Chapter 4 Handout
advertisement

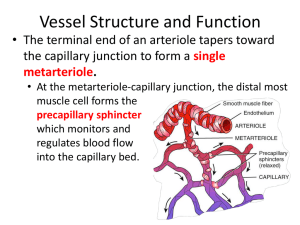
Chapter 4. Tissue Response to Injury: Inflammation, Swelling, and Edema Inflammation • The local response of the body to an __________________ • Purpose – – Cardinal Signs of Inflammation • Rubor: • Calor: • Edema: • Dolor: • Funca laesa: * Each of these signs will occur to some degree when tissue is injured and the body responds with the inflammatory process.* Common Misconceptions of Inflammation • Do you need to limit or eliminate inflammation? • Answer: – _________________ will not occur without inflammation. • You cannot ____________________ inflammation. • You can only _____________________ the signs of inflammation. • Swelling, edema, and inflammation are synonymous – WRONG! – _______________ and ________________ occur during inflammation. – _______________ and ________________ are not the same. – All edema causes swelling, but not all swelling is caused by edema. Phases of Inflammation • Inflammation consists of ____ sequential and overlapping events. Ultrastructural changes Chemical mediation Hemodynamic changes Leukocyte migration Primary Injury • Any occurrence that impairs tissue structure or function • Most sports injuries are caused by – Macrotrauma: – Microtrauma: • Other causes of injury include – Physical agents: – Metabolic processes: – Biological agents: – Chemical agents: – Endogenous chemicals: Normal secretions • In abnormal locations (gout) • In increased quantity in a normal location (stomach ulcers) Ultrastructural Changes • Cellular ________________ is disrupted and eventually breaks down. • Contents spill out into the ____________________ spaces, thereby killing the damaged cell. • Two causes – Direct: ____________ injury • – Indirect: ______________ injury • • Enzymes (chemicals) • Occur as a direct result of ____________________ and indirectly as a result of _______________________ Chemical Mediation • Histamine, bradykinin, and other chemicals • Modify and regulate the rest of the inflammatory response to: – – Hemodynamic Changes • Arteries dilate, increasing blood flow to the injured area. – Blood vessels that were previously ___________________ open – Therefore, blood flow through individual vessels ____________________ – And the rate of blood flow through individual vessels ____________________ • Slowing of blood flow is necessary, so ________________ can move to the margins • Leukocytes (WBCs) – Marginate – Tumble along the vessel wall – Adhere to the vessel wall near an opening – Pass though the vessel wall Metabolic Changes • ↓ __________________ • ↓ __________________ • Causes cell to switch to ___________________ metabolism • Membrane functions slow down. • Sodium pump maintains the concentration of intracellular sodium at a very low level. • Passive diffusion of Na++ into cell • ↑ ____________________ concentration in cell and organelles • ↑ _____________ in cell • Cells swell and burst • ↑ Intracellular acidosis (lactic acid) • Membrane attacked • Lysosome digests cell Permeability Changes • Histamine and bradykinin increase the ______________________ of small blood vessels. • The endothelial cells contract, pulling away from each other. • Gaps are left, through which the ________________ can move out of the vessel and to the injury site. Leukocyte Migration • _____________adhere to the endothelium (vessel wall) and/or to other white blood cells. • ______________________ and _______________________ move out of the vessel by squeezing through the endothelial gaps. • Neutrophils first, then larger macrophages Neutrophils – Travel fast and arrive at the injury site first – Provide the first line of defense – When they die, they release chemical mediators that attract macrophages. Macrophages – Live for months – Long-lasting second line of defense – Release potent enzymes that may _____________________ connective tissue, thus adding to the injury – Release chemical mediators that may _____________________ inflammation – Release factors that aid in healing – Secrete proteins that are important in defense mechanisms Phagocytosis • Digestion of cellular debris and other foreign material into pieces small enough to be removed from the injury site • ______________ and ____________________________ work together Chronic Inflammation • Recurring inflammation • _______________ inflammation occurring before the _______________ episode of _______________ inflammation has finished • Chronic inflammation • Results from ______________________ but does not necessarily involve an inflammatory reaction • Structural disruption and microvascular damage may occur (causing pain and other symptoms) before the classic inflammatory process is set into action. • Accumulation of _________________ in the tissues • Persists for several _____________, or ____________, and has vague and indefinite termination • Unable to eliminate the __________ of injury and restore normal ________________ • MOI = Orthopedic Injury Model (Figures 4.10 – 4.12) Contusion – Three cells – Nerve 1 – Blood vessel B • Immediate ultrastructural change – Local nerves and blood vessels may be disrupted or broken. – This damage is called primary traumatic damage. • Hemorrhage – Extravascular ___________________ occurs from broken blood vessels. – Few minutes only (usually) – Clot forms, stopping hemorrhage. – ____________ forms into strands, creating a network somewhat like a fishnet. – This net captures circulating platelets. – A plug forms to seal the damaged vessel. • • • • Hematoma forms • Comprised of ____________ and _________________________ • Places pressure on damaged and undamaged ____________ fibers • Pain, from damaged nerve – Muscle spasm and more pain – Body attempts to protect itself by ______________ the area, thus preventing aggravation of injury. • Inhibition of muscular strength, range of motion, etc. • Hematoma also triggers release of _____________________ mediators Chemical Mediation • The damaged cells release chemical mediators as a signal to the body that an injury has taken place. • Secondary enzymatic injury begins. • _______________ release enzymes that digest cellular _______________ • Additional cell ____________ occurs • ______________ occurs. • Chemical mediators released from dying cells cause – Hemodynamic changes – Permeability changes – Leukocyte (white cell) migration Hemodynamic changes – Blood flow _____________ OR ______________ – Secondary ______________ injury begins. The inflammatory response is not all positive. • Example – Slowed blood flow in the vessels on the periphery of an injury and decreased blood flow from the damaged vasculature result in less oxygen to the cells. • If prolonged, secondary __________________ injury occurs. • The total amount of damaged tissue is ______________________, and more debris is added to the hematoma. Swelling, Edema, and Vessel Fluid Pressures What Is Edema? • Accumulation of ___________________ in the tissue • What causes it? – Unbalanced fluid dynamics – Must understand normal fluid dynamics (review) Fluid Filtration in Normal Tissue Fluid in • • • Fluid out Occurs constantly between capillary and tissue Sum of multiple forces In capillary and tissue – Oncotic (osmotic) pulls – Hydrostatic pushes Hydrostatic Pressure • Pressure exerted by a column of water • The higher the column of water, the greater the pressure. • Example: swimming • The deeper you go, the higher the column of water above you and the greater the pressure. • The depth of the water, not the amount of water, is important. • Hydrostatic pressure is exerted by the water portion of the blood. • Hydrostatic pressure pushes water. – Capillary hydrostatic pressure pushes fluid out of the capillary. – Tissue hydrostatic pressure pushes fluid into the capillary. capillary CHP tissue THP Oncotic Pressure • Also called colloid osmotic pressure • Results from the attraction of fluid by free protein – Tissue oncotic pressure pulls fluid out of the capillary. – Capillary oncotic fluid pulls fluid into the capillary. capillary COP tissue TOP Fluid Filtration in Normal Tissues, Revisited •Sum of all forces What Causes Edema? • Imbalance of fluid filtration caused by an injury • Hematoma (tissue debris and hemorrhage) dumps large amounts of free protein into tissue spaces. • _________________ tissue oncotic pressure • Fluid accumulates in _________________ thereby increasing _____________________ and ______________________ What Is Swelling? • Hemorrhaging and edema – Can do nothing about hemorrhaging – Can _____________________ edema What Causes Swelling? Fluid in > Fluid out How Does Cold Decrease Swelling? • As cold decreases secondary hypoxic injury, the amount of free protein in tissues decreases. • This causes less tissue oncotic pressure (the major factor for edema). • Cold can prevent edema from occurring only if applied soon after injury. • Once edema develops, cold application cannot decrease that edema. Time Course of Swelling • Swelling immediately after injury is the result of direct hemorrhaging. • Edema begins minutes to hours after injury and continues to develop over many hours. – Accounts for the delayed nature of most swelling. Secondary Injury and Edema • Secondary injury results in increased _________________, and increased ________________ can contribute to increased secondary injury. • Two mechanisms – As ______________________ develops, the distance between blood vessel and tissue cells __________________. • More difficult for __________________ and other substances to diffuse from the circulatory system to the tissue – Edema can compress the blood vessel, thus decreasing circulation to the area. Common Misconceptions Concerning Ice and Inflammation • Many think the purpose of ice is to decrease inflammation. • However, inflammation is necessary to prepare for healing. • Healing cannot take place until much of the cellular debris is removed from the area. – So decreasing inflammation is not helpful. • • Misconception results from confusing inflammation with swelling. • The more the swelling is contained, the quicker the injury can heal. Another misconception concerning ice is that it should be used until the swelling is gone. • Ice is effective for preventing swelling but not for removing swelling. • Swelling reduction occurs as free protein is removed from the area. Summary • Inflammation is the body’s response to any injury. – Protects the body against invasion by foreign bodies and prepares the injured tissue for repair. • After understanding inflammation, hemorrhaging, and edema, you will be qualified to educate your athletes and coaching staff, who commonly apply ice to decrease inflammation after an injury. – You can explain that swelling is one of the signs of inflammation but is not the process itself; they are separate but related processes.