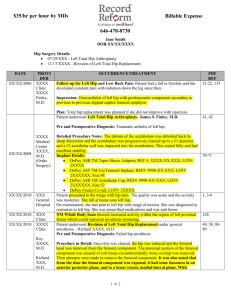
Humbert Templates
advertisement

Total Hip Replacement Anterolateral SURGEON: Edward T. Humbert, DO ASSISTANT: David Hodges, PA DATE OF PROCEDURE: ?? PREOPERATIVE DIAGNOSIS: Osteoarthritis of hip. POSTOPERATIVE DIAGNOSIS: Osteoarthritis of ?? hip. PROCEDURE PERFORMED: Total hip replacement. APPROACH: Anterolateral. COMPONENTS: ?? ESTIMATED BLOOD LOSS: ?? FLUIDS: ?? SPECIMENS: ?? We did discuss with this patient the benefits and complications of surgery, including infection, injuries to nerves, vessels and tendons, component loosening, component periprosthetic fractures, deep vein thrombosis, pulmonary embolisms, death, need for subsequent revision surgery, recurrent pain, recurrent limping, recurrent effusions and swelling, bleeding, as well as need for blood transfusions, leg length discrepancies and dislocations of components, were all discussed at length with this patient. After benefits and complications were discussed, the patient did opt for surgical intervention. PROCEDURE IN DETAIL: The patient was taken to the operative suite and the appropriate hip was prepped and draped in a sterile fashion in the lateral decubitus position. Once the hip was prepped and draped in a sterile fashion, an anterolateral approach was performed. A skin incision was made laterally over the hip and carried sharply down to subcutaneous tissues to the tensor fascia lata and IT band. This was then split in line with its fibers and anterior and posterior retractors were placed to expose the greater trochanteric region. The gluteus medius was then split in the anterior 20% and Bovie cautery was used to take a sleeve of tissue anteriorly while externally rotating the hip, then using a sharp knife, splitting down to the capsule and a portion of the gluteus minimus to the femoral head. Any remaining soft tissues were released with external rotation of the hip. Then protecting other soft tissues at all times, the femoral neck and femoral head were exposed with medial and lateral retractors and with external rotation and traction, the hip was dislocated. Using Hohmann retractors to protect the femoral neck, a saw was then used to make a femoral neck cut one fingerbreadth proximal to the lesser trochanter and the femoral head was removed. Anterior and posterior acetabular retractors were then placed with the knee back on the table and labrum was excised. An inferior blunt retractor was also placed. Resection of any soft tissue in the acetabulum was then performed. Once complete exposure of the acetabulum was identified, reaming was performed to appropriate size in 45 degrees of abduction, approximately 15-20 degrees of anteversion. The acetabular component was placed in approximately 45 degrees of abduction and 20 degrees of anteversion with an excellent peripheral rim fit and appropriate acetabular liner was then placed and interlocked with the ring lock mechanism, or if not needed was not placed with the metal on metal component. The cup was then checked with the Cobb elevator for stability anteriorly, posteriorly, inferiorly and superiorly. Once an excellent peripheral rim fit was identified, a blunt retractor was placed underneath the greater trochanteric region, the hip was externally rotated and the femoral neck was exposed with a femoral head elevator and medial Hohmann retractor. Broaching was then performed from a 5 up to an appropriate size. Trialing of femoral component with head size again was checked after hip reduction with full flexion, adduction and internal rotation to 60 degrees and showed good stability in this position as well as 30 degrees of extension and 20 degrees of external rotation. Once appropriate stability was obtained as well as relatively equal leg length in the lateral position, permanent components were then placed in the femoral canal and the appropriate head size. The hip was then reduced. Copious irrigation was performed and any obvious bleeders were cauterized. At this point, a 5 Ethibond suture was then placed through the greater trochanteric region to repair the gluteus minimus, the anterior capsule and gluteus medius through bone tunnels. The tensor fascia lata and IT band was then repaired with #1-0 Vicryl suture, subcutaneously with 0 Vicryl and staples on the skin. A sterile dressing was placed and the patient was taken to the PACU in stable condition. Total Hip Replacement Posterior SURGEON: Edward T. Humbert, DO ASSISTANT: David Hodges, PA DATE OF PROCEDURE: ?? PREOPERATIVE DIAGNOSIS: Osteoarthritis of ?? hip. POSTOPERATIVE DIAGNOSIS: Osteoarthritis of ?? hip. PROCEDURE PERFORMED: Total hip replacement. APPROACH: Posterior COMPONENTS: ?? ESTIMATED BLOOD LOSS: ?? FLUIDS: ?? SPECIMENS: ?? We did discuss with this patient the benefits and complications of surgery, including infection, injuries to nerves, vessels and tendons, component loosening, component periprosthetic fractures, deep vein thrombosis, pulmonary embolisms, death, need for subsequent revision surgery, recurrent pain, recurrent limping, recurrent effusions and swelling, bleeding, as well as need for blood transfusions, leg length discrepancies and dislocations of components, were all discussed at length with this patient. After benefits and complications were discussed, the patient did opt for surgical intervention. PROCEDURE IN DETAIL: The patient was taken to the operative suite, placed in supine position and placed under appropriate anesthesia. The appropriate hip was prepped and draped in a sterile fashion in the lateral decubitus position. Using a posterior approach, a skin incision was made in the posterior third over the greater trochanteric region. A skin incision was made and sharp dissection was taken down to the gluteus maximus fascial layers which were split in line with their fibers. Anterior and posterior acetabular retractors were placed and the hip was internally rotated, exposing the gluteus medius, piriformis and short external rotators. A blunt retractor was then placed under the gluteus medius tendon and identification of the piriformis was then performed and Bovie cautery was used to cauterize through the piriformis, short external rotators and capsule. The capsule was then teed at the level of the piriformis and the femoral neck and femoral head were exposed. At this time, with internal rotation, the hip was dislocated protecting soft tissues underneath the femoral neck with Hohmann retractors. A femoral neck cut was made one fingerbreadth proximal to the lesser trochanter region. The femoral head was then removed. At this point, the anterior and posterior acetabular retractors were placed as was the blunt inferior retractor to expose the acetabulum. Anterior and posterior osteophytes were removed as well as the labrum was excised. Reaming was then performed after the appropriate size reamer in 45 degrees of abduction and 20 degrees of anteversion. At this time, an appropriate acetabular component in size was placed with an excellent peripheral rim fit in 45 degrees of abduction and 20 degrees of anteversion. Once this was performed, an appropriate liner was placed and checked with a Cobb elevator. Once this rim fit was performed, the hip was then internally rotated exposing the femoral neck with femoral head elevator and Hohmann retractors. Broaching was performed posterolaterally up to appropriate femoral component size. This was then trialled with appropriate femoral neck and head sizes with flexion to 90 degrees, abduction and internal rotation to 45 degrees. The hip was stable as well as maximum extension at 30 degrees and external rotation to 20 degrees anteriorly. Leg lengths were equal on the table in the lateral position. Permanent femoral component and femoral head was placed and the hip was reduced. Copious irrigation was then performed. At this point, the capsule and piriformis were repaired back to the gluteus medius with #1-0 Vicryl suture. Gluteus maximus fascial layers were then repaired with #1-0 Vicryl suture. 0 Vicryl was used for subcutaneous repair and staples on the skin. A sterile dressing was placed and the patient was taken to PACU in stable condition.