Total Shoulder Replacement Physiotherapy Protocol
advertisement
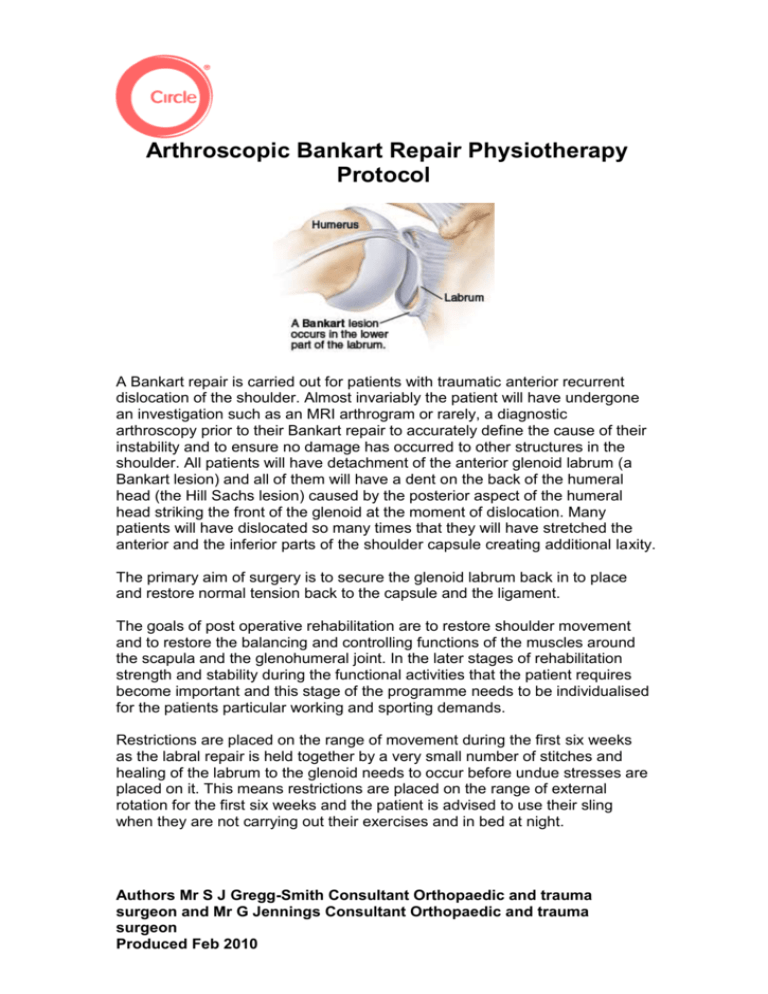
Arthroscopic Bankart Repair Physiotherapy Protocol A Bankart repair is carried out for patients with traumatic anterior recurrent dislocation of the shoulder. Almost invariably the patient will have undergone an investigation such as an MRI arthrogram or rarely, a diagnostic arthroscopy prior to their Bankart repair to accurately define the cause of their instability and to ensure no damage has occurred to other structures in the shoulder. All patients will have detachment of the anterior glenoid labrum (a Bankart lesion) and all of them will have a dent on the back of the humeral head (the Hill Sachs lesion) caused by the posterior aspect of the humeral head striking the front of the glenoid at the moment of dislocation. Many patients will have dislocated so many times that they will have stretched the anterior and the inferior parts of the shoulder capsule creating additional laxity. The primary aim of surgery is to secure the glenoid labrum back in to place and restore normal tension back to the capsule and the ligament. The goals of post operative rehabilitation are to restore shoulder movement and to restore the balancing and controlling functions of the muscles around the scapula and the glenohumeral joint. In the later stages of rehabilitation strength and stability during the functional activities that the patient requires become important and this stage of the programme needs to be individualised for the patients particular working and sporting demands. Restrictions are placed on the range of movement during the first six weeks as the labral repair is held together by a very small number of stitches and healing of the labrum to the glenoid needs to occur before undue stresses are placed on it. This means restrictions are placed on the range of external rotation for the first six weeks and the patient is advised to use their sling when they are not carrying out their exercises and in bed at night. Authors Mr S J Gregg-Smith Consultant Orthopaedic and trauma surgeon and Mr G Jennings Consultant Orthopaedic and trauma surgeon Produced Feb 2010 Post-Op Physiotherapy for Arthroscopic Bankart Repairs NB this protocol only applies to patients who have undergone arthroscopic Bankart repairs. Please see the relevant protocol for patients who have undergone open procedures. Phase 1 (Immediately Post-Op to 2 weeks) The shoulder is rested in a sling for approximately for 4 weeks following surgery to allow the labrum and ligaments to heal. Exercises: 1. Postural advice especially sleeping position 2. Passive shoulder flexion (with arm in internal rotation) no more than 90º 3. Passive external rotation to neutral 4. Shoulder girdle range of movement and setting exercises 5. Postural correction out of the sling 6. Neck, hand and elbow exercises to maintain range of movement 7. Scar massage when stitches out Aims at 2 weeks: Passive shoulder flexion to 90º Passive shoulder external rotation to neutral Decrease pain and swelling with use of painkillers/anti-inflammatories NB: avoid combined abduction and external rotation for 6 weeks Phase 2 (weeks 3-4) Exercises: 1. Isometric flexion, abduction, external and internal rotation, as pain allows. 2. Active-assisted shoulder flexion (with arm in neutral or internal rotation) to no more than 130º 3. Active-assisted external rotation to 20º. 8. Shoulder girdle range of movement and setting exercises 4. Serratus anterior isometric 5. Scar massage when stitches removed Aims at 4 weeks: Wean off sling during day Active-assisted shoulder flexion more than 130º Active-assisted shoulder external rotation to 20º NB: avoid combined abduction and external rotation for 6 weeks Authors Mr S J Gregg-Smith Consultant Orthopaedic and trauma surgeon and Mr G Jennings Consultant Orthopaedic and trauma surgeon Produced Feb 2010 Phase 3 (weeks 5-12) Exercises: 1. Active shoulder flexion (with arm in neutral or internal rotation until six weeks) 2. Active shoulder external rotation (working to full range after six weeks) 3. Active assisted shoulder abduction (in internal rotation until six weeks) 4. Hand behind back exercises 5. Unrestricted active range of movement after six weeks 6. Hydrotherapy if patient not progressing 7. Core stability exercises e.g. superman 8. Dynamic trunk stability Aims at 12 weeks: Wean off sling if not done so already Full range of movement Good scapulothoracic control Authors Mr S J Gregg-Smith Consultant Orthopaedic and trauma surgeon and Mr G Jennings Consultant Orthopaedic and trauma surgeon Produced Feb 2010