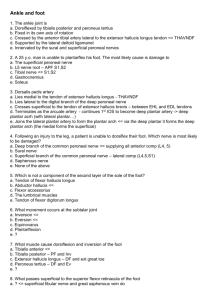
Lower limb entrapment
advertisement

Lateral femoral cutaneous nerve (meralgia paresthetica) syndrome of burning, tingling, numbness, and pain in the distribution of the LFCN Anatomy o From posterior roots lumbar plexus (L2,3) o Emerges from lateral border of psoas, travels under iliacus fascia o exits the pelvis to the subcutaneous plane of the thigh at a sharp angle just inferior to the origin of the inguinal ligament at the anterior superior iliac spine. Variations (Dellon PRS 1997) 1. Type A - course across the iliac crest posterior to the ASIS (4%). Most superficial of all types 2. Type B - ensheathed in the inguinal ligament just medial to the ASIS (27%) 3. Type C - ensheathed in the tendinous origin of the sartorius muscle medial to the ASIS (23%) 4. Type D - found in an interval in between the sartorius muscle and the iliopsoas muscle deep to the inguinal ligament (26%) 5. Type E - found in the most medial position on top of the iliopsoas muscle, contributing the femoral branch to the genitofemoral nerve (type E) (20%). Most medial of all types Types A,B and C most prone to compression Compression of this nerve is more common in obese individuals. Standing and hip extension aggravate the symptoms in many patients. A Tinel's sign may occasionally be present over the nerve at the inguinal ligament that radiates to the distribution of the nerve in the anterolateral thigh. Electrodiagnostic tests are not commonly used for this condition although in ANZ J Surg 2004 – somatosensory evoked potentials may predict outcome. Nonoperative management Posture modification Operative 8-10cm incision is placed transversely just inferior to the inguinal ligament from the anterior superior iliac spine to a point lateral to the femoral triangle fascia of the sartorius muscle is released transversely, and the lateral femoral cutaneous nerve is identified and followed superiorly overlying inguinal ligament is transected to decompress the nerve. Variable surgical results in literature If surgical decompression fails to relieve symptoms, consider neurectomy nerve is first blocked with a local anesthetic so that the patient can agree that numbness improves their symptoms. The associated nerve is identified through a retroperitoneal approach and a neurectomy of the nerve performed in the retroperitoneal area. Recommended site for iliac bone graft harvest to avoid the LFCN Common Peroneal nerve most common compression neuropathy of the lower extremity entrapment of the common peroneal nerve at the neck of the fibula and presents clinically with the characteristic foot drop and paresthesiae on the anterolateral aspect of the distal leg and dorsum of the foot. Slight predominance in males 10% bilateral peroneal tunnel- fibro-osseous tunnel formed by the superficial and deep heads of the peroneus longus muscle. deep peroneal branch supplies the tibialis anterior, extensor digitorum longus, extensor digitorum brevis, peroneus tertius, and extensor hallucis longus terminates as a sensory nerve providing sensation between the great and the second toes dorsally superficial peroneal nerve branch innervates the peroneus longus and brevis muscles and terminates as the sensory nerve, providing sensation to the anterolateral skin of the leg and the dorsum of the foot. Aetiology 1. Ankle inversion - tenses the peroneus longus at the fibular neck, thus severely compressing and producing traction on the peroneal nerve. 2. Traction at the hip (hip replacement) is more like to damage peroneal compared to tibial component of sciatic nerve: 1. peroneal nerve division of the sciatic nerve is relatively fixed proximally at the sciatic notch and distally at the fibular neck 2. peroneal nerve component has fewer and larger fascicles with limited supportive tissues, in contrast to the tibial nerve 3. competitive athletes 4. Space occupying lesions – ganglia, bony spurs 5. External pressure – prolonged bed rest, calf compression devices Nerve damage is a combination of direct compression at the peroneal tunnel, and second is the traction injury, which not only damages the nerve but also ruptures the vasa nervorum, causing bleeding and ischemia to the nerve. Clinical Lower back assessment straight leg test (Lasegue test) is common in lumbar radiculopathy and sciatic nerve lesions but is uncommon in peroneal neuropathy Neurophysiological studies (EMG and nerve conduction studies) are extremely important in the investigation of the peroneal nerve. Operative curvilinear incision over the peroneal tunnel. Avoid injury to the posterior femoral cutaneous nerve as it crosses superficial to the peroneal nerve and the lateral sural nerve. Complete decompression requires i) release of the overlying fascia proximal to the peroneal tunnel ii) opening the fascia of the peroneus longus and following the nerve between the deep and superficial heads of the peroneus longus, iii) release of the fascia of the adjacent extensor digitorum longus. protect the recurrent branch of the peroneal nerve innervating the tibialis anterior, which takes an upward route in contrast to the rest of the nerve. It can be easily damaged during the dissection Superficial peroneal nerve (superficial peroneal tunnel syndrome) symptoms produced by this syndrome are purely sensory: pain and paresthesiae on the anterolateral aspect of the leg and foot. site of compression is approximately 10 cm proximal to the lateral malleolus over the anterolateral aspect of the leg - superficial nerve pierces the fascia and becomes a cutaneous nerve at this point 10% of patients with superficial nerve entrapment have a chronic compartment syndrome Provocation test - plantar flexing the ankle passively and simultaneously inverting the ankle with percussion on the nerve recommended treatment is complete release of the superficial peroneal tunnel close to the anterior intermuscular septum Deep Peroneal nerve (anterior tarsal tunnel syndrome) compressed by i) extensor retinaculum and its specific contributions by the cruciate ligament and the medial inferior branch of the cruciate ligament ii) tendon of the extensor hallucis longus iii) hypertrophied extensor hallucis brevis muscle with a well-defined fibrous band in its deeper layers Patients usually complain of aching or tightness at the ankle and dorsum of the foot and numbness in the first dorsal web space. Conservative measures, such as avoiding shoe straps on the dorsum of the foot or high heels, are advocated initially. If symptoms persist, a diagnostic lignocaine injection can provide prognosis of surgical decompression Decompression of the nerve includes release of the fascia overlying the nerve and the dorsalis pedis artery to the level of the inferomedial aspect of the extensor retinaculum. It would be prudent to excise the extensor hallucis brevis overlying the nerve. Tibial nerve (tarsal tunnel syndrome) Tarsal tunnel o Anterior – medial malleolus o Posterior – calcaneus o Floor - tendons of the tibialis posterior, the flexor digitorum longus, and the flexor hallucis longus o Roof – flexor retinaculum tibial nerve divides into the medial and lateral plantar nerves within 1 cm of the malleolar-calcaneal axis in 90% medial and lateral plantar nerves proceed through individual tunnels separated by a septum that takes its origin from the calcaneus or the fibro-osseous canal of the flexor hallucis longus tendon Within these tunnels, the roof is formed by the origin of the abductor hallucis muscle over the medial plantar nerve and the origin of the plantar aponeurosis over the lateral plantar nerve. Both of these fibrous structures originate from the calcaneus Clinical o numbness, tingling, cramping, and a burning plantar pain at the metatarsal heads and less likely at the heel. Classically, the symptoms are aggravated by weight bearing and improve with rest and elevation of the foot. o Nerve conduction studies (NCS) are often diagnostic but a normal NCS does not exclude the diagnosis Operative o longitudinal incision over the neurovascular bundle in the interval between the medial malleolus and the calcaneus. o extends from a point 3 cm proximal to the malleolus to the medial aspect of the foot but not extending to plantar skin. o Need to decompress flexor retinaculum and abductor fascia over the individual tunnels. Common plantar digital nerves (Morton's neuroma) o Not a true neuroma o Morton’s description was nerve to 4th web space but 3rd is more common o nerve to the third web space is formed by a branch from the medial plantar nerve and from the lateral plantar nerve. o travels on the deep aspect of the intermetatarsal ligament and divides to form the proper digital nerves to the lateral aspect of the third and medial aspect of the fourth toes o present with a shooting pain between the third and fourth toes with weight bearing; the pain is aggravated by physical activity and relieved by elevation. o Narrow and high-heeled footwear has been implicated in the etiology of this condition, which explains the female predominance of this compressive neuropathy. o Manual compression of the first and fifth metatarsal heads by the examiner's hand usually provokes the symptoms of pain, as does pressure between the third and fourth toes. o Nerve conduction tests are not useful; however, a diagnostic nerve block that relieves symptoms confirms the diagnosis. Nonoperative o includes the avoidance of tight and high-heeled footwear and the use of custom orthotics to unload the metatarsal heads. o Corticosteroids may be useful as a temporizing technique, although they do not always lead to complete resolution of symptoms o When conservative measures are unsuccessful, surgery is considered. Operative o In contrast to other compressive neuropathies, surgical management of Morton's neuroma is controversial. o The controversial issues are dorsal versus plantar approach and decompression versus resection of the nerve o Historically, the nerve was decompressed by resecting the head of the metatarsal and occasionally the nerve as described by Morton o Others also recommended resection of the common plantar digital nerve and reflection to a proximal location o dorsal approach may be used in primary cases for patients with symptoms that are not considered incapacitating. Decompression by dividing the intermetatarsal ligament and intraneural neurolysis of the common plantar digital nerve at the dorsal web space o In severe cases or failed dorsal approach - resection of the common plantar digital nerve is performed through a plantar approach with transposition of the proximal end into the deep muscular layer of the foot. o In most series, inferior results occur in patients with bilateral procedures or involving more than one web space.