K B Roberts, MD-1
advertisement

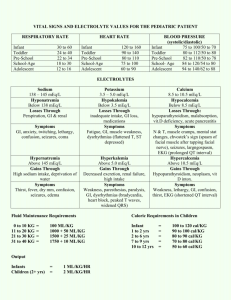
FLUID & ELECTROLYTES: PARENTERAL FLUID THERAPY Can be complex, confusing, even intimidating—but can be mastered if the problem is dissected A. There are 3 components of fluid management 1. Maintenance: what we all lose normally and continuously through skin, lungs, stool, and urine 2. Deficit: the loss incurred prior to the institution of therapy (e.g., from diarrhea for the past 2 days) 3. Ongoing Losses: loss incurred after the institution of therapy (e.g., continued watery stools, N-G drainage) B. For each component, 1. First decide AMOUNT of fluid (water) 2. Then COMPOSITION (electrolytes) 1 MAINTENANCE A. The Basics What maintenance is: Providing fluid used up during basal metabolism What maintenance is not: Replacement of a deficit or on-going losses (maintenance does NOT rehydrate a child). So “2-times maintenance” is not a valid replacement strategy Fundamental question: Why do we need fluid to maintain homeostasis? To replace the water used to eliminate the 2 by-products of metabolism: “heat” and “waste.” (Explains why fluid needs are based on metabolic rate, rather than directly on weight.) 1. “Heat” (accounts for roughly half (50%) of maintenance fluids) a. Lose heat by evaporation from skin (different from active sweating, which implies an increased heat burden to be dissipated). These are “insensible losses” in that you do not feel the loss of fluid as you are losing it. b. Insensible losses also include water lost in GI secretions and water the nose puts into inspired air to humidify air (later exhaled as water vapor) 2. “Waste” solute (roughly half (50%) of maintenance fluids) a. Water soluble compounds (eg, nitrogenous waste urea ) excreted in urine b. “Sensible” not only because you feel & see the loss but also because the kidney can dilute or concentrate the amount of water the solute is diluted in B. AMOUNT of Maintenance 1. Since metabolic rate is not related linearly to weight, need a “system:” 2. Three "systems" used: a. Surface area b. Basal calorie: the driest; requires table c. **Holliday-Segar formula (most commonly used one now) AKA 4:2:1 rule. 1) Note the difference in caloric needs between basal metabolic rate (the amount you use at bedrest) versus the caloric need with normal activity. An average of these is used for hospitalized children, but it will overestimate the caloric needs of kids who have markedly reduced activity Table 1: COMPUTED need for “average hospitalized patient” 140 Estimated total expenditure with normal activity Calories/day (ml/hr) 120 100 Weight 90 0-10 kg 11-20 kg 80 70 80 60 60 40 Basal metabolic rate 40 >20 kg 20 0 0 10 20 30 40 Weight in kilograms 2 50 60 Calories (= ml) per hour 4 per kg 2 per each kg between 10 and 20 + 40 for the 1st 10 kg 1 per each kg >20 + 60 for the 1st 20 kg Calories (= ml) per day 100 per kg 50 per each kg between 10 and 20 + 1000 for the 1st 10 kg 20 per each kg above 20 + 1500 for the 1st 20 kg Table. Calories expended per day (or per hour) by weight MAINTENANCE 3. So, 1000 calories metabolized requires 1000 ml of fluid: Table 2: Sources of Water Loss Source of Water Loss Usual Losses (ml/1000 kcal metabolized) Lung 150 Skin 300 Stool 50 Urine 500 Total 1000 Notes a. Lungs: patients receiving humidified O2 or air may not need this b. Skin: does not include active sweating c. Urine: presumes basal (non-catabolic) conditions and urine that is isotonic (neither concentrated nor dilute) = 300 mOsm/L (specific gravity of 1.010) d. Notice that urine and insensible losses each constitute approximately half of maintenance fluid needs. This useful guide has clinical implications: 1) An anuric patient should only receive insensible losses 2) A patient whose urine output is questionable can receive insensible losses plus volume equal to urine output (treat urine output as “ongoing loss”) 4. Remember, maintenance is different than rehydration: Placing a dehydrated child on “1 ½ time maintenance” generally means “lack of calculation.” C. COMPOSITION of Maintenance 1. Virtually all electrolyte loss is urinary. So, for every 1000 calories metabolized, 1000 mL of water, ~30 mEq of Na and ~20 mEq of K + are needed. (see the chart below). a. What, then, should the composition of maintenance fluid be (for all ages & weights)? b. Answer: D5 ¼ NS with 20 mEq/L KCl. Let’s dissect that: 1. Normal Saline (NS) consists of 154 mEq of Na for every 1000 mL (See table on p4) 2. Note that 32 mEq/L is about ¼ of 154 mEq/L 3. Since there is no K+ in NS, you need to specifically add it. 4. D5 ¼ NS applies to all ages & weights because the ratio of 32 mEq Na per 1000 mL of water is constant. Once you have figured out how much water is needed for maintenance, the amount of Na is straightforward. Table 3: Sources of Water & Electrolyte Loss Source of Loss Water (ml/L) Sodium (mEq/L) Potassium (mEq/L) Lungs Skin Stool Urine 150 300 50 500 0 1 1 30 0 2 2 20 Total 1000 32 24 c. When does D5 ¼ NS with 20 mEq/L KCl not apply? 1. An anuric patient needs no sodium or potassium for maintenance 2. When urine output is compromised by renal disease, the ratio of Na:water will change 3. When urine output is compromised by ADH secretion (inappropriate), the ratio of Na:water will also change 3 MAINTENANCE D. Summary of Maintenance 1. Determine AMOUNT (ml) a. Estimate caloric expenditure using the 4:2:1 rule b. convert kcal = ml, unless vital organs are compromised 2. Determine COMPOSITION (electrolytes) a. D5 ¼ NS with 20 mEq/L KCl, unless kidneys are compromised 4. Determine RATE: a. In the hospital, fluid and electrolytes generally are given evenly over 24 hours b. This is a convention for our convenience. Not necessary to do it this way, particularly when maintenance is being provided orally. In the real world, we get our maintenance fluids unevenly (e.g., how many times did you get up last night to drink water?) c. Again, note that speaking of "twice maintenance" is commonly talked about on the inpatient wards but does not have any physiologic basis unless your metabolic needs suddenly doubled. Table 4: Composition of Frequently Used IV Fluids Liquid Carbohydrates (g/100 mL) Na (mEq/L) K+ (mEq/L) Cl (mEq/L) NS (0.9 % NaCl) 154 154 ½ NS (0.45% NaCl) 77 77 ¼ NS (0.225% NaCl) 38 38 38 38 D5 ¼ NS (0.22% NaCl) 5 Lactated Ringer’s (LR) D5W 3% NS 5 HCO3 (mEq/L) 130 4 109 28 0 0 0 0 513 513 DEFICIT A. AMOUNT "% dehydration" refers to % of body weight lost. You can assume any acute weight loss is fluid, since weight loss >1% of body weight per day virtually has to be fluid. There are two methods of estimating % body weight loss 1. Weight change (e.g., today’s weight in the ED – weight in the office 3 days ago) 2. Clinical estimate a. Based on thirst, decreased urination (with increased spec gravity), moistness of mouth, skin turgor, fontanelle, pulse rate, blood pressure, perfusion b. Note difference between infant and adolescent (adult) 4 DEFICIT Table 6: Estimating the % of dehydration Clinical Data Dry mucous membranes, Oliguria Hemodynamic Severity of Infant Adolescent Changes Est. fluid loss Est. fluid loss Dehydration Normal Marked oliguria, Tachycardia Poor skin turgor, Sunken fontanel, Tachycardia Hypotension, Poor perfusion Hypotension, Poor perfusion Problems in Assessment Mild 5% (50 ml/kg) 3% (30 ml/kg) Oral mucosa may be dry in chronic mouth breathers Frequency and amount of urination may be difficult to assess during diarrhea, esp. in infant girls Moderate 10% (100 ml/kg) 6% (60 ml/kg) Oliguria: See above Turgor affected by serum [Na+]** Heart rate affected by fever, [Na+]**, underlying disease Severe 15% (150 ml/kg) 9% (90 ml/kg) Both may be affected by [Na+]**, underlying disease **[Na+] >150mEq/L gives falsely low estimate of severity; [Na+] <130mEq/L exaggerates clinical estimate of severity B. COMPOSITION Depends on 3 things: a. Time period of loss b. Type of fluid lost (e.g., diarrhea, vomiting) c. Current electrolytes 1. Time period of loss a. "Hyperacute" loss over hours: most of the loss is from the extra-cellular fluid (ECF). Therefore, the child needs a fluid similar to ECF, such as Ringers lactate (LR) or normal saline (NS) b. "Acute" loss over few days: time for equilibration between ECF and ICF means less sodium lost, more potassium. This is what you will deal with most of the time. c. "Chronic" loss over weeks: time to equilibrate further, so the composition of what is lost will look more like the ICF (i.e., even less sodium lost and more total body potassium depletion) 2. Type of fluid lost a. Most sources of fluid loss (diarrhea, vomiting, DKA) approximate the amount of sodium in ½ NS (see table below) (80 mEq is about ½ of the 154 mEq in NS) Table 7: Electrolyte Loss for Various Sources of Dehydration Cause of Deficit 5 + + "Usual" Deficit of [Na ] "Usual" Deficit of [K ] Diarrhea Isotonic dehydration Hypotonic dehydration Hypertonic dehydration 80 mEq/L 100 mEq/L 20 mEq/L 80 mEq/L 80 mEq/L 10 mEq/L Pyloric stenosis 80 mEq/L 100 mEq/L DEFICIT 3. Current electrolytes will modify your fluid regimen a. Sodium is key 1) 135 - 150 = isotonic 2) >150 = hypertonic 3) <135 = hypotonic b. Isotonic: no modifications c. Hypertonic dehydration 1) Amount of deficit is usually underestimated by physical examination since intravascular volume and circulation are bolstered (at the expense of intracellular water) 2) Skin is often described as "doughy" 3) Decreasing sodium too quickly can cause serious problems – the preferred method is to add replace the deficit and 2 days of maintenance over 48 hours. 4) Do not confuse salt poisoning with hypernatremic dehydration. d. Hypotonic dehydration 1) Amount of deficit may be overestimated by physical examination 2) Increasing sodium too quickly can cause serious problems – If forced to act (eg, because of seizures), calculate Na to raise serum [Na+] to ~125 (out of seizure range) and give rapidly as 3% solution followed by severe water restriction. a) Amount of 3% NaCl (in ml) to give if patient is hyponatremic and seizing: = (125 mEq/L – actual serum Na) x (wt in Kg) x 0.6 L/kg 3) NOTE: Hyponatremia more often represents excess of water than insufficiency of sodium! e. Anions 1) When considering replacement fluids, consider what anion was likely lost. On the ward, K+ is often provided as KCl by default – but this does not always make sense i. Diarrhea: the child loses bicarb. Therefore, replace the K+ as KAcetate. ii. DKA: the child may be hypophosphatemic. Therefore, replace the K+ as Kphos iii. Profuse vomiting (eg, pyloric stenosis): the child loses chloride. Therefore, replace the K+ as KCl. 2) “Normal saline” contains the same amount of Cl as Na which is not physiologic. Ringer’s lactate contains 130 mEq/L Na & 100 mEq/L Cl (see table 4) C. RATE 1. Hippocrates: "Those bodies which have been slowly emaciated should be slowly recruited; and those which have been quickly emaciated should be quickly recruited." 2. I can't do better than that! 6 DEFICIT D. Summary/Example of Deficit Joey, a 15 kg child comes in with vomiting & diarrhea for 3 days. He has dry mucous membranes, tachycardia, decreased wet diapers, and poor skin turgor. His capillary refill and blood pressure are normal 1. The first step is to support circulation give Ringers lactate or normal saline at 20 ml/Kg = 300 mL a. 20 ml/Kg is chosen because it is frequently enough to support circulation but generally not so much as to produce congestive failure b. If the first 20 ml/Kg isn't enough, give more until HR, perfusion return to normal: the goal is stable circulation. c. Sad that we mix units: We speak of dehydration in % but rehydration in ml/Kg; note that 20 ml/Kg = 2%. Helps in guessing what changes to expect: If a child is “15% dehydrated,” will the child be “fluid resuscitated” with a single bolus of 20 ml/Kg? (Hint: 15% - 2% = 13%) 2. Determine AMOUNT (ml) a. Two options for estimating the amount of deficit include weight change or clinical signs. Joey’s clinical signs point to 10% dehydration 10% of 15 kg = 1.5 liter. If you already gave him a 300 mL (20/kg) bolus, there are 1200 mL remaining to give. 3. Determine COMPOSITION (electrolytes) a. Amount of Na deficit depends on the mechanism of loss (see table 7). Joey has diarrhea, so he is likely losing 80 mEq of Na per liter of fluid. Normal Saline is 154 mEq per liter and 80 is about ½ that. Therefore the fluid of choice is D5 ½ NS. 4. Put it together and write your fluid orders: a. 300 mL LR bolus b. D5 ½ NS + 20 mEq/L Kacetate @ 150/hr x 8 hours (the remaining 1200 mL 8 hours) c. D5 ¼ NS + 20 mEq/L Kacetate @ 78/hr x 16 hours (It is not enough to replace deficit; Joey still needs his daily maintenance fluid of 1250 mL [100/kg for the first 10 kg = 1000 mL + 50/kg for the last 5 kg = 250 mL]. Since we used up 8 hours to replace Joey’s deficit, we can give 24 hrs worth of maintenance over the remaining 16 hours 1250 ml 16 hours = 78 ml/hr) 5. HINTS a. In "usual" situation, my bias is to rehydrate promptly, since the child will feel better when rehydrated and be less nauseous with ketones washed out, increasing the likelihood of oral intake being successful b. If you estimate the child’s dehydration to be ~10% and give 20 ml/Kg (2%) as bolus, then remainder of deficit is 8%. You can give this over 8 hours @ 10 ml/Kg/hr (1% per hour), math you can do in your head! Then give the entire day’s maintenance over the subsequent 15 or 16 hours (instead of 24) and you will have calculated and delivered appropriate rehydration without the need of complex calculations! (See example later in handout.) 7 ONGOING LOSSES A. Basic concept of ongoing losses 1. All of the above calculations are approximate; guidelines which in no way can replace careful monitoring of the patient therefore you MUST reassess your patient. 2. Note, however, that no single, simple sign or test infallibly reflects fluid and electrolyte balance 3. The following measures are listed in rough order of practical value, considering degree of ease, availability, invasiveness, time to perform, and cost Table 8: SIGNS AND TESTS TO MONITOR STATE OF HYDRATION Sign or Test 1. Physical signs of dehydration (PE) 2. Body weight 3. Urine volume 4. Urine specific gravity 5. I & O, with direct measure of all losses 6. Urea nitrogen (BUN) 7. Hematocrit 8. Concurrent serum & urine osmolalities 9. Serum electrolyte concentrations Problem May be deceiving if [Na+] abnormal, may be influenced by fever (esp pulse) Can be fooled by "third spacing" Output also low in SIADH, renal failure Concentrating ability of infant kidney limited; SG also high in SIADH, renal failure; SG low in pyelonephritis, ATN Must estimate maintenance; cannot measure "third space" loss GFR severely reduced before BUN rises; elevated by blood in GI tract; infant normally lower than adult; may mean renal disease Useful serially but not as single value and not if patient is actively bleeding Good for detecting SIADH problem By themselves, say little about state of hydration 4. Frequency of monitoring must be individualized, depending on the present severity of the disorder and the potential rate of change. Once daily is rarely sufficient. Thoughtful reassessment and attention to detail are key. B. AMOUNT (fluid) 1. Measure what you can (e.g., stool output in diapers) 2. Estimate what you must (e.g., amount of emesis) 3. In some situations, may also want to consider "ongoing gains:" e.g., fluids used to deliver medications 8 ONGOING LOSSES C. COMPOSITION (electrolyte) 1. Estimate from table: Table 9: Electrolyte Loss in Ongoing Losses Fluid Sodium (mEq/L) Gastric Bile Ileostomy Diarrheal Sweat: Normal Sweat: Cystic fibrosis Burns 20-80 120-140 45-135 10-90 10-30 50-130 140 Potassium (mEq/L) 5-20 5-15 3-15 10-80 3-10 5-25 5 Chloride (mEq/L) 100-150 80-120 20-115 10-110 10-35 50-110 110 2. Measure (lab) if profuse or prolonged 3. Also consider "ongoing gains" in situations such as heart-, brain-, or kidneycompromised patients who require salt restriction and whose IV meds require NaCl as diluent D. RATE 1. If a child has significant ongoing losses (profuse diarrhea) or does not seem to be getting better despite seemingly adequate fluid therapy, you can replace ongoing losses mL for mL. Example: 8 hours after admission, a 2 year old with rotavirus gastroenteritis has 400 mL of measured stool losses and no unmeasured emesis. Your order could state: Replace stool output mL for mL with ½ NS + 20 mEq/L Kacetate every 4 h. 2. For convenience, I prefer to administer replacement "piggy-back," separate from maintenance, since it simplifies calculations: keep separate bag of appropriate composition hung with orders to infuse volume equal to the loss at specified interval. PUTTING IT TOGETHER: AN EXAMPLE An infant who now weighs 10 kg has had diarrhea for 3 days. Clinical findings support the estimate of 10% fluid deficit: dry mucous membranes, poor skin turgor, markedly decreased urine output, and tachycardia; BP is normal and adequate peripheral perfusion is shown by compression-release of the nail beds. Serum [Na] is 136 mEq/L, [K] 4 mEq/L, [Cl] 104 mEq/L, [HCO3] 18 mEq/L. A. Let’s do AMOUNT first (then Composition) 1. Deficit: 10% of 10 kg = 1000 mL 2. Maintenance: Since infant’s weight is 0-10 Kg, use 100 kcal/Kg/day x 10Kg = 1000kcal/day = 1000ml/day 3. Ongoing losses: Amount to be determined as course progresses (weigh diapers) o Resuscitative portion of deficit: 20 ml/Kg x 10 Kg = 200 ml as bolus (usually given over about 30-60 minutes) o Remainder of deficit: 800 ml (1000 deficit – 200 bolus) given over 8 hrs = 100 mL/hr o Maintenance: “Behind” on replacing maintenance, so need to give first day supply (24 hours worth) = 1000ml in 15-16 hours = 60 mL/hr. o Ongoing losses: Will add as needed 9 PUTTING IT TOGETHER: AN EXAMPLE B. Now, address COMPOSITION: (We’ll do the detailed calculations as a demonstration) 1. Deficit: (from Table 7): 80 mEq Na x 1 liter = 80 mEq Na 2. Maintenance: 30 mEq Na x 1 liter = 30 mEq Na 3. Ongoing losses: Based on reassessment o Resuscitative portion of deficit: you gave 200 mL (0.2 L) of Ringer's lactate (130 mEq/L Na, 4 mEq/L K) 0.2 L x 130 mEq = 26 mEq Na o Remainder of deficit: (Na): 80 mEq (deficit) - 26 mEq (given in Ringer's) = 54 mEq. o 54 mEq in 800 ml (remainder of deficit fluid) = 68 mEq/L. The closest standard fluid is D5 ½ NS (77 mEq/L) o Acceptable shortcut: Once having made these calculations for different children, it becomes clear that D5 ½ NS is the deficit-replacement fluid for isotonic dehydration. o Maintenance: D5 ¼ NS (38 mEq/L) + 20 mEq/L KAcetate C. Summary 1. Ringer's lactate 200 ml x 30 minutes 2. D5 ½ NS + 20 mEq/L KAcetate @ 100 ml/hr x 8 hours 3. D5 ¼ NS + 20 mEq/L KAcetate @ 60 ml/hr x 16 hours 4. D5 ¼ NS + 20 mEq/L KAcetate @ 40 ml/hr thereafter until the child is drinking again D. Notes 1. You can use the observed weight and apply the estimated % deficit without having to calculate the “pre-dehydration” weight. For example, this 10 Kg child, if “10% dehydrated,” must have originally weighed 11.1 Kg. The difference in amount isn’t worth the added step in calculation. 2. Only sodium needs are calculated in this example: the amount and rate of potassium administered is governed by safety, and full replacement is not achieved acutely. Once urine output is assured and it is thus considered safe to administer potassium, 20 to 40 mEq/L is added to the replacement solutions. 3. Sequential replacement of deficit and maintenance fluids is demonstrated in the example; the method is convenient, illustrates the approach in the outline, and results in an appealing stepwise, progressive decrease in the amount of fluid and concentration of sodium from resuscitation to maintenance. 10 PUTTING IT TOGETHER: AN EXAMPLE a. Recall that for children who are “10% dehydrated,” giving a bolus of 20 ml/Kg (2% of body weight) leaves 8% that needs to be replaced: You should not go directly to maintenance rate or a maintenance solution. If you provide the 8% replacement over 8 hours, you are giving 1% of body weight per hour (10ml/kg/hr). Look how simple the math becomes! b. Many clinicians prefer to combine deficit and maintenance replacement and/or to proceed more slowly; that method also works and is preferred in hypernatremic dehydration. c. Many residents learn (and teach) that you should give half the deficit in the first 8 hours and the other half in the next 16 hours along with maintenance fluid. This is much more work (in terms of calculations) than necessary. For example, had you done that for the example, you would have divided the 800 ml deficit (after the resuscitation phase) into halves and planned to give 400 ml in the first 8 hours and the other 400 ml in the next eight hours. You then would have had to figure out 8 hours of maintenance to give along with the first half of the deficit and 16 hours of maintenance to give with the second half. Once you did all of that you would have come out with 400+320=720 ml for the first 8 hours and 400+640=1040 for the next 16 hours. Compare that to just replacing the deficit in 8 hours (800 ml) and finishing the day’s maintenance in 16 hours (1000 ml): Deficit + Maintenance Method: “Easy” Sequential Method: 11 1st 8 hours 720 ml 800 ml next 16 hours 1040 ml 1000 ml ANSWERS TO THE PROBLEMS 1. a. 5 Kg: 100 mL/Kg/d x 5 Kg = 500 mL/d OR 4 mL/Kg/hr x 5 Kg = 20 mL/hr b. 30 Kg: (100x10)+(50x10)+(20x10) = 1700 mL/d OR (4x10)+(2x10)+(1x10) = 70 mL/hr c. 50 Kg: (100x10)+(50x10)+(20x30) = 2100 mL/d OR (4x10)+(2x10)+(1x30) = 90 mL/hr So why isn’t the rate for 30 Kg six times the rate as for 5 Kg? And why isn’t the rate for 50 Kg ten times the rate as for 5 Kg? (Because basal metabolic rate per Kg declines with age.) 2. COMPOSITION: D5 ¼ NS + 20 mEq/L K+ regardless of age or weight (based on metabolic rate, not on age or weight). 3. Rather than use a rule about urine output, let’s calculate what urine output is expected a. First step: Urine output should not equal intake; intake needs also to cover insensible losses. b. Second step: estimate urine output 1) The key is to recognize urinary losses as 50% of maintenance, presuming basal conditions and SG of 1.010. a) Maintenance = [(100x10) + (50x5)] = 1250 ml/d i) 50% of 1250 ml/d = 625 ml/d 2) If you prefer to think of urine output in ml/Kg/hr, you can try to use a “rule,” but no rule is particularly helpful, since urine output (like the amount of maintenance fluid) is not linearly related to body weight. SO could calculate what it should be by expressing maintenance in ml/Kg/hr and calculating 50% of that: a) Urine: 2 ml/Kg/hr for first 10 Kg; 1 ml/Kg/hr from 10 to20 Kg; 0.5 ml/Kg/hr above 20 Kg b) So maintenance here = [(2x10) + (1x5)] = 25 ml/hr i) 25 ml/hr @15Kg = 1.7 ml/Kg/hr 3) Whatever way you do it, the child's urine output is not far off (particularly if the SG is a little over 1.010): a) The child is not oliguric. b) Output should NOT equal intake (because of insensible losses). c) Thank you for the consultation. 4. a. Diagnosis: Acute post-streptococcal glomerulonephritis b. AMOUNT: Maintenance is [(100x10) + (50x10) + (20x1)] = 1520 ml/d, of which half is needed for insensible losses (approximately 760 ml/d) and half for urine formation—if child is making urine. So give 760 ml/d plus, if the child is not totally anuric, enough additional fluid to replace urine output ml for ml (i.e., as an ongoing loss). If the child can drink, this can be done PO by writing an order for fluid restriction If the child cannot drink, then give using IVF c. COMPOSITION: If po, give an electrolyte free solution such as ginger ale, water, etc (remember that insensible losses have minimal electrolytes). NOTE: To maintain basal conditions as much as possible and minimize endogenous protein breakdown, need an electrolyte-free, protein-free source of calories; a favorite is hard candy ("sour balls"). If IV, give D5W which wil provide both fluids and non-protein calories 12 ANSWERS TO THE PROBLEMS 5. You could consider his lack of fluids in the last 8 hours to be a “deficit,” but you could also think of it as simply being behind on maintenance, understanding that maintenance requirements do not need to be met continuously at an even hourly rate. You do not replace your own maintenance losses continuously, and the convention of providing maintenance fluid and electrolytes at a continuous rate in the hospital is simply for staff convenience. When you think about deficits, you likely have a knee-jerk response of wanting to provide a bolus. Boluses are used to restore intravascular volume rapidly; they contain not only a large amount of water but also a large amount of sodium, as they are necessarily comparable to serum concentrations (to avoid fluid shifts). Therefore, boluses should be reserved for individuals with evidence of circulatory compromise, such as tachycardia, hypotension, or delayed capillary refill time—none of which would be expected in this child. a. AMOUNT: 1) 8 hours of maintenance fluid plus ongoing maintenance needs a) Maintenance = [(100x10)+(50x3)] = 1150 ml/d or [(4x10)+(2x3)] = 46 ml/hr b) 8 hours of maintenance not received = 8x46 = 368 ml b. COMPOSITION: D5 ¼ NS + 20 mEq/L K+ c. RATE: 1) Could give the additional 368 ml in, say, 4 hours (92 ml/hr) added to maintenance: 92+46=138 ml/hr x 4. Then you would return to maintenance rate, 46 ml/hr 2) OR could replace deficit in 6 hours (368/6=61) along with maintenance (61 + 46 = 107 ml/hr) followed by maintenance (46 ml/hr). 3) NOTE: AMOUNT and COMPOSITION are straightforward here; choices come in selecting rate. 6. a. Pyloric stenosis. There is evidence of greater malnutrition than is usually seen with GE reflux, and the electrolytes indicate a profuse loss of gastric fluid, more suggestive of vomiting than of mild regurgitation. (“Projectile vomiting” is a clue, too.) b. Before surgery is performed, medical management needs to assure restoration of circulating volume and return to normal electrolyte balance: Assess dehydration at 10% = 3.4 Kg. Phase I: Resuscitation: Bolus: 20 mL/Kg (=68 mL) of normal saline (Even a fan of Ringer's lactate like me would use normal saline in this situation, because of the chloride deficit!). Phase II: Deficit: Since 20mL/Kg = 2% body weight, an 8% deficit remains. The easiest way to replace it is to give 1% (10mL/Kg) per hour for 8 hours (10 mL/kg/hr = 34 mL) with D 5 ½ NS + 20-30 mEq/L KCl. The hypokalemia will resolve along with the alkalosis. Phase III: Maintenance: You can either piggy-back the maintenance (4 mL/kg/hr =~14 mL/hr of D5 ¼ NS+20mEq/L KCl) along with the deficit or replace deficit and then address maintenance. To avoid worsening the hyponatremia, it is preferable to replace the deficit first, then give maintenance. If you choose to do it that way, note that you are 8 hours behind (like problem #5), so you would give 24 hours worth in 16 hours: 24/16 = 1½ x maintenance rate = 21 mL/hr x 16 hours; then 14 mL/hr. 1) Only when volume is restored and electrolytes are normal should the pyloromyotomy be performed and the malnutrition addressed. 2) Consider child moderately dehydrated clinically (10%) even though the weight discrepancy between what he should weigh and what he does way is much more than 10%. The reason for the greater discrepancy is the lack of subcutaneous fat: ie, more than water is involved. You only need to resolve the dehydration prior to surgery. The rest will be accomplished through nutrition post-operatively. 3) An error commonly made is to give the bolus and then proceed to maintenance without restoring the 8% remaining deficit. Note that you will not catch up by giving some multiple of maintenance and that the composition of the fluid needed to replace the deficit contains more sodium than does the maintenance solution. 13 FLUID & ELECTROLYTES: TAKE HOME MESSAGES 1. When planning to rehydrate a dehydrated child, it is easiest if you consider separately the a. Fluid (ie, amount of water) vs. Electrolytes (ie, composition of fluid) 1) Estimate the amount of fluid first, then think about composition b. Deficit vs. Maintenance vs. Ongoing Losses 2. For maintenance, both fluids AND lytes are based on metabolic rate-- not directly to weight. Rule of thumb is as follows: -Amount: Weight ml/Kg/d or ml/Kg/hr Example (ml/Kg/d) 0- 10 Kg 100 4 7 Kg: 100x7 = 700 11-20 Kg 50 2 15 Kg: 100x10 + 50x5 =1250 >20 Kg 20 1 25 Kg: 100x10 + 50x10 + 20x5 = 1600 -Composition: always ¼ NS + 20 mEq/L K+ (either as KCl, KPhos, or Kacetate). 3. Assessment of dehydration: The rule of 5-10-15 (mild dehydration = 5%, moderate dehydration = 10%, severe dehydration = 15%) applies to infants. For adolescents and adults, the rule is 3-6-9 (mild dehydration = 3%, moderate dehydration = 5-6%, severe dehydration = 7-9%). (For young school-age children, the rule is somewhere in between, but, in practice, we often ignore the distinction from infants and use 5-10-15 in this age group.) 4. Front load your fluid replacement. This is especially true in severely dehydrated kids 5. Consider Oral Rehydration for kids who are mild-moderately dehydrated 6. "Fluid resuscitation:" Note that 20 ml/Kg = 2%. Implications: if you estimate an infants's degree of dehydration to be 15% (and you are right), he will not "normalize" with 20 ml/Kg but will improve to 13% -- and still be tachycardic, etc. To rapidly return him to cardiovascular sufficiency, he will need 3 boluses of 20 ml/Kg (as recommended in PALS). 7. Composition of rehydration fluid: To correct isotonic dehydration (i.e., serum [Na+ ] is normal), calculations will result in: a bolus of Ringer's lactate or normal saline; followed by several hours (6-8) of D5 ½ NS + 20 mEq/L KAcetate; followed by D5 ¼ NS + 20 mEq/L KAcetate. 8. On-going losses: If likely to be significant, measure and replace. 9. Monitoring rehydration: The things we forget most often are the simple ones (which are also the most helpful): e.g., the physical examination (to see if the signs of dehydration have improved); urine specific gravity. 14 Appendix: What’s wrong with 1 ½ time maintenance? A child comes in with moderate (10%) dehydration. You start D5 ½ NS at 1 ½ time maintenance, thinking that this will be a good estimate of maintenance + fix his dehydration. The next morning, the attending is unhappy when you mention “1 ½ times maintenance.” Is it just semantics? Won’t this usually work out the same as if you had calculated it? No. Look at the two examples below: 10 kg child who is 10% dehydrated from acute diarrhea Water Sodium Maintenance ~1000 mL 30 mEq Deficit Total (4:2:1 rule = 4 ml/hr * 10 kg * 24 hr in a day) (based on usual maintenance needs Table 3 ) 1000 mL 80 mEq (10% of 10 kg) (based on electrolyte losses Table 7) 2000 mL 110 mEq Na Using simply 1 ½ times maintenance: Using D5 ¼ 1440 mL Using D5 ½ 1440 mL 55 mEq Na 110 mEq Na If you use 1 ½ time maintenance, you will not give enough water (using D5 ¼ would also not give enough salt) 40 kg child who is 5% dehydrated from acute diarrhea Water Sodium Maintenance ~1900 mL 57 mEq Deficit Total (4:2:1 rule) (based on usual maintenance needs Table 3 ) 2000 mL 160 mEq (5% of 40 kg) (based on electrolyte losses Table 7) 3900 mL 217 mEq Na Using simply 1 ½ times maintenance: Using D5 ¼ 2880 mL Using D5 ½ 2880 mL 110 mEq Na 220 mEq Na If you use 1 ½ time maintenance, you will not give enough water (using D5 ¼ would also not give enough salt) 15