NICU Discharge Summary Dictation Procedure
advertisement
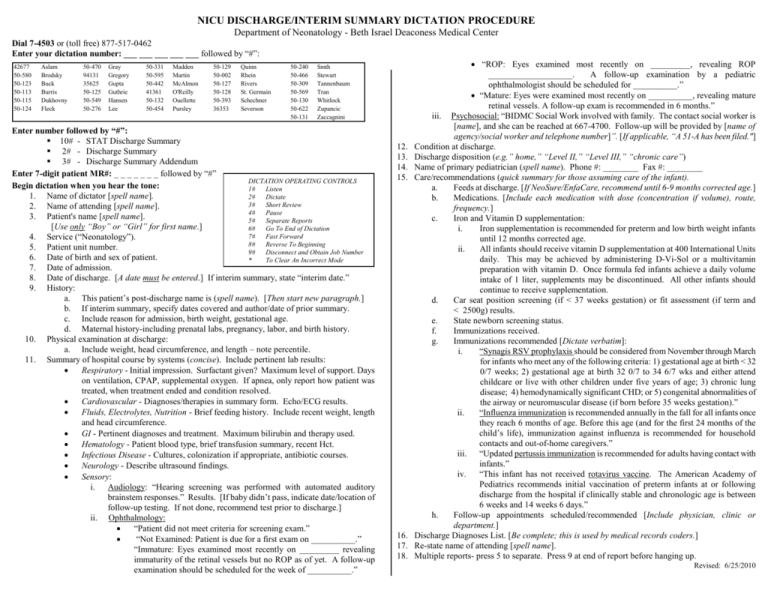
NICU DISCHARGE/INTERIM SUMMARY DICTATION PROCEDURE Department of Neonatology - Beth Israel Deaconess Medical Center Dial 7-4503 or (toll free) 877-517-0462 Enter your dictation number: ___ ___ ___ ___ ___ followed by “#”: 42677 50-580 50-123 50-113 50-115 50-124 Aslam Brodsky Buck Burris Dukhovny Fleck 50-470 94131 35625 50-125 50-549 50-276 Gray Gregory Gupta Guthrie Hansen Lee 50-331 50-595 50-442 41361 50-132 50-454 Madden Martin McAlmon O'Reilly Ouellette Pursley 50-129 50-002 50-127 50-128 50-393 36353 Quinn Rhein Rivers St. Germain Schechner Severson 50-240 50-466 50-309 50-569 50-130 50-622 50-131 Smth Stewart Tannenbaum Tran Whitlock Zupancic Zaccagnini Enter number followed by “#”: 10# - STAT Discharge Summary 2# - Discharge Summary 3# - Discharge Summary Addendum Enter 7-digit patient MR#: _ _ _ _ _ _ _ followed by “#” DICTATION OPERATING CONTROLS Begin dictation when you hear the tone: 1# Listen 1. Name of dictator [spell name]. 2# Dictate 3# Short Review 2. Name of attending [spell name]. 4# Pause 3. Patient's name [spell name]. 5# Separate Reports [Use only “Boy” or “Girl” for first name.] 6# Go To End of Dictation 7# Fast Forward 4. Service (“Neonatology”). 8# Reverse To Beginning 5. Patient unit number. 9# Disconnect and Obtain Job Number 6. Date of birth and sex of patient. * To Clear An Incorrect Mode 7. Date of admission. 8. Date of discharge. [A date must be entered.] If interim summary, state “interim date.” 9. History: a. This patient’s post-discharge name is (spell name). [Then start new paragraph.] b. If interim summary, specify dates covered and author/date of prior summary. c. Include reason for admission, birth weight, gestational age. d. Maternal history-including prenatal labs, pregnancy, labor, and birth history. 10. Physical examination at discharge: a. Include weight, head circumference, and length – note percentile. 11. Summary of hospital course by systems (concise). Include pertinent lab results: Respiratory - Initial impression. Surfactant given? Maximum level of support. Days on ventilation, CPAP, supplemental oxygen. If apnea, only report how patient was treated, when treatment ended and condition resolved. Cardiovascular - Diagnoses/therapies in summary form. Echo/ECG results. Fluids, Electrolytes, Nutrition - Brief feeding history. Include recent weight, length and head circumference. GI - Pertinent diagnoses and treatment. Maximum bilirubin and therapy used. Hematology - Patient blood type, brief transfusion summary, recent Hct. Infectious Disease - Cultures, colonization if appropriate, antibiotic courses. Neurology - Describe ultrasound findings. Sensory: i. Audiology: “Hearing screening was performed with automated auditory brainstem responses.” Results. [If baby didn’t pass, indicate date/location of follow-up testing. If not done, recommend test prior to discharge.] ii. Ophthalmology: “Patient did not meet criteria for screening exam.” “Not Examined: Patient is due for a first exam on __________.” “Immature: Eyes examined most recently on _________ revealing immaturity of the retinal vessels but no ROP as of yet. A follow-up examination should be scheduled for the week of __________.” 12. 13. 14. 15. 16. 17. 18. “ROP: Eyes examined most recently on _________, revealing ROP ___________________. A follow-up examination by a pediatric ophthalmologist should be scheduled for __________.” “Mature: Eyes were examined most recently on __________, revealing mature retinal vessels. A follow-up exam is recommended in 6 months.” iii. Psychosocial: “BIDMC Social Work involved with family. The contact social worker is [name], and she can be reached at 667-4700. Follow-up will be provided by [name of agency/social worker and telephone number]”. [If applicable, “A 51-A has been filed."] Condition at discharge. Discharge disposition (e.g.” home,” “Level II,” “Level III,” “chronic care”) Name of primary pediatrician (spell name). Phone #: ________ Fax #: ________ Care/recommendations (quick summary for those assuming care of the infant). a. Feeds at discharge. [If NeoSure/EnfaCare, recommend until 6-9 months corrected age.] b. Medications. [Include each medication with dose (concentration if volume), route, frequency.] c. Iron and Vitamin D supplementation: i. Iron supplementation is recommended for preterm and low birth weight infants until 12 months corrected age. ii. All infants should receive vitamin D supplementation at 400 International Units daily. This may be achieved by administering D-Vi-Sol or a multivitamin preparation with vitamin D. Once formula fed infants achieve a daily volume intake of 1 liter, supplements may be discontinued. All other infants should continue to receive supplementation. d. Car seat position screening (if < 37 weeks gestation) or fit assessment (if term and < 2500g) results. e. State newborn screening status. f. Immunizations received. g. Immunizations recommended [Dictate verbatim]: i. “Synagis RSV prophylaxis should be considered from November through March for infants who meet any of the following criteria: 1) gestational age at birth < 32 0/7 weeks; 2) gestational age at birth 32 0/7 to 34 6/7 wks and either attend childcare or live with other children under five years of age; 3) chronic lung disease; 4) hemodynamically significant CHD; or 5) congenital abnormalities of the airway or neuromuscular disease (if born before 35 weeks gestation).” ii. “Influenza immunization is recommended annually in the fall for all infants once they reach 6 months of age. Before this age (and for the first 24 months of the child’s life), immunization against influenza is recommended for household contacts and out-of-home caregivers.” iii. “Updated pertussis immunization is recommended for adults having contact with infants.” iv. “This infant has not received rotavirus vaccine. The American Academy of Pediatrics recommends initial vaccination of preterm infants at or following discharge from the hospital if clinically stable and chronologic age is between 6 weeks and 14 weeks 6 days.” h. Follow-up appointments scheduled/recommended [Include physician, clinic or department.] Discharge Diagnoses List. [Be complete; this is used by medical records coders.] Re-state name of attending [spell name]. Multiple reports- press 5 to separate. Press 9 at end of report before hanging up. Revised: 6/25/2010







