Infection Control, Vital Signs, Oxygen & Medical Emergencies
advertisement

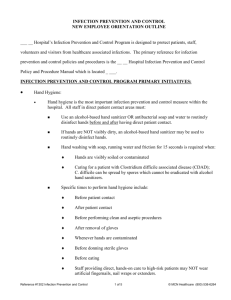
Infection Control, Vital Signs, Oxygen & Medical Emergencies Infection Control • Microorganisms • Infectious Disease • Chain of Infection • Nosocomial Infection • Disease Control • Environment Microorganisms that cause disease Bacteria Viruses Fungi Protozoa Can grow in or on an animal or plant and cause diseases. Host: animal or plant that provides life support to another organism. Disease: Any change from the normal structure or function in the human body. Infection: Growth of a microorganism on or in a host. Disease • Disease occurs only when the microorganism causes injury to the host Pathogen A disease producing microorganism. Multiply in large numbers and cause an obstruction Cause tissue damage Secrete substance that produce effects in the body Exotoxins ( high body temp, nausea, vomiting) Bacteria Protozoan Viruses Fungi 6 Steps of Infection Encounter Entry Spread Multiplication Damage Outcome Chain of Infection Host Infectious Microorganism Mode of Transmission Vector/ Fomite Reservoir Nosocomial Infections: Infections originating in the hospital; an infection not present before admittance to the hospital. Iatrogenic Infection Compromised Patients Patient Flora Hospital Environment Bloodborne Pathogens Universal Precautions Since there is no way you can know if a person is infected, you should ALWAYS use universal precautions: Wash your hands Wear gloves Handle sharp objects carefully Properly clean all spills Wear mask, eye protection, and apron if splashing is a possibility. Airborne Precautions Patients infected with pathogens that remain suspended in air for long periods on aerosol droplets or dust. TB, Chickenpox, Measles Respiratory protection must be worn when entering pt room. Pt should wear mask. Droplet Precautions Patients infected with pathogens that disseminate through large particulate droplets expelled from coughing, sneezing, or even talking. Rubella, Mumps, Influenza Surgical mask must be worn when within 3 feet of the pt. Pt should wear a mask. Contact Precautions Patients infected with pathogens that spread by direct contact with the pt or by indirect contact with a contaminated object (bedrail, pt dressing). Methicillin-resistant staphylococcus aureus (MRSA), Hepatitis A, Varicella, Flesh-eating Virus All PPE should be used and equipment must be disinfected after use. Controlling the spread of Disease • Chemotherapy • Immunization • Asepsis – Medical – Surgical • Disinfectants Physical Methods of Controlling Diseases • Handwashing • Standard Precautions – Gloving – Gowns – Face masks – Eyewear Handwashing • Single most important means of preventing the spread of infection. • 7 to 8 minutes of washing to remove the microbes present, depending on the number present. • Most effective portion of handwashing is the mechanical action of rubbing the hands together. Types of Nosocomial Infections Iatrogenic Infection – related to physician activities Compromised Patients - weakened resistance; immunosuppressed Patient Flora - microbes in healthy people Contaminated Hospital Environment Bloodborne Pathogens – Hepatitis B and HIV Vital Signs Indication of Homeostasis Primary Mechanisms Heart beat Blood pressure Body temperature Respiratory rate Electrolyte balance Physical assessment include measurement of vital signs Body Temperature Pulse Respiration Blood Pressure Mental Status Body Temperature Normal average body temperature: 98.6 F Humans can survive between 106 F and 93.2 F. Hypothermia Hyperthermia Measuring Body Temperature Oral Rectal Axillary Tympanic Pulse Pulse rate: Adult = 60 to 100 beats per minute Children under 10 = 70 to 120 beats per minute Tachycardia Bradycardia Respiratory Rate Breaths per minute: Adult = 12 to 20 Children under 10 = 20 to 30 per min Tachypnea Bradypena Dyspnea Apnea Pulse Oximeter • Normal Pulse Oximeter = 95% to 100% Blood Pressure • Blood Pressure • Systolic pressure = 95-140 mmHg • Diastolic pressure = 60-90 mmHg • Hypertension • Hypotension Oxygen Oxygen constitutes 21% of atmospheric gases If O2 levels in the body drop below 21% homeostasis is altered. Hypoxia: Inadequate amount of oxygen at the cellular level. Oxygen Devices Nasal Cannula Masks Nonrebreathing mask Aerosol mask Air-entrainment mask Tent and Oxyhood Chest Tubes and Lines • Endotracheal Tube (ET) – Ventilator • Chest Tubes • Nasogastric tube (NG) • Central Lines Medical Emergencies Definition: Sudden change in medical status requiring immediate action. For RT’s medical emergencies are rare, however as medical personnel we must be prepared to recognize emergencies. Anaphylactic Reaction An immune response to foreign material Bronchospasm – wheezing and edema in the throat and lungs Can lead to shock Requires prompt recognition and treatment from the technologist Why do RT’s care about Anaphylactic RXN’s….? General Priorities Ensure an open airway Control Bleeding Take Measures to Prevent shock Attend to wounds or fractures Appropriately Provide emotional support Continually reevaluate and follow up ABC • A = Air Way • B = Breathing • C = Circulation CPR • C = Cardio • P = Pulmonary • R = Respiration • Must be certified for the “Health Care Provider” • Cards good for 2 years are available. • In your work environment: • Emergency assistance protocol (how to get help) • Emergency Cart/Crash Cart Location Level of Consciousness: ALOC Altered Level Of Consciousness Anaphylactic Shock: vasogenic shock Hypoglycemic/Hyperglycemia NPO – Nothing by Mouth Pallor = paleness; absence of skin coloration Shock = failure of the circulatory system CPR = cardiopulmonary resuscitation For program must be for Health Care Provider Stroke = Cerebrovascular Accident (brain) Heart Attack = Myocardial Infarct (heart) N/V = Nausea & Vomiting Epistaxis = nosebleed Vertigo = dizziness Syncope = fainting Hemorrhage = bleeding outside a vessel