surgical-site-infection-prevention
advertisement
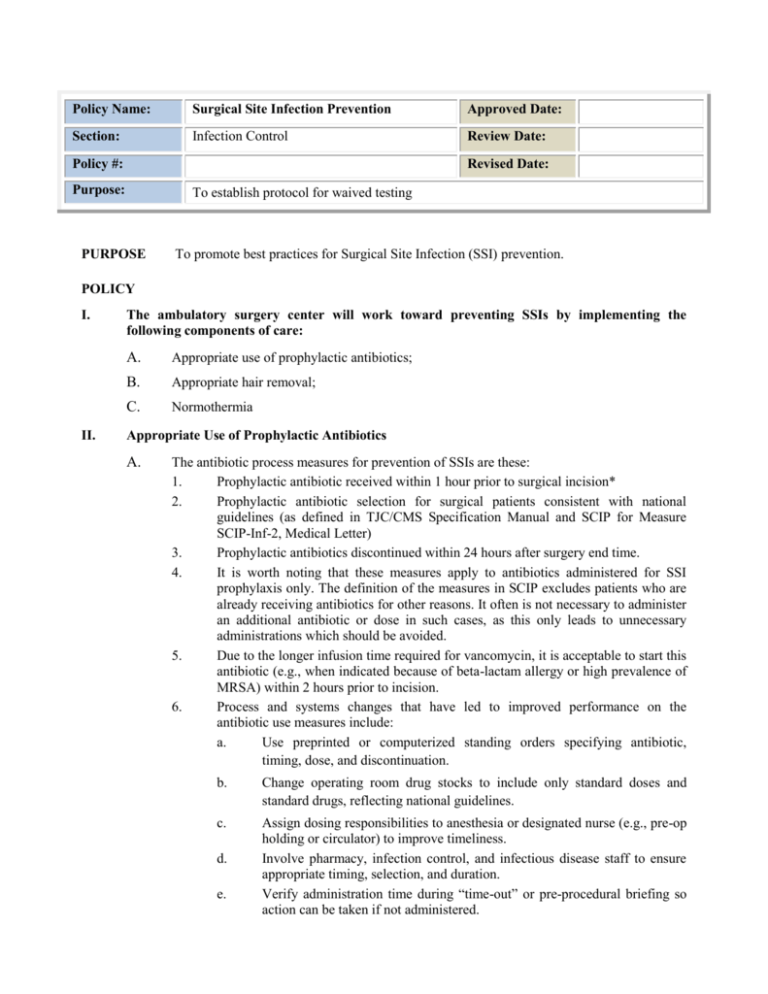
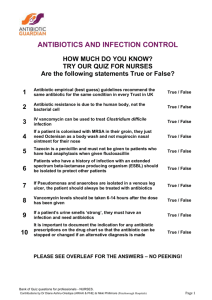
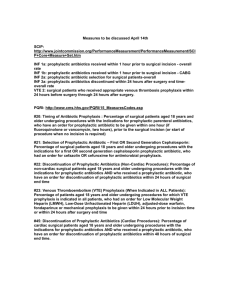
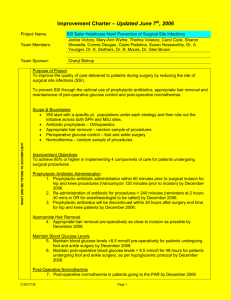
Policy Name: Surgical Site Infection Prevention Approved Date: Section: Infection Control Review Date: Policy #: Revised Date: Purpose: To establish protocol for waived testing PURPOSE To promote best practices for Surgical Site Infection (SSI) prevention. POLICY I. II. The ambulatory surgery center will work toward preventing SSIs by implementing the following components of care: A. Appropriate use of prophylactic antibiotics; B. Appropriate hair removal; C. Normothermia Appropriate Use of Prophylactic Antibiotics A. The antibiotic process measures for prevention of SSIs are these: 1. Prophylactic antibiotic received within 1 hour prior to surgical incision* 2. Prophylactic antibiotic selection for surgical patients consistent with national guidelines (as defined in TJC/CMS Specification Manual and SCIP for Measure SCIP-Inf-2, Medical Letter) 3. Prophylactic antibiotics discontinued within 24 hours after surgery end time. 4. It is worth noting that these measures apply to antibiotics administered for SSI prophylaxis only. The definition of the measures in SCIP excludes patients who are already receiving antibiotics for other reasons. It often is not necessary to administer an additional antibiotic or dose in such cases, as this only leads to unnecessary administrations which should be avoided. 5. Due to the longer infusion time required for vancomycin, it is acceptable to start this antibiotic (e.g., when indicated because of beta-lactam allergy or high prevalence of MRSA) within 2 hours prior to incision. 6. Process and systems changes that have led to improved performance on the antibiotic use measures include: a. Use preprinted or computerized standing orders specifying antibiotic, timing, dose, and discontinuation. b. Change operating room drug stocks to include only standard doses and standard drugs, reflecting national guidelines. c. Assign dosing responsibilities to anesthesia or designated nurse (e.g., pre-op holding or circulator) to improve timeliness. Involve pharmacy, infection control, and infectious disease staff to ensure appropriate timing, selection, and duration. Verify administration time during “time-out” or pre-procedural briefing so action can be taken if not administered. d. e. III. Appropriate Hair Removal A. The use of razors prior to surgery increases the incidence of wound infection when compared to clipping, depilatory use, or no hair removal at all. When hair must be removed to safely perform the procedure, it should never occur with a razor. The use of clippers has been found to be the best method in many facilities, as depilatory creams can cause skin reactions. 1. 2. 3. 4. 5. IV. Ensure adequate supply of clippers and train staff in proper use. Use reminders (signs, posters). Educate patients not to self-shave preoperatively. Remove all razors from the center. Work with the purchasing department so that razors are no longer purchased. Normothermia A. Maintaining the patient's internal temperature has been found to help reduce the risk of postoperative infection. B. Use a warming device. References: 5 Million Lives Campaign. Getting Started Kit: Prevent Surgical Site Infections How-to Guide. Cambridge, MA: Institute for Healthcare Improvement; 2008. http://www.ihi.org/IHI/Topics/PatientSafety/SurgicalSiteInfections/ Yokoe DS, Mermel LA, Classen, D, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008; 29:S12-S21. http://www.shea-online.org/about/compendium.cfm