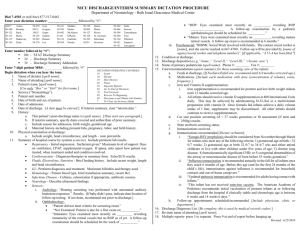
NICU Guidelines for Routine Screening, Testing , Treatment and
advertisement

Guidelines for Routine Screening, Testing, Treatment and Follow-up Neonatal Intensive Care Unit Beth Israel Deaconess Medical Center Newborn Screening Criteria All infants admitted to the NICU Initial Day 3 or D/C date (whichever comes first) Follow-up Day 14 or D/C date (whichever comes first) Week 6 (if birth weight <1500 gms) Week 10 (if birth weight <1500 gms) Head Ultrasound Criteria All infants with gestational age <32 weeks (An ultrasound should be done at any gestational age at any time if thought to be clinically indicated) Initial Day 7-10 (In the case of critically ill infants, when results of an earlier ultrasound may effect clinical management, an ultrasound should be performed at the discretion of the clinician) Follow-up (minimum if no abnormalities noted) If no hemorrhage or germinal matrix hemorrhage -If <28 weeks: week 4 and at 40 weeks postmenstrual age (or discharge if <40 weeks) -If 28 0/7-316/7 weeks: week 4 or 40 weeks postmenstrual age (or discharge if <40 weeks) If intraventricular (grade 2+) or intraparenchymal hemorrhage: follow-up at least weekly until stable (more frequently if unstable post-hemorrhagic hydrocephalus and clinically indicated). Daily head circumference measurement should also be performed in the case of ventricular dilatation. Ophthalmologic Examination Criteria All infants with birth weight <1500 gms or gestational age <31 weeks Infants <34 weeks with high illness severity (e.g. those who have had severe respiratory distress syndrome, hypotension requiring pressor support, or surgery in the first several weeks of life). Initial If <27 weeks: week 6 If 27-286/7 weeks: week 5 If 29-306/7 weeks: week 4 Note: -If the infant is transferred to another nursery prior to 4 weeks of age, recommend exam at the receiving hospital -If the infant is discharged home prior to 4 weeks of age, examine prior to discharge Follow-up (based on initial exam findings) Immature retina Zone 1 or Zone 2, or low grade ROP: follow-up every 2 weeks Immature retina Zone 3: follow-up in 3-10 weeks Prethreshold ROP: follow-up at least weekly or more frequently per ophthalmologist recommendation Regressing ROP: follow-up every 1-10 weeks depending on zone Mature retinae: Follow up at 8 months corrected age is recommended as an outpatient Audiology Screening Criteria: All infants to be discharged home from NICU Timing: Examine at 34 weeks gestation or greater Note: This is a general guideline, and it does not represent a professional standard of care governing providers' obligations to patients. Care is revised to meet individual patient needs. 1 Version 11.20.09 Guidelines for Routine Screening, Testing, Treatment and Follow-up Neonatal Intensive Care Unit Beth Israel Deaconess Medical Center Car Seat Testing Criteria All infants to be discharged home from NICU and born at less than 37 weeks or with other conditions that may compromise respiratory status (e.g. airway anomalies and tracheostomy) Timing Examine prior to discharge home Hepatitis B Vaccination For Hepatitis B Negative Mothers (See Hepatitis B Immunoprophylaxis Guidelines from Red Book if maternal status is HB SAgpositive or unknown.) Criteria All infants to be discharged home from NICU Initial If weight >2000 gms and stable: vaccinate at birth or shortly thereafter If weight >2000 and unstable: defer vaccination until their clinical condition has stablized. If weight <2000 gm : vaccinate as early as 30 days or just prior to discharge if baby discharged at < 30 days Follow-up (dose #2) Vaccinate 1 month after initial vaccine dose – may be part of Pediarix: combination vaccine (DPT, Hep B and polio) Synagis RSV Prophylaxis Criteria Synagis RSV prophylaxis should be considered from November through March for infants who meet any of the following criteria: gestational age at birth < 32 0/7 weeks gestational age at birth 32 0/7 to 34 6/7 weeks and either attend childcare or live with siblings under five years of age chronic lung disease hemodynamically significant congenital heart disease congenital abnormalities of the airway or neuromuscular disease (if born before 35 weeks gestation) Occupational Therapy Consultation Criteria All infants meeting one of the following conditions: -Birth at or below 28 weeks gestation -Birth weight < 1000g -Neurological insults including IVH, PVL, seizure d/o -Genetic syndromes which affect quality of movement or state regulation -Symptoms associated with Neonatal Abstinence Syndrome -Orthopedic or musculo-skeletal impairments -Born to parents with physical disabilities -Brachial plexus injury (Erb's or Klumpke’s Palsy) -Critically ill term infants Social Security Criteria All infants meeting one of the following conditions: -Birth weight < 1200 gms -Birth weight 1200-2000 gms and at least 4 weeks small for gestational age (refer to growth curve) -Any infant with serious handicapping conditions Timing Application completed during first week of life Follow-up Parent notifies SSI office of baby’s discharge via form letter. Note: This is a general guideline, and it does not represent a professional standard of care governing providers' obligations to patients. Care is revised to meet individual patient needs. 2 Version 11.20.09 Guidelines for Routine Screening, Testing, Treatment and Follow-up Neonatal Intensive Care Unit Beth Israel Deaconess Medical Center Infant Follow Up Program Criteria All infants meeting one of the following conditions: -Gestational age <28 weeks -Birth weight <1000 gms -Birth weight 1000 – 1499 gms and gestational age <32 weeks with one of the following: Maternal age < 20 IVH (Grades 2-4) PVL Surgical NEC ROP Stage II or greater Psychosocial concerns Timing Referral completed prior to discharge Neonatal Neurology Program Criteria All infants meeting one of the following conditions: -Neurologic disorders (e.g. stroke, intracranial hemorrhage, and neonatal seizures) -Neuromuscular disorders -Birth weight <1500 gms with IVH (Grades 2-4) or PVL (referral to IFUP also) Timing Referral completed prior to discharge Early Intervention Program (EIP) Criteria Infant meeting four or more of the following criteria: -BW < 1200 gms -GA < 32 weeks -NICU admission > 5 days -Apgar < 5 at 5 minutes -IUGR or SGA (refer to growth curves) -Chronic feeding difficulties -Suspected central nervous system abnormality -Abnormal muscle tone -Maternal age <17 or 3 or more births at maternal age < 20 -Maternal education <10 years -Parental chronic illness or disability affecting care giving -Lack of family supports -Inadequate food, shelter, and clothing, including homelessness -Open or confirmed protective service investigation (“51-A”) or file closed by DSS in the last 3 months -Substance abuse in the home -Domestic violence in the home Timing Referral complete prior to discharge Note: This is a general guideline, and it does not represent a professional standard of care governing providers' obligations to patients. Care is revised to meet individual patient needs. 3 Version 11.20.09