Medical University of South Carolina
advertisement

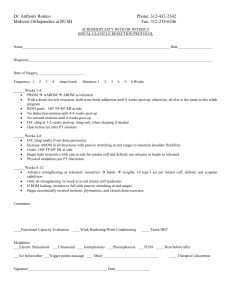
Clinical Pathway for TSA/HHR Patients Shane K. Woolf, MD James R. Demarco, MD H. Del Schutte, MD Objective: I. To create an evidence-based clinical pathway for the evaluation and care of patients who present with degenerative disease of the gleno-humeral joint and are candidates for surgical reconstruction. Preoperative evaluation a. Imaging i. Plain radiographs 1. Grashey AP view 2. Axillary lateral view 3. Supraspinatous outlet view 4. External/Internal rotation AP views, possibly ii. CT scan 1. If any concern for posterior glenoid wear or gleno-humeral deformity iii. MRI 1. If need to evaluate status of rotator cuff tendons or muscle belly 2. Aids in decision for HHR vs TSA b. Outcomes Assessment i. SANE ii. VAS pain scale iii. Simple Shoulder Test iv. ASES?? c. Lab Studies i. EKG if over 50 ii. CXR if indicated iii. BMP iv. CBC II. v. Coags, if indicated vi. Urinalysis, culture + sensitivity 1. Must be done within 5 days of surgery, if possible 2. Call in Cipro 250 mg po bid x 5 days or Bactrim DS I po bid x 5 days if positive cultures, leuk esterase or nitrites vii. Type and screen in holding viii. If revision case: 1. Infection labs (ESR, CRP, CBC with manual diff) 2. Nutrition labs (transferrin, prealbumin, absolute lymphocyte count) 3. Joint aspirate if indicated a. Cell count, gram stain b. Aerobic/anaerobic cultures d. Medical Evaluation and Preoperative Optimization i. Notify Hospitalist when scheduled 1. Decision for preop anesthesia and ortho workup ii. PCP letter of medical clearance (in chart before surgery) iii. No preop workup if otherwise healthy??? iv. Stop ASA, NSAIAs, Plavix by 7 days preop v. Stop coumadin by 5 days preop, INR < 1.5 for surgery, preop heparinization on case-by-case basis e. Dental Evaluation i. Indicated in those with poor dentition, loose teeth, caries ii. Treat oral pathology before implants in shoulder Perioperative Management a. Holding room i. Confirm labwork and studies are complete and satisfactory ii. ISB or paravertebral block by anesthesia in all eligible candidates 1. Indwelling pump OK, if paravertrebral block 2. Placement within 1 hour of OR iii. Cefazolin 2 gm IV (or Vancomycin 1 gm IV OCTOR if PCN/cephalosporin allergy more than rash/hives) iv. TED stockings and SCDs placed in holding v. Wash operative extremity/site with chlorhexidine and rinse with alcohol in holding vi. Initial operative site, confirmed by consent form and verbally b. Operating room i. Beachchair position ii. Foley catheter on request only iii. Surgeon preference for setup iv. Surgeon preference and indications for implants, technique v. Simple sling + ABDs in axilla when finished c. PACU i. May raise head of bed to tolerance ii. Remain in sling iii. Neurovascular checks q 30 min x 2 hours to operative extremity 1. Capillary refill 2. Grip, finger abduction, thumb extension, gentle elbow flexion and extension 3. Forearm, index and small finger sensation to light touch iv. Shoulder precautions 1. No external rotation > neutral 2. No active or resisted internal rotation 3. May forward flex to 90 degrees v. Postoperative imaging 1. Neutral and internally rotated AP views d. Pain management i. Regional block +/- indwelling catheter ii. Morphine PCA pump iii. May change to oral pain meds (oxycodone or Percocet, NOT oxycontin) with IV breakthough once taking po well e. Arrival to JRU bed and HD #1 i. General patient care 1. MIVF until taking >300 cc fluids without nausea 2. Pain control as above 3. Reinforce dressing as needed 4. Must have assistance 1st 24 hrs whenever getting out of bed 5. Foley removed once able to get out of bed to commode or toilet 6. SCDS or Foot pumps whenever in bed prior to d/c 7. TEDs until mobilized 8. Shoulder precautions as above 9. Drain removed on POD#1 unless > 30 cc/shift ii. Patient positioning 1. Elevate HOB as needed for comfort 2. Keep hand above elbow 3. Pillow under forearm to support hand and slightly flex shoulder forward iii. Physical Therapy 1. Begin POD #1 a. Mobilization and transfers i. Assess safety ii. Fall precautions b. Reinforce shoulder precautions c. Initiate protected (‘helper hand’) pendulums d. Protected supine forward flexion (overhead elevation) and rotation from chest wall to neutral position 2. TSA/HHR rehab protocol a. See Appendix A b. Modify as indicated iv. Occupational Therapy III. 1. Begin POD #1 a. ADL assistance b. Don/doff clothing safely c. Assess home status v. Perioperative Medications 1. Antibiotics a. 1st 24 hrs b. Cefazolin or Vancomycin 2. DVT prophylaxis a. LMWH i. Begin by 12-18 hours postop ii. Continue until mobilized/ambulatory b. Continue LMWH in high risk patients i. Previous DVT/PE ii. Previous extremity surgery or trauma iii. Age > 70 iv. Protein C/S or Antithrombin III deficiency v. Hx of Cancer vi. HX PVD or phlebitis vii. Slow to mobilize viii. If smoker and on HRT ix. > 2 risk factors Lyman et al, CORR 2006 3. General a. MVI + iron b. Stool softener 7 West Bowel protocol vi. Labwork 1. POD #1 a. BMP b. Hemoglobin/hematocrit 2. POD #2 a. Only if indicated Postoperative Management a. Discharge from hospital i. Criteria 1. Transfer and ambulate with minimal to no assistance 2. Taking po and voiding 3. Pain control adequate 4. No apparent postop issues/complications ii. Copy of patient instructions to be placed in folder 1. See Appendix B iii. Medications 1. Pain meds (oxycodone) 2. MVI + iron 3. stool softener 4. LMWH x 10 days (if indicated) iv. Physical therapy 1. outpatient vs HHPT a. Prescription in folder b. TSA/HHR protocol 2. sling x 4-6 weeks, MD directed 3. Shoulder precautions v. Will need antibiotics for future dental and surgical procedures b. Follow-up i. Routine follow-up schedule 1. ~ 2 weeks - 1st visit a. No radiographs unless an issue arises b. Sutures/staples removed, wide steri-strips applied (no benzoin) c. May drive at 4-6 weeks only if no pain off pain meds i. Explain liability risk to patient if accident occurs ii. Risk of disrupting repair 2. 6 weeks – 2nd visit a. Plain radiographs i. Grashey AP ii. Axillary lateral iii. External rotation/internal rotation views b. d/c sling c. continue PT 3. 3-4 months – 3rd visit a. No radiographs unless indicated b. PT only as needed 4. 6 months a. Radiographs i. Grashey AP ii. Axillary lateral iii. External rotation/internal rotation views b. Activity as tolerated 5. 12 months and every year thereafter a. Radiographs as above ii. Outcomes Measures 1. Administer at 4, 6, 12 months 2. Administer annually after 12 month anniversary Appendix A. Total Shoulder Arthroplasty/ Humeral Head Replacement Rehabilitation Protocol Goals: Pain control Edema control Protect subscapularis, rotator interval, and/or rotator cuff repairs Gradual restoration of motion Return to effective use of limb for ADLs Restore shoulder strength and function Phase I (0-4 weeks postop) Sling immobilization except for washing and clothing changes x 4-6 weeks Exercises 5-6 times/day for 10-15 minutes each session Codmans/Pendulum exercises using ‘helper hand’ for support Wrist, Hand AROM Elbow AROM (***wait 2-3 weeks if biceps tenotomy/tenodesis) Gripping exercises Limits: FF-AAROM (supine)-limited to 90o ER to 0o only IR to chest wall Sub-maximal, pain-free deltoid, trapezius isometrics in neutral Modalities as needed Phase II (4-6 weeks) Continue sling whenever out of home in public to protect repairs Continue FF-AAROM (wand/pulleys) ER - AAROM to 30º only FF – begin supine AROM Manual scapular stabilization exercises Begin pain-free ER isometrics in modified neutral Modalities as needed Phase III (6-8 weeks) D/C sling Begin use of the limb for ADLs as tolerated except no lifting/carrying 6 weeks - begin Biceps/Triceps strengthening Progress scapular strengthening in protective arcs Begin limited isotonic IR/ER strengthening in modified neutral Begin seated FF in plane of scapula Begin AROM for ER Continue to increase FF AROM/PROM/AAROM Phase IV (8-10 weeks) Continue scapular strengthening Advance isotonic strengthening for deltoid, trapezius, biceps, triceps and latissimus as tolerated Begin general flexibility exercises at 10 weeks Phase V (10-16 weeks) Begin gentle progressive resistive exercises of deltoid and rotator cuff Restore shoulder flexibility Continue full upper extremity strengthening Appendix B. Patient Instructions After Shoulder Replacement Surgery 1. 2. 3. 4. 5. 6. 7. Apply ice for 20-30 minutes every 2 hours while awake for the first 48 hours after surgery. Pain medicine will be prescribed prior to discharge. Use the medicine, as directed, over the first 48 hours, then begin to taper your use. Remove the dressing on the 3rd day after surgery. If the sites are still moist, place a Band-Aid over the site until dry. If drainage continues contact your physician. Keep incisions dry for at least 5 days. After 5 days you may shower, but do not submerge incisions until discussed with your physician. When you shower do not rub the incision. Simply allow the water to wash over the site, and then pat it dry. A sling will be provided prior to discharge. Remove the sling 5 times each day to perform motion exercises. The sling should only be removed for exercises or while showering. Continue to use the sling for as long as your surgeon instructs, including during sleep. Keep a clean pad in your armpit while wearing the sling to prevent excessive sweating. Active motion of the elbow, wrist, and hand are permitted immediately. Active shoulder overhead reaching and lifting are NOT permitted yet! You may use the operated arm after surgery only for activities of daily living that do not require it to leave the side of the body (eg eating, drinking, bathing, writing, computer use, etc.) Five times each day you should perform Passive and ActiveAssisted Range of Motion exercises. For example, forward elevation and external rotation exercises should be performed with the non-operated arm used as the “therapist arm” controlling the motion of the operated arm. The operated arm should remain relaxed at all times. Twenty of each exercise should be performed five times per day. 8. Overhead Reach is helping to lift your stiff arm up as high as it will go. Stretching is the GOAL! To perform overhead reach, lie flat on your back, RELAX, grasp the wrist of your operated shoulder with the opposite hand. Using the power of your well arm, bring the other arm up as far as comfortable. Start by holding it for 10 seconds and then work up to where you can hold it for 30 seconds. Breathe slowly and deeply while the arm is moved. Repeat this stretch 20 times, trying to move the arm up a little higher each time. 9. Special Instructions: ***You must always take antibiotics before any major dental work (more than routine cleanings) or surgical procedures. Please notify your dentist, surgeon, or your orthopaedic surgeon if you need a prescription. 10. Please Call (843) 792-0404 for: Any Urgent Questions or Concerns o For medical emergencies call 911 Excessive redness of the incision Drainage of more than 4 days Fever of more than 101.5° Call to confirm a follow up appointment with your surgeon 7-10 days after surgery if not already scheduled