparison of measurements before and after irradiation revealed significant temperature increases at 20 min of irradiation time (P < 0.001), at the end of the irradiation (P < 0.001), and 15 min after stopping the irradiation (P < 0.001). In the sham-irradiated feet, the drop in local skin temperature was not significant at 20 min (P = 0.1), but reached significance at the end of the sham-irradiation procedure (P < 0.001) and 15 min after the end of sham irradiation (P < 0.001). Conclusions: The data from this first randomized double-blind placebo-controlled clinical trial demonstrate an increase in skin microcirculation due to athermic laser irradiation in patients with diabetic microangiopathy. Lasers Surg Med 1998;22(5):294-301 Stimulatory effect of 660 nm low level laser energy on hypertrophic scarderived fibroblasts: possible mechanisms for increase in cell counts Webb C, Dyson M, Lewis WH Background And Objective: Varying effects of red light wavelengths on in vitro cells have been reported. Low level lasers (LLL) are employed to assist wound healing especially for indolent ulcers. On healing, burn wounds may become hypertrophic, resulting in excessive wound contraction, poor cosmesis, and functional impairment. This study enquired whether 660 nm LLL affected hypertrophic scar-derived fibroblasts. Study Design/Materials And Methods: The experiments investigated the effect of a 660 nm, 17 mW laser diode at dosages of 2.4 J/cm2 and 4 J/cm2 on cell counts of two human fibroblast cell lines, derived from hypertrophic scar tissue (HSF) and normal dermal (NDF) tissue explants, respectively. The protocol avoided transfer of postirradiated cells. Estimation of fibroblasts utilized the methylene blue bioassay. Results/Conclusion: Thepost-660 nm-irradiated HSFs exhibited very significantly higher cell counts thancontrols P < 0.01 on days 1-4 (Mann-Whitney U-test), and P < 0.01 on days 1-3 for similarly irradiated NDFs. Khirurgiia (Mosk) 1998;(4):42-5 Combined therapy of trophic ulcers with protracted healing Babadzhanov BR, Sultanov IA The results of treatment of 126 patients with trophic ulcers of the low extremities were analyzed. Trophic ulcers in 74 patients (58.7%) appeared due to postthrombophlebitic disease, in 25 patients (19.8%) due to primary varicose veins of lower limbs, in 15 (11.9%) patients due to obliterative diseases of peripheral vessels and in 12 (9.5%)-other diseases. The duration of the illness made up from 1 to 50 years. In 26 patients (group 1) low-intensity laser irradiation (LLI) was used together with combined conservative therapy; in 32 patients (group 2) hyperbaric oxygenation (HBO), in 21 (3 group)—combined application of LLI and HBO was used. The examination of regional macrohemodynamics and microcirculation in 39 patients showed decrease of rheographic index (RI) in the shin, increase of the arterioles tone and venous outflow disturbance. The use of LLI and HBO resulted in undoubtful increase of RI and improvement of microcirculatory indexes. As a result of combined application of LLI and HBO microflora of the ulcers lowered from 10 and 10 per 1 gr in patients of group 1 and 2, respectively, in patients of group 3 there was no growth of pathogenic microflora. The investigation of humoral and cellular immunity after the application of LLI and HBO demonstrated strong immunocorrective action. Arch Orthop Trauma Surg. 1998;117(3):156-8 Topical hyperbaric oxygen and low energy laser for the treatment of diabetic foot ulcers Landau Z Fifty patients with chronic diabetic foot ulcers in whom conventional therapy had failed were treated with topical hyperbaric oxygen alone (15 patients) or in combination with a low energy laser (35 patients). Eleven of these patients were treated on an ambulatory basis with topical hyperbaric oxygen. The mean time the ulcer was present before therapy was 9+/-6.6 months. The mean number of treatments was 25+/-13, and the mean duration of therapy was 3+/-1.8 months. Forty-three of the 50 patients were cured. No adverse reactions were noted. Our impression is that topical hyperbaric oxygen alone or in combination with a low power laser are valuable adjuvants to conventional therapy for diabetic foot ulcers. J Clin Laser Med Surg 1999 Feb;17(1):29-33 Low power laser therapy and analgesic action Tam G Objective: The semiconductor or laser diode (GaAs, 904 nm) is the most appropriate choice in pain reduction therapy. Summary Background Data: Low-powerdensity laser acts on the prostaglandin (PG) synthesis, increasing the change ofn PGG2 and PGH2 into PG12 (also called prostacyclin, or epoprostenol). The last is the main product of the arachidonic acid into the endothelial cells and into the smooth muscular cells of vessel walls, that have a vasodilating and anti-inflammatory action. Methods: Treatment was performed on 372 patients (206 women and 166 men) during the period between May 1987 and January 1997. The patients, whose ages ranged from 25 to 70 years, with a mean age of 45 years, suffered from rheumatic, degenerative, and traumatic pathologies as well as cutaneous ulcers. The majority of patients had been seen by orthopedists and rheumatologists and had undergone x-ray examination. All patients had received drug-based treatment and/or physiotherapy with poor results; 5 patients had also been irradiated with He:Ne and CO2 lasers. Two-thirds were experiencing acute symptomatic pain, while the others suffered long-term pathology with recurrent crises. We used a pulsed diode laser, GaAs 904 nm wavelength once per day for 5 consecutive days, followed by a 2-day interval. The average number of applications was 12. We irradiated the trigger points, access points to the joint, and striated muscles adjacent to relevant nerve roots. RESULTS: We achieved very good results, especially in cases of symptomatic osteoarthritis of the cervical vertebrae, sport-related injuries, epicondylitis, and cutaneous ulcers, and with cases of osteoarthritis of the coxa. Conclusions: Treatment with 904-nm diode laser has substantially reduced the symptoms as well as improved the quality of life of these patient, ultimately postponing the need for surgery. J Wound Care 1999 Mar;8(3):111-4 A systematic review of laser therapy for venous leg ulcers Flemming KA, Cullum NA, Nelson EA A systematic review of randomised controlled trials (RCTs) was conducted to establish the effectiveness of low-level laser therapy as a treatment for venous leg ulcers. Woundcare journals, conference proceedings and electronic databases (including Medline and Cinahl) were searched up to October 1997 for RCTs comparing low-level laser therapy with sham laser, no laser, or non-coherent light of other wavelengths. In addition, companies who manufacture or distribute therapeutic lasers were contacted for any unpublished or ongoing studies. Results from searches were scrutinised by one reviewer to identify possible RCTs and full reports of these were obtained. Details of eligible studies were extracted and summarised using a data extraction sheet. Data extraction was checked by a second reviewer. Meta-analysis was used to combine the results of trials where the interventions and outcome measures were sufficiently similar. A total of four eligible RCTs were identified. Two compared treatment with laser therapy to sham or placebo laser treatment. One study compared laser therapy with ultraviolet therapy. The fourth was a three-armed study which compared the effects of laser therapy alone, laser therapy plus infrared light, and non-coherent unpolarised red light. The comparisons of laser therapy with placebo, and laser therapy with ultraviolet therapy, showed no significant difference between treatments with regard to ulcer healing rates. The comparison of laser with red light showed a significant increase in complete healing at nine months for the combination of laser and infrared light compared to non-coherent unpolarised red light. We have not found any evidence of the benefit of low-level laser therapy per se on venous leg ulcer healing. It appears that a combination of HeNe laser and infrared light may promote the healing of venous ulcers, however more research is needed. Nurs Stand 1999 Oct 6-12;14(3):66-70, 72 Low intensity laser therapy for chronic venous leg ulcers Ashford R, Lagan K, Brown N, Howell C, Nolan C, Brady D, Walsh M Ulceration of the lower extremities is one of the most important medicosocial problems (Skobelkin et al 1990). In this article, two case studies show that it is the length of time that laser therapy is used that can have a significant impact on ulcer size. Dermatology. 1999;198(3):314-6 Diabetic neuropathic foot ulcer: successful treatment by low-intensity laser therapy Schindl A, Schindl M, Pernerstorfer-Schon H, Kerschan K, Knobler R, Schindl L Objective: To evaluate the efficacy of low-intensity laser irradiation for the induction of wound healing of a diabetic neuropathic foot ulcer. Case: We report a case of a man with insulin-dependent diabetes mellitus, sensory neuropathy, macroangiopathy and microangiopathy who had been suffering from an ulcer of his first left toe accompanied by osteomyelitis for 6 weeks. Results: After a total of 16 sessions of low-intensity laser therapy using a 670-nm diode laser administered within a 4-week period the ulcer healed completely. During a followup period of 9 months, there was no recurrence of the ulcer even though the patient's metabolic condition remained unstable. Conclusions: Although laser therapy was not applied as a monotherapy, the present observation suggests that it might constitute a useful side-effect-free alternative treatment modality for the induction of wound healing of neuropathic ulcers in diabetic patients. Therefore large properly controlled randomized studies seem justified. J Photochem Photobiol B 2000 Jan;54(1):55-60 Effects of 780 nm diode laser irradiation on blood microcirculation: preliminary findings on time-dependent T1-weighted contrast-enhanced magnetic resonance imaging (MRI) Schaffer M, Bonel H, Sroka R, Schaffer PM, Busch M, Reiser M, Duhmke E Laser therapy by low light doses shows promising results in the modulation of some cell functions. Various clinical studies indicate that laser therapy is a valuable method for pain treatment and the acceleration of wound healing. However, the mechanism behind it is still not completely understood. To explore the effect of a low-power diode laser (lambda = 780 nm) on normal skin tissue, time-dependent contrast enhancement has been determined by magnetic resonance imaging (MRI). In the examinations, six healthy volunteers (four male and two female) have been irradiated on their right planta pedis (sole of foot) with 5 J/cm2 at a fluence rate of 100 mW/cm2. T1-weighted magnetic resonance imaging is used to quantify the time-dependent local accumulation of Gadolinium-DPTA, its actual content in the local current blood volume as well as its distribution to the extracellular space. Images are obtained before and after the application of laser light. When laser light is applied the signal to noise ratio increases by more than 0.35 +/- 0.15 (range 0.23-0.63) after irradiation according to contrastenhanced MRI. It can be observed that, after biomodulation with light of low energy and low power, wound healing improves and pain is reduced. This effect might be explained by an increased blood flow in this area. Therefore, the use of this kind of laser treatment might improve the outcome of other therapeutic modalities such as tumour ionizing radiation therapy and local chemotherapy. J Clin Laser Med Surg 2000 Feb;18(1):15-22 A case report of low intensity laser therapy (LILT) in the management of venous ulceration: potential effects of wound debridement upon efficacy Lagan KM, Mc Donough SM, Clements BA, Baxter GD Objective: This single case report (ABA design) was undertaken as a preliminary investigation into the clinical effects of low intensity laser upon venous ulceration, applied to wound margins only, and the potential relevance of wound debridement and wound measurement techniques to any effects observed. Methods: Ethical approval was granted by the University of Ulster's Research Ethical Committee and the patient recruited was required to attend 3 times per week for a total of 8 weeks. Treatments were carried out using single source irradiation (830 nm; 9 J/cm2, CB Medico, Copenhagen, Denmark) in conjunction with dry dressings during each visit. Assessment of wound surface area, wound appearance, and current pain were completed by an independent investigator. Planimetry and digitizing were completed for wound tracings and for photographs to quantify surface areas. Video image analysis was also performed on photographs of wounds. Results: The primary findings were changes in wound appearance, and a decrease in wound surface area (range 33.3-46.3%), dependent on the choice of measurement method. Video image analysis was used, but rejected as an accurate method of wound measurement. Treatment intervention produced a statistically significant reduction in wound area using the C statistic on digitizing data for photographs (at Phase one only; Z = 2.412; p < 0.05). Wound debridement emerged as an important procedure to be carried out prior to measuring wounds. Despite fluctuating pain levels recorded throughout the duration of the study, VAS scores showed a decrease of 15% at the end of the study. This hypoalgesic effect was, however, statistically significant (using the C statistic) at Phase one only (Z = 2.554; p < 0.05). Conclusions: Low intensity laser therapy at this dosage, and using single source irradiation would seem to be an effective treatment for patients suffering venous ulceration. Further group studies are indicated to establish the most effective therapeutic dosage for this and other types of ulceration. Cochrane Database Syst Rev. 2000;(2):CD001182 Laser therapy for venous leg ulcers Flemming K, Cullum N Objectives: To assess the effectiveness of low level laser therapy in the treatment of venous leg ulcers. Search Strategy: Searches of 19 databases, hand searching of journals and conference proceedings from 1948 onwards, and examination of bibliographies. Selection Criteria: Randomised controlled trials comparing low level laser therapy with: sham laser; no laser; non-coherent light. There was no restriction on date or language. The main outcome measure used was complete healing of the ulcers. Data Collection And Analysis: Dataextraction was done by one reviewer and checked by a second. Meta analysis wasused to combine the results of trials where the interventions and outcomemeasures were sufficiently similar. MAIN RESULTS: There were 4 eligible trials.Two RCTs compared laser therapy with sham, 1 with ultraviolet therapy and 1 withnon-coherent, unpolarised red light. Neither of the two RCTs comparing laserwith sham found a significant difference in healing rates; there was no significant of laser evident when the trials were pooled. A three-arm study compared: laser therapy alone - laser therapy plus infrared light - non-coherent, unpolarised red light. Significantly more ulcers completely healed in the group receiving a combination of laser and infrared light compared with non-coherent, unpolarised red light. A fourth trial compared laser and ultraviolet light and found no difference. Reviewer's Conclusions: We have found no evidence of any benefit associated with low level laser therapy on venous leg ulcer healing. One small study suggests that a combination of laser and infrared light may promote the healing of venous ulcers, however more research is needed. J Clin Laser Med Surg 2000 Oct;18(5):235-40 Low-level laser therapy for wound healing: feasibility of wound dressing transillumination Lilge L, Tierney K, Nussbaum E Objective: The purpose of this study was to assess the feasibility of exposing wounds during low-level laser therapy (LLLT) by transillumination of the wound dressings. Background Data: LLLT has been associated with accelerated wound healing in chronic ulcers. The usual approach is to remove wound dressings prior to exposure and to treat three to five times weekly. Frequent change of wound dressings is time consuming and costly; it disrupts the healing process, increases the risk of wound infection, and may be traumatic for the patient. Methods: A double integrating sphere setup was employed to quantify the diffuse transmittance and reflectance of various wound dressings. Differences in transmittance for large area sources and point sources were demonstrated through the use of a diode laser and an incoherent light source. RESULTS: There were a number of gels and membrane style wound dressings with diffuse transmittance of more than 50%. Hence, for these dressings the prescribed radiant exposure to the wound surface could be achieved by increasing the exposure duration, while maintaining reasonable overall treatment times. Conclusions: Although LLLT by transillumination of wound dressings is feasible for a variety of wound dressings without significant commitments in additional treatment time, the specific transmission of products not included in this study needs to be determined at the intended treatment wavelength. A transillumination approach may facilitate a faster rate of wound healing than LLLT applied to exposed wounds by reducing trauma and the risk of infection. J Photochem Photobiol B 2000 Dec;59(1-3):1-8 Magnetic resonance imaging (MRI) controlled outcome of side effects caused by ionizing radiation, treated with 780 nm-diode laser -- preliminary results Schaffer M, Bonel H, Sroka R, Schaffer PM, Busch M, Sittek H, Reiser M, Duhmke E Background And Objective: Ionizing radiation therapy by way of various beams such as electron, photon and neutron is an established method in tumor treatment. The side effects caused by this treatment such as ulcer, painful mastitis and delay of wound healing are well known, too. Biomodulation by low level laser therapy (LLLT) has become popular as a therapeutic modality for the acceleration of wound healing and the treatment of inflammation. Evidence for this kind of application, however, is not fully understood yet. This study intends to demonstrate the response of biomodulative laser treatment on the side effects caused by ionizing radiation by means of magnetic resonance imaging (MRI). Study Design/Patients And Methods: Six female patients suffering from painful mastitis after breast ionizing irradiation and one man suffering from radiogenic ulcer were treated with lambda=780 nm diode laser irradiation at a fluence rate of 5 J/cm2. LLLT was performed for a period of 4-6 weeks (mean sessions: 25 per patient, range 19 35). The tissue response was determined by means of MRI after laser treatment in comparison to MRI prior to the beginning of the LLLT. Results: All patients showed complete clinical remission. The time-dependent contrast enhancement curve obtained by the evaluation of MR images demonstrated a significant decrease of enhancement features typical for inflammation in the affected area. Conclusion: Biomodulation by LLLT seems to be a promising treatment modality for side effects induced by ionizing radiation. J Clin Laser Med Surg 2000 Apr;18(2):67-73 Wound healing of animal and human body sport and traffic accident injuries using low-level laser therapy treatment: a randomized clinical study of seventyfour patients with control group Simunovic Z, Ivankovich AD, Depolo A Background And Objective: The main objective of current animal and clinical studies was to assess the efficacy of low level laser therapy (LLLT) on wound healing in rabbits and humans. Study Design/Materials And Methods: In the initial part of our research we conducted a randomized controlled animal study, where we evaluated the effects of laser irradiation on the healing of surgical wounds on rabbits. The manner of the application of LLLT on the human body are analogous to those of similar physiologic structure in animal tissue, therefore, this study was continued on humans. Clinical study was performed on 74 patients with injuries to the following anatomic locations: ankle and knee, bilaterally, Achilles tendon; epicondylus; shoulder; wrist; interphalangeal joints of hands, unilaterally. All patients had had surgical procedure prior to LLLT. Two types of laser devices were used: infrared diode laser (GaAlAs) 830 nm continuous wave for treatment of trigger points (TPs) and HeNe 632.8 nm combined with diode laser 904-nm pulsed wave for scanning procedure. Both were applied as monotherapy during current clinical study. The results were observed and measured according to the following clinical parameters: redness, heat, pain, swelling and loss of function, and finally postponed to statistical analysis via chi2 test. Results: After comparing the healing process between two groups of patients, we obtained the following results: wound healing was significantly accelerated (25%-35%) in the group of patients treated with LLLT. Pain relief and functional recovery of patients treated with LLLT were significantly improved comparing to untreated patients. Conclusion: In addition to accelerated wound healing, the main advantages of LLLT for postoperative sport- and traffic-related injuries include prevention of side effects of drugs, significantly accelerated functional recovery, earlier return to work, training and sport competition compared to the control group of patients, and cost benefit. Yale J Biol Med. 2001 Mar-Apr;74(2):95-100 Topical hyperbaric oxygen and low energy laser therapy for chronic diabetic foot ulcers resistant to conventional treatment Landau Z, Schattner A Chronic foot ulcers are common in long-standing diabetes, may herald severe complications and are often resistant to therapy. To evaluate the effects of adjunctive topical hyperbaric oxygen treatment (THBO) and low energy laser (LEL) irradiation on ulcer healing, a 100 consecutive patients with chronic diabetic foot ulcers (DFU) refractory to 4.5 +/- 1.2 months of comprehensive treatment, were enrolled in a prospective open study. While conventional treatment was continued as necessary, THBO was administered by pumping 100 percent oxygen into a disposable sealed polythylene hyperbaric chamber (150 min x 2 to 3/wk at up to 1.04 atm). Helium-neon LEL irradiation was given concurrently using a Unilaser Scan Unit at 4 J/cm2 for 20 min. Some patients continued THBO at home or their treatment was confined to THBO at home. Patients were monitored every two weeks revealing 81 percent cure after 25 +/13 treatments over 3.2 +/- 1.7 months. On follow-up (median 18 months), only 3/81 (4 percent) had reulceration, which responded to THBO/LEL retreatment. Nonresponders had significantly lower ankle brachial indices (ABI) than patients whose ulcers were healed (0.55 vs. 0.78, p < 0.01) and ultimately required amputation. Patient compliance was full and no adverse events occurred. In conclusion, although the study was open and uncontrolled, an 81 percent healing of DFU in patients who previously did not respond to a comprehensive treatment program, constitutes an intriguing preliminary result. Thus, THBO/LEL therapy may be a safe, simple, and inexpensive early adjunctive treatment for patients with chronic diabetic foot ulcers. Our findings should prompt its evaluation by large randomized controlled trials. Health Technol Assess. 2001;5(9):1-221 Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy Cullum N, Nelson EA, Flemming K, Sheldon T Background: Chronic wounds such as leg ulcers, diabetic foot ulcers and pressure sores are common in both acute and community healthcare settings. The prevention and treatment of these wounds involves many strategies: pressure-relieving beds, mattresses and cushions are universally used as measures for the prevention and treatment of pressure sores; compression therapy in a variety of forms is widely used for venous leg ulcer prevention and treatment; and a whole range of therapies involving laser, ultrasound and electricity is also applied to chronic wounds. This report covers the final three reviews from a series of seven. AIMS: To assess the clinical effectiveness and costeffectiveness of: (1) pressure-relieving beds, mattresses and cushions for pressure sore prevention and treatment; (2) compression therapy for the prevention and treatment of leg ulcers; (3) low-level laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy for the treatment of chronic wounds. Methods - Data Sources: Nineteen electronic databases, including MEDLINE, CINAHL, EMBASE and the Cochrane Controlled Trials Register (CENTRAL), were searched. Relevant journals, conference proceedings and bibliographies of retrieved papers were handsearched. An expert panel was also consulted. METHODS - STUDY SELECTION: Randomised controlled trials (RCTs) which evaluated these interventions were eligible for inclusion in this review if they used objective measures of outcome such as wound incidence or healing rates. Results - Beds, Mattresses And Cushions For Pressure Sore Prevention And Treatment: A total of 45 RCTs were identified, of which 40 compared different mattresses, mattress overlays and beds. Only two trials evaluated cushions, one evaluated the use of sheepskins, and two looked at turning beds/kinetic therapy. Results - Compression For Leg Ulcers: A total of 24 trials reporting 26 comparisons were included (two of prevention and 24 of treatment strategies). Results - Low-Level Laser Therapy, Therapeutic Ultrasound, Electrotherapy And Electromagnetic Therapy: Four RCTs of laser (for venous leg ulcers), 10 of therapeutic ultrasound (for pressure sores and venous leg ulcers), 12 of electrotherapy (for ischaemic and diabetic ulcers, and chronic wounds generally) and five of electromagnetic therapy (for venous leg ulcers and pressure sores) were included. Studies were generally small, and of poor methodological quality. CONCLUSIONS (1) Foam alternatives to the standard hospital foam mattress can reduce the incidence of pressure sores in people at risk, as can pressure-relieving overlays on the operating table. One study suggests that air-fluidised therapy may increase pressure sore healing rates. (2) Compression is more effective in healing venous leg ulcers than is no compression, and multi-layered high compression is more effective than single-layer compression. High-compression hosiery was more effective than moderate compression in preventing ulcer recurrence. (3) There is generally insufficient reliable evidence to draw conclusions about the contribution of laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy to chronic wound healing. Wound Repair Regen. 2001 May-Jun;9(3):248-55. Laser photostimulation accelerates wound healing in diabetic rats Reddy GK, Stehno-Bittel L, Enwemeka CS In this study, we examined the hypothesis that laser photostimulation can facilitate healing of impaired wounds in experimental diabetes using a rat model. Diabetes was induced in male rats by streptozotocin injection and two 6 mm diameter circular wounds were created on either side of the spine. The left wound of each animal was treated with a 632.8 nm He:Ne laser at a dose of 1.0 J/cm2 for five days a week until the wounds closed (three weeks). Measurements of the biomechanical properties of the laser-treated wounds indicated there was a marginal increase in maximum load (16%), stress (16%), strain (27%), energy absorption (47%) and toughness (84%) compared to control wounds of diabetic rats. Biochemical assays revealed that the amount of total collagen was significantly increased in laser treated wounds (274 +/- 8.7 microg) over the control wounds (230 +/- 8.4 microg). Sequential extractions of collagen from healing wounds showed that laser treated wounds had significantly greater concentrations of neutral salt soluble (15%) and insoluble collagen (16%) than control wounds, suggesting accelerated collagen production in laser treated wounds. There was an appreciable decrease in pepsin soluble collagen (19%) in laser treated wounds over control wounds, indicating higher resistance to proteolytic digestion. In conclusion, the biomechanical and biochemical results collectively suggest that laser photostimulation promotes the tissue repair process by accelerating collagen production and promoting overall connective tissue stability in healing wounds of diabetic rats. Lasers Surg Med. 2001;29(2):105-6. 780 nm low power diode laser irradiation stimulates proliferation of keratinocyte cultures: involvement of reactive oxygen species Grossman N, Schneid N, Reuveni H, Halevy S, Lubart R Background And Objective: The purpose of this study was to determine irradiation parameters of a 780 nm low power CW diode laser (6.5 mW) leading to enhanced proliferation of cultured normal human keratinocytes (NHK). The possible role of reactive oxygen species (ROS) in this response was evaluated. Study Design/Materials And Methods: NHK were exposed to a single dose of 0 to 3.6 J/cm2 (0-180 sec) of irradiation. Proliferation parameters studied were: incorporation of 3H-thymidine during 6-24 hr following irradiation; percentage of dividing cells and number of cells, 24 hr and 48 hr following irradiation, respectively. Results: Proliferation of NHK exposed to 0.45-0.95 J/cm2 was significantly enhanced by 1.3-1.9-folds relative to sham-irradiated controls, as inferred from parameters studied. Exposure to other energy densities was considerably less effective in enhancing proliferation parameters. Added enzymatic antioxidants, superoxide dismutase or catalase, scavenging superoxide anions and H2O2, suppressed this enhanced proliferation. Added scavengers (alpha-tocopherol acetate, scavenging lipid peroxidation, or sodium azide, histidine, mannitol, scavenging singlet oxygen, superoxide anions, and hydroxyl radicals, respectively), or N-acetyl cysteine, the thiol-reducing agent, suppressed the response, but to different extents. Conclusions: The results indicate that 780 nm low power diode laser irradiation enhanced keratinocytes proliferation in vitro, with an apparent involvement of ROS in this response, and comparably, might be used to promote their proliferation in vivo to enhance wound healing. Lasers Surg Med 2001;28(1):27-32 Low intensity laser therapy (830nm) in the management of minor postsurgical wounds: a controlled clinical study Lagan KM, Clements BA, McDonough S, Baxter GD Background And Objective: The stimulatory effects of low intensity laser therapy (LILT) have been widely published for the treatment of chronic ulceration. In contrast to this previous work, the current study investigated its potential efficacy (by using a dosage of 9 J/cm2) in the management of acute wounds. For this purpose, uncomplicated postoperative wounds after minor podiatric surgery were examined. Study Design/Materials And Methods: The study was designed as a controlled group study. Ethical approval was granted by the University of Ulster's Research Ethics Committee. Patients (n = 9) presenting with a total of 12 wounds after minor surgical procedures (partial/total nail avulsions/electrosurgery) were recruited from the Podiatry Teaching Clinic, Northern Ireland. Patients attended the clinic once per week for assessment and treatment. Weekly irradiation was performed by using a CBM Master 3 (CB Medico, Copenhagen, Denmark) diode laser (GaAlAs). The physical parameters of the output of this unit were as follows: wavelength, 830 nm; average power output, 30 mW; spot size, 0.1 cm2; irradiance, 300 mW/cm2; continuous wave output. Wound assessment and recording of pain levels were conducted weekly. Wound measurement was completed by using planimetry and digitising methods. RESULTS: Current findings indicated no statistically significant differences between Laser and Control groups for wound closure (P = 0.28 digitising; P = 0.49 planimetry) nor for pain levels reported (P = 0.88). CONCLUSION: It would seem that LILT provides no advantages in the management of minor postoperative wounds over current practice. Despite no apparent benefit of infrared laser at this dosage in the management of acute stage wounds, further research is required to determine its potential efficacy in the management of other wound types. 14 Th World Congress of International Union of Phlebology Rome 9-14 Sept 2001, Abstract P 243 Low lever laser therapy (LLL) in chronic venous insufficiency V.I.Kozlov, K.T.Zaitzev, O.A.Terman Aims: To estimate a range of changeability in rnicrocirculation (MC) under LLL-therapy, as well as to determine a pathogenic role of microcirculation activation in complex treatment of chronic venous insufficiency (CVI) in low limbs. Material and methods: We have investigated 91 patients with CVI and trophic impairments (ulcers). LLL-energy (wavelength 0.83 pin) application to the surface of a trophic ulcer and also laser reflexotherapy (wavelength 1.3 pin) at the body acupuncture points and the points of the ear lobe were used. The treatment session involved 15 , = 20 procedures every day. The rnicrocirculation was studied with conjunctival and skin biomicroscopy and the Laser Doppler Fluxmetry (LDF). Results: The comparison of biomicroscopy and LDF results indicates a high correlation between these two methods. Disturbances of blood inflow and outflow, decrease of capillary blood flow, rheological disorders, leukocyte adhesion and derangements of permeability were identified as the pathogenic signs of CVI. The amplitude-frequency analysis of flux motions ascertained the disorder of correlation between the low-frequent rhythms, which characterize vasomotions, and the high-frequent rhythms, connected with respiration and cardiac pulsation. After LLL-therapy ulcer healing took place in 71% of patients; noticeable improvement in 12% and a recurrence rate within 1 year was 6%. Clinical effect of LLL-therapy has been accompanied by disappearance of microcirculation disorders. Conclusion: LLL-therapy in combined treatment of CVI patients has been successful. The essence of its pathogenic effect is based on the photostimulation of microcirculation and reparative processes. Pol Merkuriusz Lek 2001 Nov;11(65):418-21 Laser's biostimulation in healing or crural ulcerations Krol P, Franek A, Hunka-Zurawinska W, Bil J, Swist D, Polak A, Bendkowski W Katedra i Zaklad Biofizyki Lekarskiej Slaskiej Akademii Medycznej w Katowicach The objective of this paper was to evaluate effect of laser's biostimulation on the process of healing of crural ulcerations. Three comparative groups of patients, A, B and C, were made at random from the patients with venous crural ulcerations. The group A consisted of 17, the group B 15, the group C 17 patients. The patients in all comparative groups were treated pharmacologically and got compress therapy. Ulcerations at patients in group A were additionally irradiated by light of biostimulation's laser (810 nm) in this way that every time ulcerations got dose of energy 4 J/cm2. The patient's in-group B additionally got blind trial (with placebo in the form of quasi-laserotherapy). The evaluated factors were to estimate how laser's biostimulation causes any changes of the size of the ulcers and of the volume of tissue defect. The speed of changes of size and volume of tissue defect per week was calculated. After the treatment there was statistically significant decrease of size of ulcers in all comparative groups while there was no statistically significant difference between the groups observed. After the treatment there was statistically significant decrease of volume of ulcers only in groups A and C but there was no statistically significant difference between the groups observed. Lasers Surg Med. 1997;20(1):56-63. Comment in: Lasers Surg Med. 2001;29(2):105-6. Effects of photostimulation on wound healing in diabetic mice Yu W, Naim JO, Lanzafame RJ Background And Objective: Low-level laser irradiation at certain fluences and wavelengths can enhance the release of growth factors from fibroblasts and stimulate cell proliferation in vitro. We evaluated whether low-level laser irradiation can improve wound healing in diabetes mellitus. Study Design/Materials And Methods: Genetically diabetic mice (C57BL/Ksj/db/db) were used as the animal model for this wound healing study. The experimental animals were divided among four groups: negative control, positive control (topical basic fibroblast growth factor [bFGF] on wound), laser therapy group; and a combination group of laser therapy and topical bFGF. An argon dye laser (Lexel Auora Model 600) at a wavelength of 630 nm and an output of 20 m W/cm2 was used as the light source. The speed of wound closure and histological evaluation were used to analyze the experimental results. Results: Laser irradiation enhanced the percentage of wound closure over time as compared to the negative control group (58.4 +/- 2.6 vs. 40.8 +/- 3.4 at day 10 and 95.7 +/- 2 vs. 82.3 +/- 3.6 at day 20, P < .01). Histological evaluation showed that laser irradiation improved wound epithelialization, cellular content, granulation tissue formation, and collagen deposition in laser-treated wounds as compared to the negative control group (6.4 +/- 0.16 vs. 3.8 +/- 0.13 at day 10 and 12 +/- 0.21 vs. 8.2 +/- 0.31, P < .01). Conclusion: This study of laser biostimulation on wound healing in diabetic mice suggests that such therapy may be of great benefit in the treatment of chronic wounds that occur as a complication of diabetes mellitus. Lasers Med Sci 2002, 17:110-134 Review article Wound healing in cell studies and animal model experiments by low level laser therapy; were clinical studies justified ? A systematic Review C. Lucas, L.J. Criens-Poublon, C.T. Cockrell and R.J. de Hann Based on results of cell studies and animal experiments, clinical trials with Low Level Laser Therapy (LLLT) were performed, which finally did not demonstrate a beneficial effect on outcome of wound healing. The aim of this study was to investigate whether the evidence from cell studies and animal experiments with respect tu wound healing was unequivocally in favour of LLLT, which would imply that these models might be adequate to predict treatment response in patients, or that the data of cell studies and animal experiments were inconclusive, which would mean that the clinical trials were based on insuftcient evidence. We performed a systematic review of cell studies and animal experiment with LLLT on wound healing. Manuscripts were identified by searching Medline, Embase, and SPIE (the International Society for Optical Engineering). We assessed whether studies showed a beneficial effect of active treatment or not. The effect size was expressed in standardised mean difference [(SMD) the mean outcome measure of the treatment group minus the mean outcome measure of the control group, divided by the pooled standard deviation of these measurements]. In-depth analyses were perfomed on (1) studies in which infiicted wounds on animals were irradiated and evaluated; (2) studies with primary outcome measures on dimensions with direct reference to wound healing (ranging from acceleration of wound closure to epithelialisation, but excluding surrogate dimensions with regard to wound healing; in this case: tensile strength); (3) animal studies with `true controls'; (4) studies in which animals functioned as their `own controls' and (5) studies with the highest methodological quality score. The 36 included studies contained 49 outcome parameters of which 30 reported a positive effect of laser irradiation and 19 did not. Eleven studies presented exact data about the effect of active treatment and controls. The pooled effect size (SMD) over 22 outcome measures of these studies was - 1.05 (95% CI: -1.67 to 0.43) in favour of LLLT. Methodological quality of the studies was poor. In-depth analysis of studies showed no significant pooled effect size in studies with highest methodological quality scores [0.06 (95% CI: - 0.42 Io 0.53)]. Summarising the data of cell studies and animal experiments, reviewed in this manuscript, these studies failed to show unequivocal evidence Io substantiate the decision for trials with LLLT in a large number of patients. In tact, there were no diflerences between the results of these experiments and clinical studies. Remarkably, we found that (almost from the introduction on) animal experiments and clinical studies that adress the biological eflects of LLLT on wound healing, ran simultaneously, rather than in sequence. We conclude that this type of phototherapy should not be considered a valuable (adjuvant) treatment for this selected, generally therapy-refractory condition in humans. J Clin Laser Med Surg 2002 Jun;20(3):109-16 Low-intensity laser therapy/combined phototherapy in the management of chronic venous ulceration: a placebo-controlled study Lagan KM, McKenna T, Witherow A, Johns J, McDonough SM, Baxter GD Objective: The current placebo-controlled study was undertaken to investigate the efficacy of combined phototherapy and low-intensity laser therapy (LILT) in the management of chronic venous ulceration when used in conjunction wit standardized nursing intervention. Materials And Methods: Approval was granted by Research Ethical Committees at the University of Ulster and Altnagelvin Hospitals Health and Social Services Trust. Patients (n = 15; 10 female/5 male; age +/- SD = 69.9 +/- 13.8 years) were recruited from an outpatient "leg ulcer clinic," where they attended once per week for irradiation/sham treatments for 4 weeks. Treatment was withheld for a total of 8 weeks, and patients were reviewed during this time (weeks 8 and 12) for ulcer and pain assessment only. A multisource diode array (660-950 nm) was used for irradiation; parameters were kept constant for the duration of the study (532 mW; 5 kHz; 12 J/cm(2)). Wound and pain assessment were carried out by an independent investigator. Digitizing was used to quantify surface areas from wound tracings. Results: Although there was no statistically significant difference between Treatment and Placebo groups, an apparent clinical difference in wound healing rate was noted; at postirradiation, a continued reduction in wound size was evident for the treatment group. These effects were believed to be due to an apparent delayed effect. There was no statistically significant difference between groups for pain. Conclusion: These findings provide only limited evidence for the use of this modality as an adjunctive therapy with current nursing intervention. Further group studies are indicated to investigate the apparent delayed effect reported here for various etiologies of ulceration. Microvasc Res 2002 Sep;64(2):240-6 Systemic effects of low-intensity laser irradiation on skin microcirculation in patients with diabetic microangiopathy Schindl A, Heinze G, Schindl M, Pernerstorfer-Schon H, Schindl L Low-intensity laser irradiation has been shown to induce wound healing in conditions of reduced microcirculation, which is in part explained by systemic effects. We therefore investigated such a potential systemic effect of low-intensity laser irradiation on skin blood circulation in patients with diabetic microangiopathy. Patients with diabetic microangiopathy were randomized to receive either a single helium-neon (HeNe, 632.8 nm) low-intensity laser irradiation with a dose of 30 J/cm(2) or a sham irradiation over the forefoot region in a double-blind, placebo-controlled clinical study. Skin blood circulation by means of temperature recordings over forefoot regions was detected by infrared thermography. Following a single transcutaneous low-intensity laser irradiation, a rise in skin temperature in both feet of the subjects in the laser group was noted, whereas in both feet of the subjects in the placebo group a drop in skin temperature occurred. The baseline-adjusted skin temperature 15 min after the end of the irradiation was significantly higher in the laser-treated forefeet compared to the placebo-"treated" forefeet (p < 0.0001); the baseline-adjusted difference in the temperature was 1.94 +/0.35 degrees C. Simultaneously, the baseline-adjusted skin temperature was significantly higher in the laser-untreated forefeet compared to the placebo-"untreated" forefeet (P < 0.0001); the baseline-adjusted difference was 1.70 +/- 0.33 degrees C. Our data show a significant increase in skin circulation due to athermic laser irradiation in patients with diabetic microangiopathy and point to the possibility of inducing systemic effects. Lasers Surg Med 2002;31(5):343-51 Effects of 810 nm laser irradiation on in vitro growth of bacteria: Comparison of continuous wave and frequency modulated light Nussbaum EL, Lilge L, Mazzulli T Background And Objectives: Low intensity laser therapy may modify growth of wound bacteria, which could affect wound healing. This study compares the effects on bacteria of 810 nm laser using various delivery modes (continuous wave or frequency modulated light at 26, 292, 1,000, or 3,800 Hz). Study Design/Materials And Methods: Staphylococcus (S.) aureus, Escherichia (E.) coli,and Pseudomonas (P.) aeruginosa were plated on agar and then irradiated (0.015W/cm(2); 1-50 J/cm(2)) or used as controls (sham irradiated); growth wasexamined after 20 hours of incubation post exposure. Results: There wereinteractions of species and modulation frequency in the overall effects ofirradiation (P = 0.0001), and in the radiant exposure mediated effects (P =0.0001); thus individual frequencies and each bacterium were analysedseparately. Bacteria increased following 3,800 Hz (P = 0.0001) and 1,000 Hz (P =0.0001) pulsed irradiation; at particular radiant exposures P. aeruginosaproliferated significantly more than other bacteria. Pulsed laser at 292 and 26Hz also produced species-dependent effects (P = 0.0001; P = 0.0005); however,the effects for different radiant exposures were not significant. Bacterialgrowth increased overall, independent of species, using continuous mode laser,significantly so at 1 J/cm(2) (P = 0.02). Analysis of individual speciesdemonstrated that laser-mediated growth of S. aureus and E. coli was dependenton pulse frequency; for S. aureus, however, there was no effect for differentradiant exposures. Further tests to examine the radiant exposure effects on E.coli showed that growth increased at a frequency of 1,000 Hz (2 J/cm(2); P =0.03). P. aeruginosa growth increased up to 192% using pulsed irradiation at1,000-3,800 Hz; whereas 26-292 Hz laser produced only a growth trend. Conclusions: The findings of this study point to the need for wound culturesprior to laser irradiation of infected wounds. Similar investigations usingother common therapeutic wavelengths are recommended. Ned Tijdschr Tandheelkd 2002 Sep;109(9):334-8 Lasers in dentistry 6. The soft laser ten Bosch JJ A soft laser is a low-power laser emitting in the red and near-infrared part of the spectrum. Studies with cell cultures have shown that radiation from a soft laser, when used under proper conditions, promotes cell function and cell proliferation. However, wavelength and dose should be carefully adjusted to an optimum value: too low a dose does not work and neither does a high dose. The dose should be adjusted within an interval of about 10%. In a few animal studies a positive effect on wound healing has been demonstrated, although other studies did not show such an effect. Of the human studies done in the dental field, many do not meet scientific standards because there was no control group or the study was not double-blind. A few studies showed a positive effect but most did not. Perhaps the large variation in results may be explained by the required accuracy of adjustment of the dose, combined with the complicated processes that relate the incident dose to the dose to cells lying on or in tissue. More research, in particular studies in which the dose and wave length are varied systematically, are needed before responsible clinical use can be recommended. Lasers Surg Med 2002;31(4):263-7 Effect of low-power laser irradiation on cell growth and procollagen synthesis of cultured fibroblasts Pereira AN, Eduardo Cde P, Matson E, Marques MM Background And Objectives: In dentistry, low-power lasers have been used in the treatment of dentin hypersensitivity, gingivitis, periodontitis, and different forms of oral ulcers. This in vitro study focuses on the biostimulation of NIH-3T3 fibroblasts by a lowpower Ga-As-pulsed laser. Study Design/Materials And Methods: We have studied cell growth and procollagen synthesis of cultured fibroblasts submitted to low-power laser irradiation with energy densities varying from 3 to 5 J/cm(2) over a period of 1-6 days. The light source was a 120 mW Ga-As diode laser (lambda = 904 nm). Growth curves and procollagen immunoprecipitation were obtained. Results: Irradiation of 3 and 4 J/cm(2) increased the cell numbers about threefold to sixfold comparing to control cultures. However, this effect was restricted to a small range of energy densities since 5 J/cm(2) had no effect on cell growth. The energy density of 3 J/cm(2) remarkably increased cell growth, with no effect on procollagen synthesis, as demonstrated by the immunoprecipitation analysis. Conclusions: Our results showed that a particular laser irradiation stimulates fibroblast proliferation, without impairing procollagen synthesis. J Clin Laser Med Surg 2002 Feb;20(1):37-40 Effects of 1047-nm neodymium laser radiation on skin wound healing Simoes RM, Teixeira D, Maldonado EP, de RW, Zezell DM Previous research in our laboratory has shown that the polarization component of the electrical field plays an important role on the healing process of inflammatory lesions created in the end of the spinal column of Lewis rats, using a He-Ne laser at lambda = 632.8 nm. It is well known that polarization is lost in a turbid medium, such as living tissue. However, the Nd:YLF wavelength (lambda = 1,047 nm) allows more polarization preservation than lambda = 632.8 nm, and the Nd:YLF laser beam has been used in clinical trials as a biostimulating agent. In this work, we investigated the influence of a low-intensity, linearly polarized Nd:YLF laser beam on skin wound healing, considering two orthogonal directions of polarization. We have considered a preferential axis as the animals' spinal column, and we aligned the linear laser polarization first parallel, then perpendicular to this direction. Burns of about 6 mm in diameter were created with liquid N2 on the back of the animals, and the lesions were irradiated on days 3, 7, 10, and 14 postwounding, D = 1.0 J/cm2. Lesions 1 and 2 were illuminated using Nd:YLF pulsed laser radiation. Lesion 1 was irradiated with linear polarization parallel with the rat spinal column. Lesion 2 was irradiated using the same protocol, but the light polarization was aligned with the perpendicular relative orientation. Control lesions were not irradiated. We have taken photographs from the wound areas on the 3rd, 7th, 10th, 14th, and 17th postoperative day for a biometrical analysis. The results have shown that lesion 1 healed faster than the control lesions (p < 0,05), which presented a smaller degree of healing after 14 days postwounding. Med Eng Phys. 2002 Nov;24(9):607-15 Does low output laser stimulation enhance the healing of crural ulceration? Some critical remarks Franek A, Krol P, Kucharzewski M The objective of the experiment was to evaluate the impact of laser stimulation on crural ulceration healing.Three groups were established at random from patients with crural ulceration: A, B and C. Group A included 21 patients, group B included 22 patients and group C, 22 patients. Patients in all groups were treated with pharmaceuticals and with compressive therapy. The ulcers in group A were additionally irradiated with laser light of wavelength 810 nm, so that a dose of 4 J/cm2 was applied in each procedure. Patients in group B were additionally subjected to a blind test (with placebo in the form of quasi laser therapy).At the end of the treatment a statistically significant reduction of the area and volume of the ulcers was found in all groups. No statistically significant difference was found between the groups in terms of average rate of change per week of the relative area of ulceration and average rate of change per week of the relative volume of ulceration. Reduction of infected area was observed in all groups, but a significant change was only observed in group C.No significant impact of laser light (lambda=810 nm, P=65 mW, p=4 J/cm2) on any of the stages of ulceration healing was observed. Am J Clin Dermatol 2003;4(1):1-12 Can thermal lasers promote skin wound healing? Capon A, Mordon S Lasers are now widely used for treating numerous cutaneous lesions, for scar revision (hypertrophic and keloid scars), for tissue welding, and for skin resurfacing and remodeling (wrinkle removal). In these procedures lasers are used to generate heat. The modulation of the effect (volatilization, coagulation, hyperthermia) of the laser is obtained by using different wavelengths and laser parameters. The heat source obtained by conversion of light into heat can be very superficial, yet intense, if the laser light is well absorbed (far-infrared:CO(2) or Erbium:Yttrium Aluminum Garnet [Er:YAG] lasers), or it can be much deeper and less intense if the laser light is less absorbed by the skin (visible or near-infrared). Lasers transfer energy, in the form of heat, to surrounding tissues and, regardless of the laser used, a 45-50 degrees C temperature gradient will be obtained in the surrounding skin. If a wound healing process exists, it is a result of live cells reacting to this low temperature increase. The generated supraphysiologic level of heat is able to induce a heat shock response (HSR), which can be defined as the temporary changes in cellular metabolism. These changes are rapid and transient, and are characterized by the production of a small family of proteins termed the heat shock proteins (HSP). Recent experimental studies have clearly demonstrated that HSP 70, which is over-expressed following laser irradiation, could play a role with a coordinated expression of other growth factors such as transforming growth factor (TGF)-beta. TGFbeta is known to be a key element in the inflammatory response and the fibrogenic process. In this process, the fibroblasts are the key cells since they produce collagen and extracellular matrix. In conclusion, the analysis of the literature, and the fundamental considerations concerning the healing process when using thermal lasers, are in favor of a modification of the growth factors synthesis after laser irradiation, induced by an HSR. An extensive review of the different techniques and several clinical studies confirm that thermal lasers could effectively promote skin wound healing, if they are used in a controlled manner. Br J Dermatol. 2003 Feb;148(2):334-6 Direct stimulatory effect of low-intensity 670 nm laser irradiation on human endothelial cell proliferation Schindl A, Merwald H, Schindl L, Kaun C, Wojta J Background: Endothelial cell (EC) proliferation plays a key role in the process of tissue repair. Low-intensity laser irradiation has been demonstrated to accelerate wound healing and to improve microvascularization. OBJECTIVES: The present study evaluated a possible stimulatory influence of low-intensity laser irradiation on human umbilical vein endothelial cell (HUVEC) proliferation in a systematic manner. Methods: Subconfluent cultures of HUVEC were irradiated every other day with a 670nm diode laser (intensity: 10-65 mW cm(-2), dose: 2-8 J cm(-2)) during a period of 6 days. Cell proliferation was evaluated quantitatively by counting in a haemocytometer. Results: Our data demonstrate a dose-dependent and intensity-dependent stimulatory effect of laser irradiation on HUVEC cell proliferation. Doses of between 2 and 8 J cm(-2) induced statistically significant cell proliferation. Testing different intensities at a constant dose of 8 J cm(-2), 20 and 65 mW cm(-2) induced most pronounced cell proliferation. Conclusions: Low-intensity laser irradiation influences EC proliferation and might thereby contribute to the increase in angiogenesis and the acceleration of wound healing in vivo. J Clin Laser Med Surg. 2003 Jun;21(3):165-70 Low-level laser irradiation attenuates production of reactive oxygen species by human neutrophils Fujimaki Y, Shimoyama T, Liu Q, Umeda T, Nakaji S, Sugawara K Objective: The aim of this study was to examine the effects of low-level laser therapy (LLLT) on production of reactive oxygen (ROS) species by human neutrophils. Background Data: LLLT is an effective therapeutic modality for inflammatory conditions. Materials And Methods: The laser device used was the infrared diode laser (GaAlAs), 830-nm continuous wave (150 mW/cm² ). After irradiation, ROS production by neutrophils was measured using luminol-dependent chemiluminescence (LmCL) and expression of CD11b and CD16 on neutrophil surface was measured by flow cytometry. Results: The LmCL response of neutrophils was reduced by laser irradiation at 60 min prior to the stimulation with opsonized zymosan and calcium ionophore. The attenuating effect of LLLT was larger in neutrophils of smokers than non-smokers, while the amount of produced ROS was larger in neutrophils of smokers. Expression of CD11b and CD16 on neutrophil surface was not affected by LLLT. CONCLUSION: Attenuation of ROS production by neutrophils may play a role in the effects of LLLT in the treatment of inflammatory tissues. There is a possible usage of LLLT to improve wound healing in smokers. Lasers Med Sci. 2003;18(2):72-7 Efficacy of low-level laser therapy in the management of stage III decubitus ulcers: a prospective, observer-blinded multicentre randomised clinical trial Lucas C, van Gemert MJ, de Haan RJ Low-level laser therapy (LLLT) has been suggested as a promising treatment option for open wounds. In view of the absence of randomised studies with sufficiently large sample sizes, we assessed the efficacy of LLLT in the treatment of stage III decubitus ulcers. We performed a prospective, observer-blinded multicentre randomised clinical trial to assess the effect of LLLT as adjuvant to standard decubitus care. A total of 86 patients were enrolled into the study. Treatment was the prevailing consensus decubitus treatment (n=47); one group (n=39) had LLLT in addition, five times a week over a period of 6 weeks. The primary outcome measure was the absolute (mm2) and relative (%) wound size reduction at 6 weeks compared to baseline. Secondary outcome measures were the number of patients developing a stage IV ulcer during the study period, and the median change in Norton scores at 6 weeks compared to baseline. Based on the intention-totreat principle, using last-observation-carried-forward analyses, Mann-Whitney U tests showed that the differences between the two groups in terms of absolute improvement (p=0.23) and relative improvement (p=0.42) were not significant. Because the wound size areas were non-normally distributed, we also analysed the data after logarithmic transformation of the wound size measurements. No significant difference in log(e) improvement scores between groups could be demonstrated (unpaired t-test: p=0.59). During the treatment period 11% of the patients in the control group and 8% of the patients in the LLLT group developed a stage IV decubitus ulcer (Fisher's exact test: p=0.72). The patients' Norton scores did not change during the treatment period. In this trial we found no evidence that justifies using low-level laser therapy as an adjuvant to the consensus decubitus ulcer treatment. J Biol Chem. 2005 Feb 11;280(6):4761-71. Epub 2004 Nov 22 Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase Wong-Riley MT, Liang HL, Eells JT, Chance B, Henry MM, Buchmann E, Kane M, Whelan HT Far red and near infrared (NIR) light promotes wound healing, but the mechanism is poorly understood. Our previous studies using 670 nm light-emitting diode (LED) arrays suggest that cytochrome c oxidase, a photoacceptor in the NIR range, plays an important role in therapeutic photobiomodulation. If this is true, then an irreversible inhibitor of cytochrome c oxidase, potassium cyanide (KCN), should compete with LED and reduce its beneficial effects. This hypothesis was tested on primary cultured neurons. LED treatment partially restored enzyme activity blocked by 10-100 microm KCN. It significantly reduced neuronal cell death induced by 300 microm KCN from 83.6 to 43.5%. However, at 1-100 mm KCN, the protective effects of LED decreased, and neuronal deaths increased. LED significantly restored neuronal ATP content only at 10 microm KCN but not at higher concentrations of KCN tested. Pretreatment with LED enhanced efficacy of LED during exposure to 10 or 100 microm KCN but did not restore enzyme activity to control levels. In contrast, LED was able to completely reverse the detrimental effect of tetrodotoxin, which only indirectly down-regulated enzyme levels. Among the wavelengths tested (670, 728, 770, 830, and 880 nm), the most effective ones (830 nm, 670 nm) paralleled the NIR absorption spectrum of oxidized cytochrome c oxidase, whereas the least effective wavelength, 728 nm, did not. The results are consistent with our hypothesis that the mechanism of photobiomodulation involves the up-regulation of cytochrome c oxidase, leading to increased energy metabolism in neurons functionally inactivated by toxins. Photomed Laser Surg. 2004 Aug;22(4):281-90 Photobiomodulation improves cutaneous wound healing in an animal model of type II diabetes Byrnes KR, Barna L, Chenault VM, Waynant RW, Ilev IK, Longo L, Miracco C, Johnson B, Anders JJ OBJECTIVE: We investigated the effects of photobiomodulation (PBM) on cutaneous wound healing in an animal model of type II diabetes, Psammomys obesus (Sand Rats). Background Data: 632-nm light has been established as the most effective wavelength for treatment of cutaneous wounds; however, the inconsistent efficacy of PBM may be due to inadequate treatment parameter selection. Methods: Using 632-nm light, an initial series of experiments were done to establish optimal treatment parameters for this model. Following creation of bilateral full-thickness skin wounds, non-diabetic Sand Rats were treated with PBM of differing dosages. Wound healing was assessed according to wound closure and histological characteristics of healing. Optimal treatment parameters were then used to treat type II diabetic Sand Rats while a diabetic control group received no irradiation. In order to elucidate the mechanism behind an improvement in wound healing, expression of basic fibroblast growth factor (bFGF) was assessed. Results: Significant improvement in wound healing histology and wound closure were found following treatment with 4 J/cm(2) (16 mW, 250-sec treatments for 4 consecutive days; p < 0.05). The 4 J/cm(2) dosage significantly improved histology and closure of wounds in the diabetic group in comparison to the non-irradiated diabetic group. Quantitative analysis of bFGF expression at 36 h post-injury revealed a threefold increase in the diabetic and non-diabetic Sand Rats after PBM. Conclusions: The results demonstrate that PBM at an energy density of 4 J/cm(2) is effective in improving the healing of cutaneous wounds in an animal model of type II diabetes, suggesting that PBM (632 nm, 4 J/cm(2)) would be effective in treating chronic cutaneous wounds in diabetic patients. Mitochondrion. 2004 Sep;4(5-6):559-67 Mitochondrial signal transduction in accelerated wound and retinal healing by near-infrared light therapy Eells JT, Wong-Riley MT, VerHoeve J, Henry M, Buchman EV, Kane MP, Gould LJ, Das R, Jett M, Hodgson BD, Margolis D, Whelan HT Photobiomodulation by light in the red to near infrared range (630-1000 nm) using low energy lasers or light-emitting diode (LED) arrays has been shown to accelerate wound healing, improve recovery from ischemic injury in the heart and attenuate degeneration in the injured optic nerve. Recent evidence indicates that the therapeutic effects of red to near infrared light result, in part, from intracellular signaling mechanisms triggered by the interaction of NIR light with the mitochondrial photoacceptor molecule cytochrome c oxidase. We have demonstrated that NIR-LED photo-irradiation increases the production of cytochrome oxidase in cultured primary neurons and reverses the reduction of cytochrome oxidase activity produced by metabolic inhibitors. We have also shown that NIR-LED treatment prevents the development of oral mucositis in pediatric bone marrow transplant patients. Photobiomodulation improves wound healing in genetically diabetic mice by upregulating genes important in the promotion of wound healing. More recent studies have provided evidence for the therapeutic benefit of NIR-LED treatment in the survival and functional recovery of the retina and optic nerve in vivo after acute injury by the mitochondrial toxin, formic acid generated in the course of methanol intoxication. Gene discovery studies conducted using microarray technology documented a significant upregulation of gene expression in pathways involved in mitochondrial energy production and antioxidant cellular protection. These findings provide a link between the actions of red to near infrared light on mitochondrial oxidative metabolism in vitro and cell injury in vivo. Based on these findings and the strong evidence that mitochondrial dysfunction is involved in the pathogenesis of numerous diseases processes, we propose that NIR-LED photobiomodulation represents an innovative and non-invasive therapeutic approach for the treatment of tissue injury and disease processes in which mitochondrial dysfunction is postulated to play a role including diabetic retinopathy, age-related macular degeneration, Leber's hereditary optic neuropathy and Parkinson's disease. Photomed Laser Surg. 2005 Jun;23(3):268-72 Effects of 670-nm phototherapy on development. Yeager RL, Franzosa JA, Millsap DS, Angell-Yeager JL, Heise SS, Wakhungu P, LimJ, Whelan HT, Eells JT, Henshel DS Objective: The objective of the present study was to assess the survival and hatching success of chickens (Gallus gallus) exposed in ovo to far-red (670-nm) LED therapy. Background Data: Photobiomodulation by light in the red to near-infrared range (6301000 nm) using low-energy lasers or light-emitting diode (LED) arrays has been shown to accelerate wound healing and improve recovery from ischemic injury. The mechanism of photobiomodulation at the cellular level has been ascribed to the activation of mitochondrial respiratory chain components resulting in initiation of a signaling cascade that promotes cellular proliferation and cytoprotecton. Materials And Methods: Fertile chicken eggs were treated once per day from embryonic days 0-20 with 670-nm LED light at a fluence of 4 J/cm2. In ovo survival and death were monitored by daily candling (after Day 4). Results: We observed a substantial decrease in overall and third-week mortality rates in the light-treated chickens. Overall, there was approximately a 41.5% decrease in mortality rate in the light-treated chickens (NL: 20%; L: 11.8%). During the third week of development, there was a 68.8% decrease in the mortality rate in light-treated chickens (NL: 20%; L: 6.25%). In addition, body weight, crown-rump length, and liver weight increased as a result of the 670-nm phototherapy. Light-treated chickens pipped (broke shell) earlier and had a shorter duration between pip and hatch. Conclusion: These results indicate that 670-nm phototherapy by itself does not adversely affect developing embryos and may improve the hatching survival rate. Rozhl Chir. 2005 Aug;84(8):417-21 Effect of laser irradiation of diode laser on healing of surgical wounds in rats Vidinsky B, Gal P, Toporcer T, Balogacova M, Hutnanova Z, Kilik R, Bober J, Sabo J, Longauer F The aim of this work was to continue in previous study, which concerns biostimulation of skin wound healing evaluated after 24, 48, 120, 168 hours and so complete the chronological continuance of the process during the first seven days. Male, Sprague Dawley rats (n=21) were used for the experiment. The rats were divided into 3 groups of 7 animals. In general anaesthesia (combination of xylazine, ketamine and tramadol) under aseptic condition two 3,5 cm long parallel skin incisions were performed on the left and right side of the rats spine and immediately sutured. The left wounds were daily stimulated with the diode laser (670 nm). The right wounds were not stimulated and served as control. The specimens of skin wounds were removed for histological evaluation 72, 96 and 144 hours after surgery. The biological specimens were stained with hematoxylin and eosin and histopathologically evaluated. In summary, in our histomorphological study of the influence of laser irradiation on primary wound healing evaluated after 72, 96 and 144 hours was concluded, that the healing of stimulated wounds was accelerated in comparison with controls. The histological evaluation showed earlier regress of inflammatory phase, faster finishing of reepithelization and acceleration in maturation phase. Presented experimental study completes the previous study and achieves the positive effect of biostimulation on all phases of skin wound healing in vivo. J Wound Care. 2005 Sep;14(8):391-4 Comment in: J Wound Care. 2005 Nov;14(10):478-9; author reply 478 Does the use of low-level laser influence wound healing in chronic venous leg ulcers? Kopera D, Kokol R, Berger C, Haas J Objective: Venous leg ulcer treatment often requires months or years of regular wound care by trained staff. It has been suggested that low-level laser irradiation has a biostimulative and wound healing effect, but this has not been clinically verified by controlled studies. This study aimed to compare the effectiveness of low-level laser irradiation with that of a placebo 'light source'. Method: Forty-four patients were assigned to two treatment groups (laser and placebo) or a third group (standardised treatment only) to quantify the effect of the laser therapy. Patients in all three groups received standardised wound care (disinfection, a hydrofibre dressing and compression bandaging). Ulcer size was measured at baseline (day 1), at the end of therapy (day 28) and then two months later (day 90). The relative difference in wound size was evaluated. Results: The difference in the reduction in wound size was not statistically significant in all three groups. A positive effect of using the non-laser device (placebo effect) was demonstrated in some patients. Conclusion: These study results suggest that low-level laser does not stimulate wound healing in venous leg ulcers. Further controlled studies are needed to clarify the efficacy of low-level laser treatment as a wound-healing stimulant. Photomed Laser Surg. 2005 Oct;23(5):485-92 Polarized light (400-2000 nm) and non-ablative laser (685 nm): a description of the wound healing process using immunohistochemical analysis Pinheiro AL, Pozza DH, Oliveira MG, Weissmann R, Ramalho LM Objective: This study aimed to describe, through morphologic and cytochemical analysis, the healing process of wounds submitted (or not) to laser therapy (lambda 685 nm) or polarized light (lambda 400-2000 nm). Background Data: There are many reports on different effects of several types of phototherapies on the treatment of distinct conditions, amongst them, on wound healing. Laser therapy and the use of polarized light are still controversial despite successive reports on their positive effects on several biological processes. Methods: Thirty male Wistar rats, approximately 4 months old, were used, and standardized excisional wounds were created on their dorsum. The wounds were irradiated in four equidistant points with laser light or illuminated with polarized light, both with doses of 20 or 40 J/cm2. Group 1 acted as untreated controls. Animals were irradiated every 48 h during 7 days, starting immediately after surgery, and were humanely killed on the 8th post-operative day. Specimens were taken and routinely processed and stained with H&E, and for descriptive analysis of myofibroblasts and collagen fibers, the specimens were imunnomarked by smooth muscle alpha-actin and picrosirius stain. Results: Control specimens showed the presence of ulceration, hyperemia, discrete edema, intense, and diffuse inflammation, collagen deposition was irregular, and myofibroblasts were seen parallel to the wound margins. Wounds treated by laser therapy with a dose of 20 J/cm2 showed mild hyperemia, inflammation varied from moderate to intense, the number of fibroblasts was large, and the distribution of collagen fibers was more regular. Increasing the dose to 40 J/cm2 evidenced exuberant neovascularization, severe hyperemia, moderate to severe inflammation, large collagen deposition, and fewer myofibroblasts. On subjects illuminated with polarized light with a dose of 20 J/cm2, mild to moderate hyperemia was detectable, and collagen matrix was expressive and unevenly distributed; a larger number of myofibroblasts was present and no re-epithelialization was seen. Increasing the dose resulted in mild to moderate hyperemia, no re-epithelialization was seen, edema was discrete, and inflammation was moderate. Conclusion: The use of 685-nm laser light or polarized light with a dose of 20 J/cm2 resulted in increased collagen deposition and better organization on healing wounds, and the number of myofibroblast was increased when polarized light is used. Biofizika. 2005 Nov-Dec;50(6):1137-44 A comparative study of the effects of laser and light-emitting diode irradiation on the wound healing and functional activity of wound exudate leukocytes Klebanov GI, Shuraeva NIu, Chichuk TV, Osipov AN, Rudenko TG, Shekhter AB, Vladimirov IuA The effects of coherent He-Ne laser and non-coherent light-emitting diode radiation on rat skin wound healing and functional activity of wound excudate leukocytes were compared. A comparative pathomorphological analysis showed that the He-Ne laser and light-emitting diode irradiation stimulated the transition of the inflammatory phase of the wound healing into the reparative (proliferative) and scarring phases sequentially. It was also detected that the functional activity of leucocytes changed in a dose-dependent manner. The leukocyte activity was found to be similar in the groups with laser and lightemitting diode irradiation. Thus, we can conclude that coherent laser and non-coherent light-emitting diode radiation have very close effects on wound healing and activity of wound exudate leukocytes, and coherence is not required for this activity. Khirurgiia (Mosk). 2005;(4):37-41 Surgical technologies in the treatment of varicose veins of the lower extremities complicated with trophic ulcer Kuznetsov NA, Barinov VE, Teleshov BV, Trepilets VE, Zheltikov AN Results of an open randomized study of staged treatment of 94 patients suffering from varicose veins of the lower extremities with open infected trophic ulcers of the shank were analyzed. All the patients were divided into 3 groups depending on the treatment variant. Based on this study, clinical efficacy of early correction of upper vertical venousvenous reflux is substantiated. Efficacy of CO(2) laser application for sanation of trophic venous ulcers and practical importance of their auto-venous plastic reconstruction are demonstrated. Thus, up-to-date technologies provide differential treatment in patients with trophic venous ulcers. Dermatol Surg. 2006 Jan;32(1):21-5 Clinical effect of a single pulsed dye laser treatment of fresh surgical scars: randomized controlled trial Alam M, Pon K, Van Laborde S, Kaminer MS, Arndt KA, Dover JS Background: Pulsed dye laser has been used to decrease erythema and telangiectasia associated with scars, including surgical scars. There is limited evidence indicating improved surgical scar appearance if pulsed dye laser treatments are commenced immediately at the time of suture removal. Objective: To determine whether a single one-pass pulsed dye laser treatment at the time of suture removal can improve the appearance of surgical scars. Methods: Randomized controlled trial enrolling 20 patients (complete data for 17 patients) at two geographic sites, with blinded ratings of pre- and post-treatment photographs obtained at various time points. Included patients underwent elliptical excision for atypical nevi of the trunk and/or extremities, with at least one resulting scar of at least 5 cm in length or two scars of at least 2.5 cm in length. For each patient, each scar or half-scar (if a larger scar was used) was randomized to treatment or control groups. Treatment scars received a single one-pass treatment with a 595 nm pulsed dye laser (Vbeam, Candela Corporation, Wayland, MA, USA) at the time of suture removal (ie, 2 weeks after excision) at the following parameters: 7 J/cm2 fluence, 7 mm spot size, 1.5-millisecond pulse duration, and 30-millisecond spray, 20-millisecond delay of dynamic cooling. The treatment area included 1 cm on either side of the scar, and the round laser spots were overlapped 10%. Control scars were not treated with laser. Results: Immediate purpura was induced from the laser treatment Six weeks after laser treatment, no significant difference was found in the clinical appearance of surgical scars treated with a single pulsed dye laser treatment on suture removal day versus those surgical scars not treated with laser. Parameters on which no significant difference was found included visibility of incision, erythema, hyperpigmentation, hypopigmentation, induration, and atrophy. Both sets of scars improved over time. Conclusions: A single pulsed dye laser treatment at the time of suture removal does not appear to have a beneficial effect on clinical scar appearance. The point of minimal benefit for such laser treatments may lie somewhere between one and three treatments. Lasers Surg Med. 2006 Jan;38(1):74-83 The role of laser fluence in cell viability, proliferation, and membrane integrity of wounded human skin fibroblasts following helium-neon laser irradiation Hawkins DH, Abrahamse H Background: In medicine, lasers have been used predominantly for applications, which are broadly termed low level laser therapy (LLLT), phototherapy or photobiomodulation. This study aimed to establish cellular responses to Helium-Neon (632.8 nm) laser irradiation using different laser fluences (0.5, 2.5, 5, 10, and 16 J/cm(2)) with a single exposure on 2 consecutive days on normal and wounded human skin fibroblasts. Materials And Methods: Changes in normal and wounded fibroblast cell morphology were evaluated by light microscopy. Changes following laser irradiation were evaluated by assessing the mitochondrial activity using adenosine triphosphate (ATP) luminescence, cell proliferation using neutral red and an alkaline phosphatase (ALP) activity assay, membrane integrity using lactate dehydrogenase (LDH), and percentage cytotoxicity and DNA damage using the Comet assay. Results: Morphologically, wounded cells exposed to 5 J/cm(2) migrate rapidly across the wound margin indicating a stimulatory or positive influence of phototherapy. A dose of 5 J/cm(2) has a stimulatory influence on wounded fibroblasts with an increase in cell proliferation and cell viability without adversely increasing the amount of cellular and molecular damage. Higher doses (10 and 16 J/cm(2)) were characterized by a decrease in cell viability and cell proliferation with a significant amount of damage to the cell membrane and DNA. Conclusions: Results show that 5 J/cm(2) stimulates mitochondrial activity, which leads to normalization of cell function and ultimately stimulates cell proliferation and migration of wounded fibroblasts to accelerate wound closure. Laser irradiation can modify cellular processes in a dose or fluence (J/cm(2)) dependent manner. Biofizika. 2006 Jan-Feb;51(1):116-22 A comparison of the effects of laser and light-emitting diodes on superoxide dismutase activity and nitric oxide production in rat wound fluid Klebanov GI, Shuraeva NIu, Chichuk TV, Osipov AN, Vladimirov IuA The action of laser and light-emitting diode radiation in the visible region on the content of reactive nitrogen species and activity of superoxide dismutase in rat wound fluid was studied, and efficiency of action of coherent laser and incoherent light emitting diode radiations in the red region of the spectrum on the parameters under study was compared. A model of incised aseptic wounds in rats proposed by L.I. Slutskiy was used. A He-Ne laser (632 nm) and a Y-332B light emitting diode served as radiation sources. It was shown that (1) exposure of wounds to the visible light of both laser and lightemitting diodes causes dose-dependent changes in superoxide dismutase activity and production of nitrites and (2) the radiation coherence does not play any significant role in the changes of superoxide dismutase activity or nitrogen oxide formation by wound fluid phagocytes. Lasers Med Sci. 2006 Apr;21(1):5-10. Epub 2006 Mar 17 Closure of skin incisions by 980-nm diode laser welding Gulsoy M, Dereli Z, Tabakoglu HO, Bozkulak O A 980-nm diode laser is proposed to be an alternative welding laser in dermatology due to its optimal penetration in tissue. An in vivo predosimetry study was done to estimate the optimal laser energy delivery conditions (6 W, 400 ms). Next, in vivo experiments were comparatively performed to examine healing of wounds closed either with suture or laser welding. One-centimeter-long, full-thickness incisions were done on the dorsal side of Wistar rats. Wounds were surgically removed at 1, 4, 7, 14, and 21 days postoperatively. Macroscopic examinations showed that welding had minimal scarring and a fine quality healing. According to histological (hematoxylin and eosin staining) results, change of epidermal thickness and granulation tissue formation through 21 days of healing period showed similarities in both methods. Epidermal thickness of welded wounds decreased from 62.46+/-6.87 microm (first day) to 36.49+/-0.92 microm (21st day) and that of sutured wounds decreased from 62.94+/-13.53 microm (first day) to 37.88+/-7.41 microm (21st day). At day 14, epidermal thickness of sutured wounds (61.20+/-6.60 microm) were higher than welded wounds (49.69+/-6.31 microm) (p<0.05). Besides, granulation values were greater for the sutured wounds but the difference was statistically significant (p<0.05) only for the seventh day (197,190.29+/.89,554.96 microm(2) for sutured wounds, 138,433.1+/-51,077.17 microm(2) for welded wounds). Those differences indicate a faster recovery with laser welding. It is concluded that tissue welding with a 980-nm diode laser can be a good candidate for tissue welding applications with accelerated and improved healing, but further investigations are in progress for clinical use. Photomed Laser Surg. 2006 Apr;24(2):121-8 Clinical and experimental applications of NIR-LED photobiomodulation Desmet KD, Paz DA, Corry JJ, Eells JT, Wong-Riley MT, Henry MM, Buchmann EV, Connelly MP, Dovi JV, Liang HL, Henshel DS, Yeager RL, Millsap DS, Lim J, Gould LJ, Das R, Jett M, Hodgson BD, Margolis D, Whelan HT This review presents current research on the use of far-red to near-infrared (NIR) light treatment in various in vitro and in vivo models. Low-intensity light therapy, commonly referred to as "photobiomodulation," uses light in the far-red to near-infrared region of the spectrum (630-1000 nm) and modulates numerous cellular functions. Positive effects of NIR-light-emitting diode (LED) light treatment include acceleration of wound healing, improved recovery from ischemic injury of the heart, and attenuated degeneration of injured optic nerves by improving mitochondrial energy metabolism and production. Various in vitro and in vivo models of mitochondrial dysfunction were treated with a variety of wavelengths of NIR-LED light. These studies were performed to determine the effect of NIR-LED light treatment on physiologic and pathologic processes. NIRLED light treatment stimulates the photoacceptor cytochrome c oxidase, resulting in increased energy metabolism and production. NIR-LED light treatment accelerates wound healing in ischemic rat and murine diabetic wound healing models, attenuates the retinotoxic effects of methanol-derived formic acid in rat models, and attenuates the developmental toxicity of dioxin in chicken embryos. Furthermore, NIR-LED light treatment prevents the development of oral mucositis in pediatric bone marrow transplant patients. The experimental results demonstrate that NIR-LED light treatment stimulates mitochondrial oxidative metabolism in vitro, and accelerates cell and tissue repair in vivo. NIR-LED light represents a novel, noninvasive, therapeutic intervention for the treatment of numerous diseases linked to mitochondrial dysfunction. J Photochem Photobiol B. 2006 May 1;83(2):87-93. Epub 2006 Feb 7 Effect of low-level helium-neon laser therapy on the healing of third-degree burns in rats Bayat M, Vasheghani MM, Razavi N This paper presents the results of a study on the effects of low-level helium-neon laser therapy (LL He-Ne LT) on the healing of burns. Seventy-eight adult male rats, having been subjected to third-degree burns, were randomly divided into four groups: two laser treated groups (n=20, each), one control group (n=19) and one nitrofurazone treated group (n=19). In the two laser treated groups, the burns were treated on a daily basis with LL He-Ne LT with an energy density of 1.2 and 2.4 J/cm(2), respectively. The response to treatment was assessed histologically at 7, 16 and 30 days after burning, and microbiologically at day 15. Analysis of variance showed that the mean of blood vessel sections in the 1.2J/cm(2) laser group was significantly higher than those in the other groups and the mean of the depth of new epidermis in the 2.4 J/cm(2) laser group on day 16 was significantly lower than in the nitrofurazone treated group (P=0.025, P=0.047, respectively). When Staphylococcus aureus and Pseudomonas aeruginosa grew in more than 50% of samples obtained from control group, there were no S. aureus and P. aeruginosa in the samples of 2.4 J/cm(2) laser group. It is concluded that LL He-Ne LT induced the destruction of S. aureus and P. aeruginosa in third-degree burns of rats, yet at the same time our histological findings showed that LL He-Ne LT caused a significant increase in the mean of blood vessel sections on day 7 after third degree burns and a decrease in the mean of the depth of new epidermis on day 16 after the same burns in rats. Photomed Laser Surg. 2006 Jun;24(3):389-96 Effects of laser therapy in CO2 laser wounds in rats Grbavac RA, Veeck EB, Bernard JP, Ramalho LM, Pinheiro AL Objective: The aim of this study was to assess the effects of laser therapy and its possible dose dependency on the healing of CO2 laser surgical wounds. Background Data: Several reports from our group and others have indicated that light therapies may improve healing, depending on wavelength, dose, intensity of the light, and both local and systemic conditions. METHODS: Circular surgical wounds were created on the dorsum of Wistar rats, which were separated into three groups (A, B, and C). Group A acted as control and had no additional treatment. Groups B and C were irradiated with GaAlAs lambda685-nm laser light, either with 20 J/cm2 (Group B) or 40 J/cm2 (Group C). The animals were humanely killed at the end of the experimental period; specimens were taken and routinely processed to wax and stained with Hematoxylin and Eosin, Sirius Red, and alpha-Smooth Muscle Actin (alphaSMA). Results: Laser-irradiated groups showed a healing process characterized by a more prominent fibroblastic proliferation, with young fibroblasts actively producing collagen; no myofibroblasts were found. No statistically significant differences were observed when the different doses were compared. Conclusion: It may be concluded that, using this methodology, laser therapy has a positive effect in wound healing produced by CO2 laser, and the dose has no influence on the treatment. Photomed Laser Surg. 2006 Aug;24(4):474-9 Comparison between wound healing in induced diabetic and nondiabetic rats after low-level laser therapy Rabelo SB, Villaverde AB, Nicolau R, Salgado MC, Melo Mda S, Pacheco MT Objective: The aim of this work was to compare the effect of low-level laser therapy (LLLT) on the wound healing process in nondiabetic and diabetic rats. Background Data: Among the clinical symptoms caused by diabetes mellitus, a delay in wound healing is a potential risk for patients. It is suggested that LLLT can improve wound healing. Methods: The tissue used for this study was extracted from animals suffering from diabetes, which was induced by Streptozotocin, and from nondiabetic rats. Animals were assembled into two groups of 25 rats each (treated and control) and further subdivided into two groups: diabetic (n = 15) and nondiabetic (n = 10). A full-thickness skin wound was made on the dorsum area, with a round 8-mm holepunch. The treated group was irradiated by a HeNe laser at 632.8 nm, with the following parameters: 15 mW, exposition time of 17 sec, 0.025 cm2 irradiated area, and energy density of 10 J/cm2. Square full-thickness skin samples (18 mm each side, including both injured and noninjured tissues) were obtained at 4, 7, and 15 days after surgery and analyzed by qualitative and quantitative histological methods. RESULTS: Quantitative histopathological analysis confirmed the results of the qualitative analysis through histological microscope slides. When comparing tissue components (inflammatory cells, vessels and fibroblast/area), we found that treated animals had a less intense inflammatory process than controls. Conclusion: Results obtained by both qualitative and quantitative analyses suggested that irradiation of rats with HeNe (632.8 nm), at the tested dose, promoted efficient wound healing in both nondiabetic and diabetic rats as, compared to the control group. Photomed Laser Surg. 2006 Aug;24(4):480-8 Histological assessment of the effect of laser irradiation on skin wound healing in rats Gal P, Vidinsky B, Toporcer T, Mokry M, Mozes S, Longauer F, Sabo J Objective: The purpose of this study was to evaluate, from the histological point of view, the effect of diode laser irradiation on skin wound healing in Sprague-Dawley rats. Background Data: Various biological effects have been described in different studies after low-level laser therapy (LLLT). METHODS: Two parallel full-thickness skin incisions were performed on the back of each rat (n = 49) and immediately sutured. After surgery, one wound of each rat was exposed to laser irradiation (continuous mode, 670 nm, daily dose 30 J/cm2), whereas the parallel wound was not irradiated and served as control. Both wounds were removed 24, 48, 72, 96, 120, 144, and 168 h after surgery and routinely fixed and embedded in paraffin sections, stained with hematoxylin and eosin, van Gieson, periodic acid Schiff + periodic acid Schiff diastase, Mallory's phosphotungstic hematoxylin, and azur and eosin, and histopathologically evaluated. RESULTS: As compared to non irradiated control wounds, laser stimulation shortened the inflammatory phase as well as accelerated the proliferative and maturation phase, and positively stimulated the regeneration of injured epidermis and the reparation of injured striated muscle. Conclusion: LLLT at 670 nm positively influences all phases of rat skin wound healing. Lasers Surg Med. 2006 Sep;38(8):779-86 Low-level laser irradiation modulates matrix metalloproteinase activity and gene expression in porcine aortic smooth muscle cells Gavish L, Perez L, Gertz SD Background And Objectives: The vascular extracellular matrix is maintained by a dynamic balance between matrix synthesis and degradation. This equilibrium is disrupted in arterial pathologies such as abdominal aortic aneurysm. Low-level laser irradiation (LLLI) promotes wound healing. However, its effect on smooth muscle cells (SMCs), a central player in these responses, has not been established. The current study was designed to determine the effects of LLLI on arterial SMC proliferation, inflammatory markers, and matrix proteins. Study Design/Materials And MethODS: Porcine primary aortic SMCs were irradiated with a 780 nm laser diode (1 and 2 J/cm(2)). Trypan blue exclusion assay, immunofluorescent staining for collagen I and III, Sircol assay, gelatin zymography, and RT-PCR were used to monitor proliferation; collagen trihelix formation; collagen synthesis; matrix metalloproteinase-2 (MMP-2) activity, and gene expression of MMP-1, MMP-2, tissue inhibitor of MMP-1 (TIMP-1), TIMP-2, and IL-1-beta, respectively. Results: LLLI-increased SMC proliferation by 16 and 22% (1 and 2 J/cm(2), respectively) compared to non-irradiated cells (P<0.01 and P<0.0005). Immediately after LLLI, trihelices of collagen I and III appeared as perinuclear fluorescent rings. Collagen synthesis was increased twofold (2 days after LLLI: 14.3+/-3.5 microg, nonirradiated control: 6.6+/-0.7 microg, and TGF-beta stimulated control: 7.1+/-1.2 microg, P<0.05), MMP-2 activity after LLLI was augmented (over non-irradiated control) by 66+/-18% (2 J/cm(2); P<0.05), and MMP-1 gene expression upregulated. However, TIMP-2 was upregulated, and MMP-2 gene expression downregulated. IL-1-beta gene expression was reduced. Conclusions: LLLI stimulates SMC proliferation, stimulates collagen synthesis, modulates the equilibrium between regulatory matrix remodeling enzymes, and inhibits pro-inflammatory IL-1-beta gene expression. These findings may be of therapeutic relevance for arterial diseases such as aneurysm where SMC depletion, weakened extracellular matrix, and an increase in pro-inflammatory markers are major pathologic components. J Photochem Photobiol B. 2006 Nov 17; [Epub ahead of print] Evaluation of mitochondrial respiratory chain activity in wound healing by low-level laser therapy Silveira PC, Streck EL, Pinho RA Laser therapy is used in many biomedical sciences to promote tissue regeneration. Many studies involving low-level laser therapy have shown that the healing process is enhanced by such therapy. In this work, we evaluated mitochondrial respiratory chain complexes II and IV and succinate dehydrogenase activities in wounds after irradiation with low-level laser. The animals were divided into two groups: group 1, the animals had no local nor systemic treatment and were considered as control wounds; group 2, the wounds were treated immediately after they were made and every day after with a low level laser (AsGa, wavelength of 904nm) for 10 days. The results showed that low-level laser therapy improved wound healing. Besides, our results showed that low-level laser therapy significantly increased the activities of complexes II and IV but did not affect succinate dehydrogenase activity. These findings are in accordance to other works, where cytochrome c oxidase (complex IV) seems to be activated by low-level laser therapy. Besides, we showed, for the first time, that complex II activity was also activated. More studies are being carried out in order to evaluate other mitochondrial enzymes activities after different doses and irradiation time of low-level laser. Photomed Laser Surg. 2006 Dec;24(6):705-14 Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts Hawkins D, Abrahamse H Objective: This study aimed to establish the behavior of wounded human skin fibroblasts (HSF) after heliumneon (HeNe) (632.8 nm) laser irradiation using one, two, or three exposures of different doses, namely, 2.5, 5.0, or 16.0 J/cm(2) on each day for 2 consecutive days. Background Data: Low-level laser therapy (LLLT) is a form of phototherapy used to promote wound healing in different clinical conditions. LLLT at than adequate wavelength, intensity, and dose can accelerate tissue repair. However, there is still conflicting information about the effect of multiple irradiations on the cellular responses of wounded cells. Methods: Cellular responses to HeNe laser irradiation were evaluated by measuring changes in cell morphology, cell viability, cell proliferation, and damage caused by multiple irradiations. Results: A single dose of 5.0 J/cm(2), and two or three doses of 2.5 J/cm(2) had a stimulatory or positive effect on wounded fibroblasts with an increase in cell migration and cell proliferation while maintaining cell viability, but without causing additional stress or damage to the cells. Multiple exposures at higher doses (16 J/cm(2)) caused additional stress, which reduces cell migration, cell viability, and ATP activity, and inhibits cell proliferation. Conclusion: The results show that the correct energy density or fluence (J/cm(2)) and number of exposures can stimulate cellular responses of wounded fibroblasts and promote cell migration and cell proliferation by stimulating mitochondrial activity and maintaining viability without causing additional stress or damage to the wounded cells. Results indicate that the cumulative effect of lower doses (2.5 or 5 J/cm(2)) determines the stimulatory effect, while multiple exposures at higher doses (16 J/cm(2)) result in an inhibitory effect with more damage. J Photochem Photobiol B. 2007 Feb 1;86(2):87-96. Epub 2006 Oct 9 Ultrastructural and autoradiographical analysis show a faster skin repair in He-Ne laser-treated wounds de Araujo CE, Ribeiro MS, Favaro R, Zezell DM, Zorn TM There are evidences that low-intensity red laser radiation is capable to accelerate wound healing. Nowadays, this therapy has been gradually introduced in clinical practice although mechanisms underlying laser effects are poorly understood. To better understand the photobiological effects of laser radiation, this study investigated by electron microscopy, immunohistochemistry and autoradiography the morphological and functional features of irradiated and none irradiated injured mice skin. Full-thickness skin lesions were created on the back of mice and irradiated on days 1, 5, 8, 12, and 15 postwounding with a He-Ne laser (lambda=632.8nm), dose 1J/cm(2), exposure time 3min. Non-irradiated lesions were used as a control. The mice were inoculated with (3)Hproline and sacrificed one hour after on the 8th, 15th and 22nd days to histological and radioautographical analysis. The irradiated-lesions showed a faster reepithelization compared with control lesions. The irradiated dermis contained a higher number of activated fibroblasts compared to control group and, most of them showed several cytoplasmic collagen-containing phagosomes. In irradiated-lesions, smooth muscle alpha-actin positive cells predominated, which correspond to a higher number of myofibroblasts observed in the electron microscope. Moreover, laser radiation reduced the local inflammation and appears to influence the organization of collagen fibrils in the repairing areas. Quantitative autoradiography showed that the incorporation of (3)H proline was significantly higher in irradiated-dermis on the 15th day post-wounding (p<0.05). These results suggest that laser radiation may accelerate cutaneous wound healing in a murine model. Photomed Laser Surg. 2007 Apr;25(2):102-6 Photobiomodulation on the angiogenesis of skin wounds in rats using different light sources Corazza AV, Jorge J, Kurachi C, Bagnato VS Objective: The aim of this study was to compare the angiogenic effects of laser and light-emitting diode (LED) illumination on wounds induced in rats, with varied fluence. Background Data: The LED is an alternative light source that accelerates wound healing, and its efficiency concerning the angiogenic effect was compared to low-level laser therapy (LLLT). Methods: The experimental model consisted of a circular wound inflicted on the quadriceps of 120 rats, using a 15-mm-diameter "punch." Animals were divided randomly into five groups: two groups of laser, with dosages of 5 and 20 J/cm(2), respectively, two groups of LED, also with dosages of 5 and 20 J/cm(2), and a control group. Six hours after wound infliction, the treated groups received the diverse applications accordingly and were irradiated every 24 h. Angiogenesis was studied through histomorphometry on days 3, 7, 14, and 21 after the wounds were inflicted. Results: On days 3, 7, and 14, the proliferation of blood vessels in all irradiated groups was superior in comparison to those of the control group (p < 0.05). Treatment with fluence of 5 J/cm(2) was better than the laser group with 20 J/cm(2) on day 21. Conclusion: Red LLLT and LED demonstrated expressive results in angiogenesis. Light coherence was shown not to be essential to angiogenesis. However, further studies are needed in order to investigate the photobiomodulatory effects of LED in relation to LLLT in various biological tissues. Wound Repair Regen. 2007 Nov-Dec;15(6):866-74 Activation of latent TGF-beta1 by low-power laser in vitro correlates with increased TGF-beta1 levels in laser-enhanced oral wound healing Arany PR, Nayak RS, Hallikerimath S, Limaye AM, Kale AD, Kondaiah P The term Laser "Photobiomodulation" was coined to encompass the pleiotropic effects of low-power lasers on biological processes. The purpose of this study was to investigate whether transforming growth factor (TGF)-beta had a role in mediating the biological effects of low-power far-infrared laser irradiation. We assayed for in vitro activation using various biological forms of cell-secreted, recombinant, and serum latent TGF-beta using the p3TP reporter and enzyme-linked immunosorbent assays. We demonstrate here that low-power lasers are capable of activating latent TGF-beta1 and -beta3 in vitro and, further, that it is capable of "priming" these complexes, making them more amenable to physiological activation present in the healing milieu. Using an in vivo oral tooth extraction-healing model, we observed an increased TGF-beta1, but not beta3, expression by immunohistochemistry immediately following laser irradiation while TGFbeta3 expression was increased after 14 days, concomitant with an increased inflammatory infiltrate. All comparisons were performed between laser-irradiated wounds and nonirradiated wounds in each subject essentially using them as their own control (paired T-test p<0.05). Low-power laser irradiation is capable of activating the latent TGF-beta1 complex in vitro and its expression pattern in vivo suggests that TGFbeta play a central role in mediating the accelerated healing response. J Wound Ostomy Continence Nurs. 2008 Jan-Feb;35(1):113-5; discussion 116-7 Light therapy and advanced wound care for a neuropathic plantar ulcer on a Charcot foot Sutterfield R Light therapy is a relatively novel modality in wound care. I used a light-emitting diode (LED) and superluminous diode (SLD) to deliver low-intensity laser light as an adjunctive treatment to a patient with a chronic diabetic foot ulcer. Standard treatment of conservative sharp debridement, off-loading, bioburden management, and advanced dressings was delivered in a WOC clinic setting. This combination of therapies resulted in closure of the neuropathic plantar ulcer within 8 weeks. Photomed Laser Surg. 2008 Feb;26(1):47-54 Effectiveness of laser photobiomodulation at 660 or 780 nanometers on the repair of third-degree burns in diabetic rats Meireles GC, Santos JN, Chagas PO, Moura AP, Pinheiro AL Objective: The aim of this investigation was to compare by light microscopy the effects of laser photobiomodulation (LPBM) at lambda = 660 nm and lambda = 780 nm on thirddegree burns in diabetic Wistar rats. Background Data: Burns are severe injuries that result in fluid loss, tissue destruction, infection, and shock, that may result in death. Diabetes is a disease that reduces the body's ability to heal properly. LPBM has been suggested as an effective method of improving wound healing. Materials And Methods: A third-degree burn measuring 1.5 x 1.5 cm was created in the dorsum of each of 55 animals, and they were divided into three groups that were or were not treated with LPBM (lambda = 660 nm or lambda = 780 nm, 35 mW, varphi = 2 mm, 20 J/cm(2)). The treatments were started immediately post-burn at four points within the burned area (5 J/cm(2)) and were repeated at 24-hour intervals over 21 d. The animals were humanely killed after 3, 5, 7, 14, and 21 d by an overdose of intraperitoneal general anesthetic. The specimens were routinely cut and stained and analyzed by light microscopy. Results: We found that healing in the animals receiving 660-nm laser energy was more apparent at early stages, with positive effects on inflammation, the amount and quality of granulation tissue, fibroblast proliferation, and on collagen deposition and organization. Epithelialization and local microcirculation were also positively affected by the treatment. Conclusion: The use of 780-nm laser energy was not as effective as 660-nm energy, but it had positive effects at early stages on the onset and development of inflammation. At the end of the experimental period the primary effect seen was on the amount and quality of the granulation tissue. The 660-nm laser at 20 J/cm(2), when used on a daily basis, was more effective than the 780-nm laser for improving the healing of thirddegree burns in the diabetic rats beginning at the early stages post-burn. Photomed Laser Surg. 2008 Apr;26(2):159-66 A comparative study of the effects of laser photobiomodulation on the healing of third-degree burns: a histological study in rats Meirelles GC, Santos JN, Chagas PO, Moura AP, Pinheiro AL Objective: The aim of this investigation was to compare by light microscopy the effects of laser photobiomodulation at wavelengths of 660 and 780 nm on third-degree burns in Wistar rats. Background Data: Burns are severe injuries that result in the loss of fluid and destruction of tissue, infection, and shock that may result in death. Laser energy has been suggested as an effective method to improve wound healing. Materials And Methods: Fifty-five animals were used in this study. A third-degree burn measuring 1.5 x 1.5 cm was created on the dorsum of each animal. The animals were divided into three subgroups according the type of laser photobiomodulation they received (wavelength of 660 or 780 nm, 35 mW, theta = 2 mm, and 20 J/cm2). In the animals receiving treatment, it was begun immediately post-burn at four points around the burn (5 J/cm2) and repeated at 24-h intervals for 21 d. The animals were humanely killed after 3, 5, 7, 14, and 21 d by an intraperitoneal overdose of general anesthetic. The specimens were routinely cut and stained, and then were analyzed by light microscopy. Results: The results showed more deposition of collagen fibers, larger amounts of granulation tissue, less edema, a more vigorous inflammatory reaction, and increased revascularization on all laser-treated animals. These features were more evident at early stages when the 660-nm laser was used, and were more evident throughout the experimental period for the animals receiving 780-nm laser therapy. Conclusion: We concluded that laser photobiomodulation using both wavelengths improved healing of third-degree burns on Wistar rats. Photomed Laser Surg. 2008 Aug;26(4):289-99 The use of light photobiomodulation on the treatment of second-degree burns: a histological study of a rodent model Oliveira PC, Meireles GC, dos Santos NR, de Carvalho CM, de Souza AP, dos Santos JN, Pinheiro AL Objective: The aim of this investigation was to compare, by light microscopy, the effects of the use of laser photobiomodulation (LPBM) and polarized light (PL) on second-degree burns on rodents. Background Data: Burns are severe injuries that result in the loss of tissue fluids, destruction of tissues, infection, and shock. With severe and widespread third-degree burns death may occur. Several light sources have been suggested as being effective for improving wound healing. Materials And Methods: Forty five rats were used in this study. A second-degree burn was created on the dorsum of each animal, and the animals were divided into four groups: PL (400-2000 nm, 40 mW, 2.4 J/cm(2)/min); LPBM-1 (780 nm, 35/40 mW, theta approximately 2 mm, 4 x 5 J/cm(2)); LPBM-2 (660 nm, 35/40 mW, theta approximately 2 mm, 4 x 5 J/cm(2)); and untreated animals acted as controls. The treatment was started immediately post-burn at four points around the burned area (laser: 5 J/cm(2) per site). The illumination with PL was performed according to the manufacturer's instructions. Treatments were repeated at 24-h intervals for 7 d. The animals were sacrifice at 3, 5, and 7 d post-burn. The specimens were routinely cut and stained and analyzed by light microscopy using hematoxylin and eosin and Sirius red. Results: The analysis of the results demonstrated that the damaged tissue was able to efficiently absorb and process the light at all tested wavelengths. LPBM at 660 nm showed better results at early stages of wound healing. However, the use of 780-nm laser light had beneficial effects throughout the experimental period, with the animals growing newly-formed tissue similar to normal dermis. Conclusion: Despite our findings that the use of both types of light energy improved the healing of second-degree burns at the early stages, long-term assessment is needed to verify if this improvement will influence the final results of treatment. J Photochem Photobiol B. 2008 Sep 18;92(3):144-52. Epub 2008 Jul 7 Influence of laser photobiomodulation upon connective tissue remodeling during wound healing Medrado AP, Soares AP, Santos ET, Reis SR, Andrade ZA The modulation of collagen fibers during experimental skin wound healing was studied in 112 Wistar rats submitted to laser photobiomodulation treatment. A standardized 8mmdiameter wound was made on the dorsal skin of all animals. In half of them, 0.2ml of a silica suspension was injected along the border of the wound in order to enhance collagen deposition and facilitate observation. The others received saline as vehicle. The treatment was carried out by means of laser rays from an aluminum-gallium arsenide diode semiconductor with 9mW applied every other day (total dose=4J/cm2) on the borders of the wound. Tissue sections obtained from four experimental groups representing sham-irradiated animals, laser, silica and the association of both, were studied after 3, 7, 10, 15, 20, 30 and 60 days from the laser application. The wounded skin area was surgically removed and submitted to histological, immunohistochemical, ultrastructural, and immunofluorescent studies. Besides the degree and arrangement of collagen fibers and of their isotypes, the degree of edema, the presence of several cell types especially pericytes and myofibroblasts, were described and measured. The observation of Sirius-red stained slides under polarized microscopy revealed to be of great help during the morphological analysis of the collagen tissue dynamic changes. It was demonstrated that laser application was responsible for edema regression and a diminution in the number of inflammatory cells (p<0.05). An evident increase in the number of actin-positive cells was observed in the laser-treated wounds. Collagen deposition was less than expected in silica-treated wounds, and laser treatment contributed to its better differentiation and modulation in all irradiated groups. Thus, laser photobiomodulation was able to induce several modifications during the cutaneous healing process, especially in favoring newly-formed collagen fibers to be better organized and compactedly disposed. Lasers Surg Med. 2008 Sep;40(7):509-14 A possible mechanism for visible light-induced wound healing Lipovsky A, Nitzan Y, Lubart R Background And Objectives: Chronic wounds resistant to conventional therapy have been treated successfully with low energy lasers and light emitting diodes (LEDs) in the visible and near IR region. It has been proposed that production of low level reactive oxygen species (ROS) following illumination is the first step of photobiomodulation. It was also shown that white light (400-800 nm) has similar stimulatory effects as lasers and LEDs. ROS at higher levels are toxic to cells and bacteria. Study Design/Materials And Methods: In the present study, we examined the phototoxicity of broadband (400-800 nm, 120 J/cm(2)) visible light on the survival of several pathogenic bacteria: Staphylococcus aureus 195, Pseudomonas aeruginosa 1316, Escherichia coli 1313, and Serratia marcescens. These bacteria were chosen due to their high prevalence in infected wounds. The survival of bacterial cells following illumination was monitored by counting the number of colony forming units before and after exposure to light. Results: Illumination with white light, 120 J/cm(2), caused a reduction of 62%, 83%, and 56% in the colony count of E. coli 1313, S. aureus 195 and S. marcescens, respectively, though no reduction in the viability of P. aeruginosa 1316 was demonstrated. The phototoxic effect was found to involve induction of ROS production by the bacteria. It was also found that illumination of S. aureus 195 and E. coli 1313 in the presence of pyocyanin, known to be secreted by P. aeruginosa, had a stronger bactericidal effect compared to illumination alone. Conclusion: Visible light at high intensity can kill bacteria in infected wounds. Thus, illumination of infected wounds with intense visible light, prior to low intensity illumination for stimulating wound closure, may reduce infection and promote healing. J Biochem Mol Toxicol. 2009 Jan-Feb;23(1):1-8 Effects of low-level light therapy on hepatic antioxidant defense in acute and chronic diabetic rats Lim J, Ali ZM, Sanders RA, Snyder AC, Eells JT, Henshel DS, Watkins JB 3rd Diabetes causes oxidative stress in the liver and other tissues prone to complications. Photobiomodulation by near infrared light (670 nm) has been shown to accelerate diabetic wound healing, improve recovery from oxidative injury in the kidney, and attenuate degeneration in retina and optic nerve. The present study tested the hypothesis that 670 nm photobiomodulation, a low-level light therapy, would attenuate oxidative stress and enhance the antioxidant protection system in the liver of a model of type I diabetes. Male Wistar rats were made diabetic with streptozotocin (50 mg/kg, ip) then exposed to 670 nm light (9 J/cm(2)) once per day for 18 days (acute) or 14 weeks (chronic). Livers were harvested, flash frozen, and then assayed for markers of oxidative stress. Light treatment was ineffective as an antioxidant therapy in chronic diabetes, but light treatment for 18 days in acutely diabetic rats resulted in the normalization of hepatic glutathione reductase and superoxide dismutase activities and a significant increase in glutathione peroxidase and glutathione-S transferase activities. The results of this study suggest that 670 nm photobiomodulation may reduce, at least in part, acute hepatic oxidative stress by enhancing the antioxidant defense system in the diabetic rat model. Photomed Laser Surg. 2009 Feb;27(1):49-55 Immunohistochemical assessment of myofibroblasts and lymphoid cells during wound healing in rats subjected to laser photobiomodulation at 660 nm Ribeiro MA, Albuquerque RL Jr, Ramalho LM, Pinheiro AL, Bonjardim LR, Da Cunha SS Objective: The goal of this study was to assess the biomodulatory effect of low-level laser therapy (LLLT) on myofibroblasts and T and B cells during wound healing. Background Data: Phtotobiomodulation using LLLT has been extensively applied to improve wound healing. Materials And Methods: Standardized artificial surgical wounds were made on the backs of 24 male rats. Half of them underwent LLLT (20 J/cm(2) at 660 nm delivered for 7 d. At 8 and 14 d post-surgery the healing wounds were removed and immunohistochemical analysis of myofibroblasts, T cells, and B cells was carried out. The mean of each cell subset was calculated and compared to one another using two-way analysis of variance (ANOVA) and Tukey's test. Results: The average number of myofibroblasts was statistically significantly higher in the irradiated group than in the non-irradiated group on the eighth (p = 0.001) but not the 14th (p = 0.555) day. B and T cells were significantly more conspicuous in the irradiated group on both the eighth (p = 0.004 and 0.02, respectively) and 14th days (p = 0.04 and 0.03, respectively). Conclusions: Our results suggest that LLLT facilitates myofibroblastic differentiation during the early stages of the cicatricial repair process. Furthermore, LLLT also appears to modulate the inflammatory response by downregulating lymphocytic proliferation during the wound healing process. Lasers Med Sci. 2009 Mar;24(2):234-40. Epub 2008 Apr 17 Bone repair following bone grafting hydroxyapatite guided bone regeneration and infra-red laser photobiomodulation: a histological study in a rodent model. Pinheiro AL, Martinez Gerbi ME, de Assis Limeira F Jr, Carneiro Ponzi EA, Marques AM, Carvalho CM, de Carneiro Santos R, Oliveira PC, Nóia M, Ramalho LM The aim of the investigation was to assess histologically the effect of laser photobiomodulation (LPBM) on a repair of defects surgically created in the femurs of rats. Forty-five Wistar rats were divided into four groups: group I (control); group II (LPBM); group III (hydroxyapatite guided bone regeneration; HA GBR); group IV (HA GBR LPBM). The animals in the irradiated groups were subjected to the first irradiation immediately after surgery, and it was repeated every day for 2 weeks. The animals were killed 15 days, 21 days and 30 days after surgery. When the groups irradiated with implant and membrane were compared, it was observed that the repair of the defects submitted to LPBM was also processed faster, starting from the 15th day. At the 30th day, the level of repair of the defects was similar in the irradiated groups and those not irradiated. New bone formation was seen inside the cavity, probably by the osteoconduction of the implant, and, in the irradiated groups, this new bone formation was incremental. The present preliminary data seem to suggest that LPMB therapy might have a positive effect upon early wound healing of bone defects treated with a combination of HA and GBR. Photochem Photobiol. 2009 Jul-Aug;85(4):987-96. Epub 2009 Feb 13 Mitochondrial responses of normal and injured human skin fibroblasts following low level laser irradiation--an in vitro study Zungu IL, Hawkins Evans D, Abrahamse H Laser irradiation has proved to be very efficient in speeding and improving the quality of healing in pathological conditions of diverse etiologies. However, the mechanisms by which the beneficial effects are attained are not clear. Mitochondria are the primary phototargets during irradiation. The study aimed to establish if laser irradiation had an effect on hypoxic and acidotic cells. The study also aimed to use existing information regarding the possible mechanism of action (established in wounded cells) and apply these principles to acidic and hypoxic irradiated cells to determine whether laser has a stimulatory or inhibitory effect. Cell cultures were modified to simulate conditions of hypoxia (hypoxic gas mixture 95% N2 and 5% O2) and acidosis (pH 6.7) whereas the central scratch model was used to simulate a wound. Cells were irradiated with a helium-neon (632.8 nm, 3 mW cm(-2)) laser using 5 or 16 J cm(-2) on days 1 and 4. Mitochondrial responses were measured 1 or 24 h after laser irradiation by assessing changes in mitochondrial membrane potential (MMP), cyclic AMP, intracellular Ca2+ and adenosine triphosphate (ATP) cell viability. Hypoxia and acidosis significantly reduced MMP when compared with normal nonirradiated control cells. Wounded, hypoxic and acidotic cells irradiated with 5 J cm(-2) showed an increase in mitochondrial responses when compared with nonirradiated cells while 16 J cm(-2) showed a significant decrease. The study confirmed that laser irradiation with 5 J cm(-2) stimulated an increase in intracellular Ca2+ which resulted in an increase in MMP, ATP and cAMP, which ultimately results in photobiomodulation to restore homeostasis of injured cells. Indian J Dent Res. 2009 Jul-Sep;20(3):390 Morphological analysis of second-intention wound healing in rats submitted to 16 J/cm 2 lambda 660-nm laser irradiation Gonzaga Ribeiro MA, Cavalcanti de Albuquerque RL, Santos Barreto AL, Moreno de Oliveira VG, Santos TB, Freitas Dantas CD Background And Objectives: Low-level laser therapy (LLLT) has been extensively applied to improve wound healing due to some biostimulatory properties presented by laser arrays apparently able to accelerate the cicatricial repair of soft tissue injuries. However, many controversial results have been reported in the literature, probably as a result of the wide sort of different protocols of photobiomodulation employed in those experiments. The goal of this study was to investigate the effect of a low-dose protocol of LLT on the intensity of the inflammatory response and the pattern of collagen fibers' deposition during second-intention wound healing in rodents. Materials And Methods: Standard-sized wounds were carried out in the back of 24 male rats. Half of them underwent LLLT treatment (16 J/cm 2 ) at 660 nm delivered for 7 days. Eight and 14 days after the wounds were performed, the repairing area was removed and stained in HE and Masson's trichrome, and the inflammatory response, epithelization, and collagen fiber depositions were evaluated. Results: We found that LLLT was able to slightly reduce the intensity of the inflammatory reaction as well as to enhance substantially the epithelization process at both 8 th and 14 th days. In addition, it also appeared to stimulate the deposition of collagen fibers at the final stages of wound healing. Conclusions: The LLLT protocol tested in this study resulted in some improvements in second-intention wound healing in rodents. Indian J Dent Res. 2009 Jul-Sep;20(3):390 Morphological analysis of second-intention wound healing in rats submitted to 16 J/cm 2 lambda 660-nm laser irradiation Gonzaga Ribeiro MA, Cavalcanti de Albuquerque RL, Santos Barreto AL, Moreno de Oliveira VG, Santos TB, Freitas Dantas CD Background And Objectives: Low-level laser therapy (LLLT) has been extensively applied to improve wound healing due to some biostimulatory properties presented by laser arrays apparently able to accelerate the cicatricial repair of soft tissue injuries. However, many controversial results have been reported in the literature, probably as a result of the wide sort of different protocols of photobiomodulation employed in those experiments. The goal of this study was to investigate the effect of a low-dose protocol of LLT on the intensity of the inflammatory response and the pattern of collagen fibers' deposition during second-intention wound healing in rodents. Materials And Methods: Standard-sized wounds were carried out in the back of 24 male rats. Half of them underwent LLLT treatment (16 J/cm 2 ) at 660 nm delivered for 7 days. Eight and 14 days after the wounds were performed, the repairing area was removed and stained in HE and Masson's trichrome, and the inflammatory response, epithelization, and collagen fiber depositions were evaluated. Results: We found that LLLT was able to slightly reduce the intensity of the inflammatory reaction as well as to enhance substantially the epithelization process at both 8 th and 14 th days. In addition, it also appeared to stimulate the deposition of collagen fibers at the final stages of wound healing. Conclusions: The LLLT protocol tested in this study resulted in some improvements in second-intention wound healing in rodents. Dermatol Ther. 2009 Nov;22 Suppl 1:S8-15 Fractional CO2 laser: a novel therapeutic device upon photobiomodulation of tissue remodeling and cytokine pathway of tissue repair Prignano F, Campolmi P, Bonan P, Ricceri F, Cannarozzo G, Troiano M, Lotti T Minimally ablative fractional laser devices have gained acceptance as a preferred method for skin resurfacing. Notable improvements in facial rhytides, photodamage, acne scarring, and skin laxity have been reported. The aim of the present work was to compare how different CO(2) laser fluences, by modulating the secretory pathway of cytokines, are able to influence the wound-healing process, and how these fluences are associated with different clinical results. Eighteen patients, all with photodamaged skin, were treated using a fractional CO(2) laser (SmartXide DOT, Deka M.E.L.A., Florence, Italy) with varying laser fluencies (2.07, 2.77, and 4.15 J/cm(2)). An immunocytochemical study was performed at defined end points in order to obtain information about specific cytokines of the microenvironment before and after treatment. The secretory pathway of cytokines changed depending on the re-epithelization and the different laser fluences. Different but significant improvements in wrinkles, skin texture, and hyperpigmentation were definitely obtained when using 2.07, 2.77, and 4.15 J/cm(2), indicating fractional CO(2) laser as a valuable tool in photorejuvenation with good clinical results, rapid downtime, and an excellent safety profile. J Plast Reconstr Aesthet Surg. 2009 Dec;62(12):1684-7. Epub 2008 Nov 1 The use of argon beam coagulation in pressure sore reconstruction Buck DW 2nd, Lewis VL Jr Purpose: Pressure sores are a significant source of physical and financial burden for debilitated patients. When conservative measures fail, surgical reconstruction with myocutaneous flaps may be the last hope for cure and/or improved quality of life in these patients. Adequate haemostasis is an integral component of these reconstructive procedures, as bleeding and haematoma formation can lead to increased morbidity. This study was designed to investigate the use of argon beam coagulation in patients undergoing bony debridement and subsequent pressure sore reconstruction with myocutaneous flaps. Methods: The clinical records of 34 patients undergoing pressure sore reconstruction with the use of argon beam coagulation from 2004 to 2006 at an academic institution were reviewed and outcomes were assessed. Results: Reconstruction was performed by a single surgeon on 34 patients (31 men, three women; mean age 41+/-15 years), with a total of 41 pressure sores. Thirteen (32.5%) patients had evidence of osteomyelitis preoperatively and five (12.5%) had previous coccygectomies secondary to infection. Twenty-six (65%) of the pressure sores were treated with hamstring V-Y musculocutaneous flaps, 10 (25%) with gluteal flaps, and four (10%) with tensor fascia lata flaps. Overall, suture line dehiscence occurred in six (15%) cases, flap failure and pressure sore recurrence occurred in six (15%) cases, an abscess developed in one (2.5%) case, and a sinus tract with a superficial wound developed in one (2.5%) case. There were no complications related to haemostasis, including excessive bleeding or haematoma formation. Conclusions: Argon beam coagulation is an efficacious tool for achieving adequate haemostasis during pressure sore reconstruction, particularly when significant bony debridement is involved. The use of argon beam coagulation does not result in an increased complication or recurrence rate when compared with conventional electrocautery methods. Photomed Laser Surg. 2010 Feb;28(1):81-90 Effects of laser photobiomodulation on cutaneous wounds treated with mitomycin C: a histomorphometric and histological study in a rodent model Santos NR, dos Santos JN, Sobrinho JB, Ramalho LM, Carvalho CM, Soares LG, Pinheiro AL Aim: The aim of the present study was to assess histologically the effect of Laser Photobiomodulation (LPBM) on skin wounds treated with Mitomycin C (MMC). Background Data: Wound healing occurs because of a competitive mechanism between the synthesis and lyses of collagen. Therefore, any factor that increases the lyses or reduces the synthesis of collagen may result in changes in the healing process. MMC is an antineoplastic drug that inhibits fibroblast proliferation, collagen synthesis, and neoangiogenesis. LPBM has been shown to stimulate wound healing, increasing the production of collagen, fibroblastic proliferation, and angiogenesis. Materials And Methods: Forty-eight Wistar rats were randomly distributed into 4 main groups (n = 12): G1--control (G1a--7 d and G1b--14 d); G2--MMC (G2a--7 d and G2b-14 d); G3--MMC + lambda660 nm laser (G3a--7 d and G3b--14 d); and G4--MMC + lambda790 nm laser (G4a--7 d and G4b--14 d). Under general anesthesia, one excisional wound was created on the dorsum of each animal. Two ml of MMC solution was applied to the wound 4 h after surgery for 5 min. LPBM was performed on groups G3 (lambda690 nm; 20 J/cm(2); 30 mW; Phi = 2 mm) and G4 (lambda790 nm; 20 J/cm(2); 40 mW; Phi = 2 mm), starting immediately after the application of the MMC and repeated every other day during the experimental period. Laser light was applied transcutaneously at 4 equidistant points on the wound margin (4 x 5 J/cm(2), 20 J/cm(2)/session). The specimens were routinely cut and processed to wax. The slides were stained with HE and Sirius red. Computerized hystomorphometry was performed. Results: LPBM resulted in reduced inflammation and an increase in both fibroblast proliferation and collagen deposition. Conclusion: The use of LPBM improves wound healing in subjects treated with MMC. Lasers Surg Med. 2010 Apr;42(4):348-52 Visible light induces nitric oxide (NO) formation in sperm and endothelial cells Ankri R, Friedman H, Savion N, Kotev-Emeth S, Breitbart H, Lubart R Background: Visible light-based stimulation using low-intensity lasers, LEDs, and broadband visible light devices has been recently introduced for therapy of human tissues in the absence of exogenous photosensitizers. Nitric oxide (NO) formation might be a potential mechanism for photobiomodulation because it is synthesized in cells by nitric oxide synthase (NOS), which contains both flavin and heme groups that absorb visible light. NO synthesis may also result from increased reactive oxygen species (ROS), which are found in various cell cultures following visible light illumination. NO is mainly known for inducing blood vessel dilation by endothelial cells, and in sperm cells NO is considered as an important agent in acrosome reaction and capacitation process, which are essential for successful fertilization. Purpose: To study NO formation in endothelial and sperm cells following visible light irradiation. Materials And Methods: Sperm and endothelial cells were illuminated with broadband visible light, 400-800 nm, 130 mW/cm(2), for 5 minutes. During illumination, the endothelial cells were incubated in PBS free of Ca(+2) and Mg(+2), and the sperm cells were incubated in NKM buffer, to induce "stress conditions." NO production was quantified by using the Griess reagent which reacts with nitrite in the medium to yield an Azo compound which has an absorption band at 540 nm. Results: Visible light illumination increased NO concentration both in sperm and endothelial cells. Blue light was more effective than red. Light-induced NO occurred only when endothelial cells were incubated in PBS free of Ca(+2) and Mg(+2), and in sperm cells, only when incubated in NKM. Conclusion: Light induces NO formation in endothelial and sperm cells. In endothelial cells, NO formation may explain previous results demonstrating enhanced wound healing and pain relief following illumination. In illuminated sperm cells, NO formation may account for the enhanced fertilization rate. Photomed Laser Surg. 2010 Apr;28(2):251-61 Laser photobiomodulation of wound healing in diabetic and non-diabetic mice: effects in splinted and unsplinted wounds. Chung TY, Peplow PV, Baxter GD Objective: The aim of this investigation was to compare the healing of laser-irradiated and non-irradiated wounds covered by an occlusive dressing in mice. Background Data: Many previous studies of the effects of laser irradiation of experimental wounds in mice and rats did not cover the wounds so that healing occurred mainly by contraction. Healing of covered wounds is slower and mimics more closely wound healing in humans. Materials And Methods: Forty-seven diabetic and twenty non-diabetic mice were used. A single wound (5 mm diameter) was created on the left flank of each animal and covered by Tegaderm HP dressing (Day 1). Wounds were irradiated (660 nm) for 20 s using a lower power (18 mW) or higher power (80 mW) laser starting immediately postwounding for seven consecutive days (0.36 or 1.6 J/day); untreated wounds served as controls. Animals were euthanized on Day 8, 10, or 14. Wound specimens were cut and stained using haematoxylin and eosin, and picrosirius red, and examined by microscopy. Results: Results confirmed that wound healing was impaired in diabetic mice. Analysis of the data demonstrated that Tegaderm HP dressing had retarded contraction (splinted the wounds) in a large proportion of diabetic mice and, to a lesser extent, in non-diabetic mice. Healing of splinted wounds was delayed compared to unsplinted wounds, but laser irradiation (1.6 J/day, 7 days) stimulated healing by re-epithelization and granulation tissue formation. Conclusion: These are the first findings of laser-mediated stimulation of healing in splinted wounds. Further studies are needed to assess the effects of different constellation sets of laser parameters in this wound model. Photomed Laser Surg. 2010 Jun;28(3):291-325 Laser photobiomodulation of wound healing: a review of experimental studies in mouse and rat animal models Peplow PV, Chung TY, Baxter GD Objectives: This investigation reviewed experimental studies of laser irradiation of wound healing in mice and rats published from 2003 to August 2008, respectively, to assess putative stimulatory effects of this treatment. Background: Animal models, including rodents, attempt to reflect human wound healing and associated problems such as dehiscence, ischemia, ulceration, infection, and scarring. They have played a key role in furthering understanding of underlying mechanisms involved in impaired wound healing, and in testing new therapeutic strategies including laser irradiation. Method: Original research papers investigating effects of laser or monochromatic light therapy on wound healing in mice and rats and published from January 2003 to August 2008 were retrieved from library sources, PubMed and Medline databases, reference lists from retrieved papers, and hand searches of relevant journals. Papers were selected for this review with regard to specific inclusion and exclusion criteria. Studies were critically reviewed in terms of study design, methodology, and appropriateness of laser irradiation parameters. Results: The literature search identified eight studies in mice and 39 in rats. A variety of wound models were investigated, including acute-wound, impaired-healing, and chronicwound models. Considerable variation was observed in research design, methodology, and irradiation parameters employed, limiting comparison of research findings between studies. Inadequate reporting of key experimental details, or errors in specification and/or calculation of key irradiation parameters was also found. Evidence from the studies reviewed suggested that use of red or infrared wavelength at a range of dosage parameters (median 4.2 J cm(-2)) results in significant benefits in measured parameters of wound healing. Interestingly, coherence does not seem essential to the photobiomodulatory effects of 'laser' phototherapy. Conclusion: Studies reviewed consistently demonstrated the ability of laser or monochromatic light to photobiomodulate wound healing processes in experimental wounds in rats and mice, and strongly support the case for further controlled research in humans. J Orthop Sci. 2010 Mar;15(2):233-9. Epub 2010 Apr 1 Effect of near-infrared light-emitting diodes on nerve regeneration Ishiguro M, Ikeda K, Tomita K Background: Photobiomodulation by red to near-infrared light-emitting diodes (LEDs) has been reported to accelerate wound healing, attenuate degeneration of an injured optic nerve, and promote tissue growth. The purpose of this study was to investigate the effect of LEDs on nerve regeneration. A histological study as well as a measurement of antioxidation levels in the nerve regeneration chamber fluid was performed. Methods: For the histological study, the bilateral sciatic nerves were transected, and the left proximal stump and the right distal stump were inserted into the opposite ends of a silicone chamber, leaving a 10-mm gap. Light from an LED device (660 nm, 7.5 mW/cm(2) was irradiated for 1 h per day. At 3 weeks after surgery, regenerated tissue was fixed and examined by light microscopy. For the antioxidation assay of chamber fluid, the left sciatic nerve and a 2-mm piece of nerve from the proximal stump were transected and inserted into opposite sides of a silicone chamber leaving a 10-mm gap. LEDs were irradiated using the same parameters as those described in the histological study. At 1, 3, and 7 days after surgery, antioxidation of the chamber fluid was measured using an OXY absorbent test. Results: Nerve regeneration was promoted in the LED group. Antioxidation of the chamber fluid significantly decreased from 3 days to 7 days in the control group. In the LED group, antioxidation levels did not decrease until 7 days. Conclusions: Chamber fluid is produced from nerve stumps after nerve injury. This fluid contains neurotrophic factors that may accelerate axonal growth. Red to near-infrared LEDs have been shown to promote mitochondrial oxidative metabolism. In this study, LED irradiation improved nerve regeneration and increased antioxidation levels in the chamber fluid. Therefore, we propose that antioxidation induced by LEDs may be conducive to nerve regeneration. Photomed Laser Surg. 2010 Aug;28 Suppl 1:S3-40 Laser photobiomodulation of proliferation of cells in culture: a review of human and animal studies Peplow PV, Chung TY, Baxter GD Aim: The aim of this article was to review experimental studies of la irradiation of human and animal cells in culture to assess the photobiomodulatory effects of such irradiation. Background: Previous studies have shown that various types of cells respond differently to laser irradiation, depending on irradiation parameters. Cellular outcomes measured or examined include cell numbers, cell viability, and ultrastructural features. A review of these studies may provide a further insight into the clinical effects brought about by laser light on cells and tissues, including laser effects in wound healing and repair of nerves and skeletal muscle after injury. Methods: A systematic review was completed of original research articles investigating the effects of laser therapy on human and animal cells in culture (January 2002 to September 2009). Relevant articles were primarily sourced from PubMed and Medline by using EndNote X1, and from secondary searches. Search terms were "cell proliferation," "laser therapy," "laser irradiation," "laser phototherapy," and "phototherapy." Results: In total, 46 relevant articles were included in the review, comprising work completed on a variety of cell types. Although results consistently demonstrated the potential of laser irradiation to affect cellular proliferation in a wavelength- and dosagedependent manner, the relevance of other key irradiation parameters, such as irradiance, to such effects remained unclear. Conclusions: Findings from studies of cells in culture clearly demonstrate the ability of laser irradiation to modulate (typically stimulate) cellular proliferation. The relevance of some irradiation parameters remains occult and represents an important area for further research. Photomed Laser Surg. 2011 Jan;29(1):11-7. Epub 2010 Aug 11 Influence of laser photobiomodulation on collagen IV during skeletal muscle tissue remodeling after injury in rats Baptista J, Martins MD, Pavesi VC, Bussadori SK, Fernandes KP, Pinto Júnior Ddos S, Ferrari RA Objective: The aim of the present study was to determine the effect of GaAlAs low-level laser therapy (LLLT) on collagen IV remodeling of the tibialis anterior (TA) muscle in rats after cryolesion. Background: Considerable interest exists in skeletal muscle regeneration in situations such as repair after exercise-induced muscle injury, after muscle transplantation, in muscular dystrophy, exercise-induced muscle injury, and the recovery of strength after atrophy due to disuse. A number of studies have demonstrated the potential of LLLT in facilitating the muscle-healing process; however, no consensus is found in the literature regarding the best laser-irradiation parameters. Methods: Adult male Wistar rats (n = 45) were used and randomly divided into three groups: control (n = 5); nontreated cryolesioned group (n = 20), and LLLT-cryolesioned group (n = 20). The cryolesioned groups were analyzed at 1, 7, 14, and 21 days after the injury procedure. Laser irradiation was performed 3 times per week on the injured region by using the GaAlAs laser (660 nm; beam spot of 0.04 cm(2), output power of 20 mW, power density of 500 mW/cm(2), and energy density of 5 J/cm(2), for 10 sec). The muscles were removed, frozen, cryosectioned, and then stained with hematoxylin-eosin for the visualization of general morphology or used for immunohistochemical analysis of collagen IV. Results: It was demonstrated that LLLT promotes an increase in collagen IV immunolabeling in skeletal muscle in the first 7 days after acute trauma caused by cryoinjury, but does not modify the duration of the tissue-repair process. Even with LLLT, the injured muscle tissue needs ∼21 days to achieve the same state of organization as that in the noninjured muscle. Conclusion: The collagen IV content is modulated in regenerating skeletal muscle under LLLT, which might be associated with better tissue outcome, although the histologic analysis did not detect tissue improvement in the LLLT group. Photomed Laser Surg. 2010 Oct;28(5):639-46. Epub 2010 Oct 9 Influence of laser (λ670 nm) and dexamethasone on the chronology of cutaneous repair Marchionni AM, Medrado AP, Silva TM, Fracassi LD, Pinheiro AL, Reis SR Objective: This study aimed to assess the effect of LLLT associated with and without dexamethasone on inflammation and wound healing in cutaneous surgical wounds. Background: Limited studies are directed at the possible interference of laser photobiomodulation on the formation of myofibroblasts, associated with an antiinflammatory drug. Methods And Materials: Standard skin wounds were performed on 80 Wistar rats, distributed into four groups: no treatment (sham group), laser only (λ670 nm, 9 mW, 0.031 W/cm(2), 4 J/cm(2), single dose after surgery), dexamethasone only (2 mg/kg 1 h before surgery), and laser with dexamethasone. Tissue was examined histologically to evaluate edema, presence of polymorphonuclear, mononuclear cells, and collagen. The analysis of myofibroblasts was assessed by immunohistochemistry and transmission electron microscopy. The intensity was rated semiquantitatively. Results: The results showed that laser and dexamethasone acted in a similar pattern to reduce acute inflammation. Collagen synthesis and myofibroblasts were more intense in the laser group (p = 0.048), whereas animals treated with dexamethasone showed lower results for these variables. In a combination of therapies, the synthesis of collagen and actin and desmin-positive cells was less than laser group. Conclusions: Laser was effective in reducing swelling and polymorphonuclear cells and accelerated tissue repair, even in the presence of dexamethasone. Photomed Laser Surg. 2010 Oct;28(5):597-602 Comparative study of the effects of gallium-aluminum-arsenide laser photobiomodulation and healing oil on skin wounds in wistar rats: a histomorphometric study Gonçalves RV, Novaes RD, Matta SL, Benevides GP, Faria FR, Pinto MV Objective: The present study compared the effects of gallium-aluminum-arsenide diode laser and healing oil on fibroblasts, blood vessels, and collagen maturation of skin wounds in Wistar rats. Materials And Methods: Twenty-four male rats weighing 325 ± 27 g were used. Five wounds, 12 mm in diameter, were made on the animals' backs. The rats were randomly divided into four groups with six animals in each group. Control group: saline solution; L30 group: 30 J/cm(2) laser; L60 group: 60 J/cm(2) laser; Oil group: healing oil. Histomorphometric analysis was performed on the scar tissue removed from the different wounds every 4 d for 20 d. Results: On day 4, there were significantly more fibroblasts in the wounds treated with the laser and the healing oil compared to the controls. On day 8, there were significantly more fibroblasts in the oil group compared to the L30 and L60 groups. On the same day, the quantity of vessels was significantly greater in the L60 group compared to the other groups. On day 16, there was a significant increase in the number of blood vessels in the wounds treated with the 60 J/cm(2) laser compared to the other groups. Analysis of the collagen maturation index throughout the experiment showed significantly higher values in the L60 group compared to the other groups at all time points. Conclusion: The healing oil exerted a greater effect on fibroblast proliferation, whereas the 60 J/cm(2) laser was more effective in stimulating angiogenesis and scar-tissue maturation. Photomed Laser Surg. 2011 Apr;29(4):233-7. Epub 2010 Dec 23 Effect of photobiomodulation on vinblastine-poisoned murine HERS cells Hodgson BD, Pyszka B, Henry MM, Buchmann E, Whelan HT Objective: The aim of this study was to investigate the effect of near-infrared (NIR) photobiomodulation on the proliferation and glutathione levels in murine Hertwig's epithelial root sheath (HERS) cells after poisoning with vinblastine. Background: Photobiomodulation has been shown to improve wound healing in a number of animal models. There have been no studies on the effect of photobiomodulation on cancer-related chemotherapy injury to the cells that initiate tooth root growth. Materials And Methods: Control groups consisted of murine HERS cells without vinblastine (VB-) and cells with vinblastine at 10, 20, and 30 ng/mL (VB10, VB20, and VB30). Experimental groups consisted of these same groups with light therapy (VB-L, VB10L, VB20L, and VB30L). The cells were exposed to vinblastine for 1 h. Photobiomodulation consisted of a 75-cm(2) gallium-aluminum-arsenide light-emitting diode (LED) array at an energy density of 12.8 J/cm(2), delivered with 50 mW/cm(2) power over 256 s. Results: Vinblastine alone significantly decreased HERS cell proliferation and glutathione levels at all concentrations (VB10 [-55%, p < 1.0 × 10(-8)]; VB20 [-72%, p < 1.0 × 10(9)]; VB30 [-80%, p < 1.0 × 10(-10)]; and VB10 [-36%, p < 0.0001]; VB20 [-49%, p < 1.0 × 10(-6)]; VB30 [-53%, p < 1.0 × 10(-7)] respectively). Photobiomodulation significantly increased cell proliferation at all levels of vinblastine exposure (VB10L [+50%, p < 0.0001]; VB20L [+45%, p < 0.05]; VB30 [+39%, p < 0.05]) but not of the control (+22%, p = 0.063). The photobiomodulation significantly increased glutathione production in all concentrations of vinblastine except 20 ng/mL (VB10L [+39%, p = 0.007]; VB20L [+19%, p = 0.087]; VB30 [+14%, p = 0.025]) and the control (+12%, p = 0.13). Conclusions: Photobiomodulation demonstrated an improvement in proliferation and glutathione levels in vinblastine-poisoned murine HERS cells. PM R. 2010 Dec;2(12 Suppl 2):S292-305 Role of low-level laser therapy in neurorehabilitation Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR This year marks the 50th anniversary of the discovery of the laser. The development of lasers for medical use, which became known as low-level laser therapy (LLLT) or photobiomodulation, followed in 1967. In recent years, LLLT has become an increasingly mainstream modality, especially in the areas of physical medicine and rehabilitation. At first used mainly for wound healing and pain relief, the medical applications of LLLT have broadened to include diseases such as stroke, myocardial infarction, and degenerative or traumatic brain disorders. This review will cover the mechanisms of LLLT that operate both on a cellular and a tissue level. Mitochondria are thought to be the principal photoreceptors, and increased adenosine triphosphate, reactive oxygen species, intracellular calcium, and release of nitric oxide are the initial events. Activation of transcription factors then leads to expression of many protective, anti-apoptotic, antioxidant, and pro-proliferation gene products. Animal studies and human clinical trials of LLLT for indications with relevance to neurology, such as stroke, traumatic brain injury, degenerative brain disease, spinal cord injury, and peripheral nerve regeneration, will be covered. J Photochem Photobiol B. 2011 Dec 2;105(3):175-82. Epub 2011 Sep 6 Enhancement of cutaneous immune response to bacterial infection after lowlevel light therapy with 1072 nm infrared light: a preliminary study Lee SY, Seong IW, Kim JS, Cheon KA, Gu SH, Kim HH, Park KH We investigated the photobiomodulation effects of 1072 nm infrared light on the natural immune response involved in anti-bacterial and wound healing processes. Thirty mice infected with MRSA on the skin were divided into two groups. The experimental group was treated with 1072 nm infrared light (irradiance: 20 mW/cm(2), fluence: 12 J/cm(2) for 10 min) at 2, 4, 8, 12, 24 h, 3 and 5 days after inoculation and the control group with sham light. Serial changes of the mRNA levels of TLR2, IL-1β, TNF-α, IL-6, iNOS, MCP-1, TGF-β, bFGF and VEGF were studied by real time RT-PCR and those of the expression level of VEGF, bFGF, TGF-β and NF-κB by immunohistochemistry. The mRNA levels of the cytokines involved in the early phase of anti-bacterial immune response (IL-1β, TNF-α, IL-6, MCP-1) increased significantly in the 1072 nm group, peaking between 12 and 24 h post-inoculation. These levels normalized after 3-5 days. Immunohistochemistry revealed a notably stronger expression of VEGF in the 1072 nm group from 8-h post-inoculation to 5-day post-inoculation. We concluded that 1072 nm infrared light had a photobiomodulation effect which resulted in an enhanced biological immune response to the bacterial infection by MRSA and also increased the expression of VEGF to a significant level. Ann Biomed Eng. 2011 Nov 2. [Epub ahead of print] The Nuts and Bolts of Low-level Laser (Light) Therapy Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR Soon after the discovery of lasers in the 1960s it was realized that laser therapy had the potential to improve wound healing and reduce pain, inflammation and swelling. In recent years the field sometimes known as photobiomodulation has broadened to include light-emitting diodes and other light sources, and the range of wavelengths used now includes many in the red and near infrared. The term "low level laser therapy" or LLLT has become widely recognized and implies the existence of the biphasic dose response or the Arndt-Schulz curve. This review will cover the mechanisms of action of LLLT at a cellular and at a tissular level and will summarize the various light sources and principles of dosimetry that are employed in clinical practice. The range of diseases, injuries, and conditions that can be benefited by LLLT will be summarized with an emphasis on those that have reported randomized controlled clinical trials. Serious life-threatening diseases such as stroke, heart attack, spinal cord injury, and traumatic brain injury may soon be amenable to LLLT therapy.