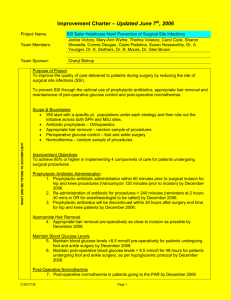
Slide - community360.net

Surgical Site Infection Prevention
The Cardiac Surgery Translational Study (“CSTS”)
The Quality And Safety Research Group
Elizabeth Martinez, MD, MHS emartinez10@partners.org
March 18, 2011 Immersion Calls
Immersion call Schedule
Title
Program Overview
Science Of Safety
Comprehensive Unit-Based Safety
Program CUSP
Central Line Blood Stream Infection
Elimination
Surgical Site Infection Elimination
Ventilator-Associated Pneumonia
Reduction
Hand-Offs: Transitions in Care
Data we Can Count on
Team Building
Physician Engagement
Date /Time
13:00 EST
Feb 18, 2011
Presented by
Peter Pronovost MD PhD
February 25, 2011 Jill Marsteller, PhD, MPP
March 4, 2011 Christine Goeschel MPA MPS ScD RN
March 11, 2011 David Thompson DNSC, MS
March 18, 2011 Elizabeth Martinez, MD, MHS
March 25, 2011 Sean Berenholtz, MD
April 1, 2011
April 8, 2011
April 15, 2011
April 22, 2011
Ayse Gurses, PhD
Lisa Lubomski, PhD.
Jill Marsteller, PhD, MPP
Peter Pronovost, MD, PhD
Slide 2
CSTS Timeline
• Planned Roll-out
– CLABSI Prevention interventions and monthly data collection: June, 2011
– SSI Prevention interventions and monthly data collection: Approximately September 2011
– VAP Prevention and monthly data collection:
After December 2011
Slide 3
Learning Objectives
• To understand the model for translating evidence into practice
• To explore how to implement evidence-based behaviors to prevent SSI
• To understand strategies to engage, educate, execute and evaluate
Slide 4
Proportion of Adverse Events
Most Frequent Categories
Non-surgical
Surgical
Brennan. N Engl J Med. 1991;324:370-376
Slide 5
Introduction
• Over 300,000 CABG annually
• SSI rates 3.51% (10,500 annually)
– 25% mediastinitis
– 33% saphenous vein site
– 6.8% multiple sites
• Increased mortality:17.3% v. 3.0% (p<0.0001)
• Increased LOS: 47% v 5.9% with LOS>14days (p<0.0001)
• Increased cost: $20,000 to $60,000
Fowler et al..
Circ , 2005:112(S), 358.
Slide 6
Background: An Example of
Surveillance Methodology
National Healthcare Safety Network (NHSN)
• Formerly NNIS
• National Healthcare Safety Network surveillance
• CDC program that reports aggregated surveillance data from ~thousands of US hospitals
• hospitals/mandated for certain infections in order to receive full Medicare payment
• Standard case-finding (by ICD-9 code), definitions for infection, and risk-stratification methodology
• Pooled mean and standard deviation reported for surgical procedures
• SSIs can develop up to 1-year postop
• ‘hardware’ = sternal wires
Slide 7
CABG SSI Risk Model*
Preop
• Age
• Obesity
• Diabetes
• Cardiogenic shock
• Hemodialysis
• Immunosuppression
Intraop
• Perfusion time
• Placement of IABP
• ≥ 3 anastomoses
*Did not include known best practices (e.g. SCIP)
Fowler et al..
Circ , 2005:112(S), 358.
Traditional SSI Risk Factors
Intrinsic-Patient Related
• Age
• Nutritional status
• Diabetes
• Smoking
• Obesity
• Remote infections
• Endogenous mucosal microorganisms
• Altered immune system
• Preoperative stay-severity of illness
• Wound class
Slide 9
Translating Evidence into Practice
Pronovost, Berenholtz, Needham. BMJ 2008
Slide 10
Evidence Based Practices that Reduce risk of SSIs*
• Appropriate prophylactic antibiotics
– Selection
– Timing (and redosing)
– Discontinuation
• Appropriate hair removal as close to time of surgery as possible:
– Don’t remove hair unless necessary; If you remove hair -
Don’t shave. Can use clipper/depilatory (AVOID razors)
• Normothermia in non CPB cases
• Appropriate glycemic control
*************************************************************
• Chlorhexidine surgical skin prep (used appropriately)
Slide 11
*SCIP measures
Your Hospitals’ Performance*
95
94
93
92
91
100
99
98
97
96
90
Antibiotic stopped at right time Proper hair removal
*summarized (estimate) data for all surgical procedures from all participating Institutions as of 3/31/2011 www.hospitalcompare.hhs.gov;
Accessed 3/5/2011
Slide 12
Ensure Patients Reliably
Receive Evidence
Engage
Educate
Execute
Evaluate
Senior leaders
Team leaders
Staff
How does this make the world a better place?
What do we need to do?
What keeps me from doing it?
How can we do it with my resources and culture?
How do we know we improved safety?
Slide 13
TRiP: Model to Improve
• Pick an important clinical area
• Identify what should we do
– principles of evidence-based medicine
• Measure if you are doing it
• Ensure patients get what they should
– Education
– Create redundancy
– Reduce complexity/standardize
• Evaluate whether outcomes are improved
Slide 14
Systems Approach
• Every system is perfectly designed to get the results that it gets.
- Bataldan
• If you want to change performance you need to change the system.
Slide 15
Science of Safety
• Accept that we will make mistakes
• Focus on systems, including interpersonal communication, rather than people
• Largest barrier is lack of awareness evidence exists
• Standardize to reduce complexity
• Create independent checks
Slide 16
Eliminating SSI
• Apply best practices
– If hair is removed, use clippers or depilatory
– Appropriate antibiotics
• Choice
• Timing
• Discontinuation
– Perioperative normothermia
– Glycemic control
• Decrease complexity
• Create redundancy
Slide 17
Tips for Success
• Engage
– Make the problem real
– Publicly commit that harm is untenable
• Educate
• Execute
– Culture, complexity and redundancy
– Regular team meetings
• Evaluate
– Measurement and feedback
– Recognition and visibility
– Celebrate your successes
Slide 18
Engage
• Make the problem real
– Share local infection rates
– Share local compliance with process measures
– Share a story of a patient with SSI
• Have the patient share their story
• Publicly commit that harm is untenable
– Institutional commitment
– Champions within the OR and the ICU and floor teams
– Partnership with Infection Preventionist
Slide 19
Educate
– Develop an educational plan to reach ALL members of the caregiver team
– Educate on the evidence based practices AND the data collection plan and other steps of the process.
– Use posters to educate the teams about the evidence-based process measures
Slide 20
Avoid Razors
Avoid Hypothermia
Give Correct Antibiotics
Give Antibiotics at the Right Time
* Within 60 minutes prior to incision
Redose Antibiotics Appropriately
Antibiotics at 24 Hours
Perioperative SSI Process Measures
Quality Indicator Numerator Denominator
Appropriate antibiotic choice
Appropriate timing of prophylactic antibiotics
Appropriate discontinuation of antibiotics
Appropriate hair removal
Perioperative normothermia
Number of patients who received the appropriate prophylactic antibiotic
Number of patients who received the prophylactic antibiotic within
60 minutes prior to incision
Number of patients who received prophylactic antibiotics and had them discontinued in 24 hours
Number of patients who did not have hair removed or who had hair removed with clippers
Number of patients with postoperative temperature ≥36.0
o C
All patients for whom prophylactic antibiotics are indicated
All patients for whom prophylactic antibiotics are indicated
All patients who received prophylactic antibiotics
All surgical patients
Patients undergoing surgery without CPB/planned hypothermia
Perioperative glycemic control Number of cardiac surgery patients with glucose control at 6AM pod 1 and 2
Patients undergoing cardiac surgery
Slide 22
Execute
• Culture
– Develop a culture of intolerance for infection
• Standardize/Reduce complexity of the process
– Checklists -Confirm abx administration during briefing
– Utilize glycemic control protocol
– Local antibiotic guidelines posted in Ors
– Standardize surgical skin prep
• Redundancy
– Add best practices to briefing/debriefing checklist
– Post reminders in the OR (White board)
– Antibiotic timer program for redosing
• Regular team meetings
– Develop a project plan
– Identify barriers
Slide 23
Evaluate
• Track compliance with SCIP measures
– Performance measures already being tracked by hospitals as part of SCIP participation*
– Post performance on monthly basis
• Post in the OR, ICU and floor
• Investigate non-compliant cases on a monthly basis
– Use Learning from Defect (LFD) tool
• Post SSI rates on a monthly/quarterly basis
– Investigate each SSI with the CUSP team to identify areas for improvement using the LFD tool
• Audit performance with skin prep methodology (at a minimum) and goal is conversion to chlorhexidine
*based on data availability on
Hospital compare
Slide 24
Share Results
Slide 25
Acknowledgements
Deborah Hobson, BSN
Pamela Lipsett, MD
Sara Cosgrove, MD
Lisa Maragakis, MD
Trish Perl, MS
Matthew Huddle, BS
Nicole Errett, BS
Justin Henneman, BS
The Johns Hopkins SSI Prevention Collaborative teams
Slide 26
QUESTIONS?
Thank You!
Elizabeth Martinez, MD, MHS
Massachusetts General Hospital, Harvard University emartinez10@partners.org