BIO 307
PATHOPHYSIOLOGY
DR. GREENAMYER
BASIC TERMS
• Vocabulary
–
–
–
–
–
Hyper-- vs hypo---itis
--osis
--opathy
Idopathic, Iatrogenic, Nosocomial
• Disease (Syndrome) vs Normalcy
• Etiology: causes or reasons for a disease
– Virus/bacteria, occupation, age, sex, nutritional status,
genetics
• Can be used to classify disease
– Inherited, congenital, toxic, infectious, traumatic,
degenerative, neoplastic, metabolic
• Pathogenesis: development/evolution of
disease
• Manifestations of Disease
– Signs: objectively identifiable changes (fever,
BP, HR, PCV)
– Symptoms: subjective feelings (nausea, pain)
FACTORS THAT INFLUENCE DISEASE
• Extrinsic factors—outside individual, may or may
not be controlled
– Diet, medication, exposure to harmful agents
• Intrinsic factors—rarely under individual control
– Age, sex, genetic inheritance
– Congenital vs inherited
• Most diseases are a combination (interaction) of
factors
Genetic disorders
• Single gene disorders—may affect any
tissue/organ system
• Autosomal dominant—need only one bad copy of
gene
– Equally prevalent in males and females
– No skipping of generations, delayed onset common
– Typically less severe than recessive, structural protein
defect
– Huntingdon’s Disease, Adult polycystic kidney disease
• Autosomal recessive—need two bad
copies of gene
• Equally prevalent in males and females
• May skip many generations, but often seen in
siblings
• Early age onset, more often enzymatic deficiency
• Cystic fibrosis, sickle cell anemia
• Sex Linked disorders—carried on X (most
often) or Y (rarely) chromosome
• X linked recessive most common
• More common in male; females are usually
asymptomatic carriers unless unequal X inactivation
or 2 copies of the mutated gene
• All daughters of affected men are carriers
• Hemophilia A, Duchenne’s muscular dystrophy
• Mitochondrial gene disorders—passed
through maternal line
– Extremely rare
Chromosomal abnormalities
• Aneuploidy—abnormal number of chromosomes
• Down’s syndrome (trisomy 21) most common
• Result of nondisjunction
• Translocations—result in structural abnormalities
– Genetic material exchanged between nonhomologus
chromosomes
– Robertsonian translocations most important clinically
– Philadelphia chromosome in chronic myelogenous
leukemia
Fig. 4-18
Causes of Cellular Injury
• Hypoxic injury (ischemia is #1 cause)
• Chemical injury (free radicals, heavy metals)
• Physical injury (mechanical, thermal, radiation,
electric shock)
• Infectious injury (bacteria, viruses, fungi,
parasites)
• Immunological and inflammatory injury
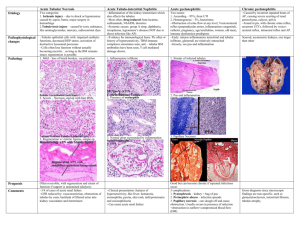
Terminology of Cellular Changes
• Atrophy
– Autophagy in malnutrition
•
•
•
•
Hypertrophy vs hyperplasia
Dysplasia (atypical hyperplasia)
Metaplasia
Senescence (aging) and death
Common themes/results (T 2-2)
•
•
•
•
ATP depletion
Defects in membrane permeability
Increased intracellular calcium
Increased free radicals
Manifestations of Cellular Injury
• Accumulate water (cloudy swelling,
oncosis, hydropic degeneration)
• Accumulate lipids (steatosis),
carbohydrates, or proteins
• Atrophy—requires autophagy
– accumulation of pigments (brown atrophy)
Cloudy swelling (oncosis, hydropic
degeneration)
Cell death (necrosis)
• Nuclear changes are most obvious
– Pyknosis—shrunken, irregular, dark staining
nucleus
– Karyorrhexis—fragmentation of nucleus
• Karyolysis—dissolution of nucleus
• Coagulative necrosis—most common type
– Cells retain shape, tissue retains normal
architecture
– Indicates ischemia—dry gangrene
• Liquifactive necrosis—most common in brain
– Can result from hydrolases from bacteria
– Wet gangrene
• Caseous necrosis—cells degenerate but fragments
remain--Mycobacterium infections
Apoptosis
• Active process of programmed cell death
(scattered, single)
– Deletes excess cells during development
– Probably occurs in malignant cells or cells
damaged by chemotherapy
• NOT accompanied by inflammation
– Should not stimulate an immune reaction
Apoptosis
Systemic Manifestations of
Necrosis (Inflammation)
•
•
•
•
Fever (from pyrogens)
Increased heart rate
Increased WBCs
Elevated presence of tissue specific enzymes
• CPK creatine phosphokinase
• LDH lactic dehydrogenase
• ALT alanine aminotransferase
• Loss of some organ function
• Pain
LOCAL INFLAMMATION
Purpose of Inflammation
•
•
•
•
Destroy and remove insult
Wall off and confine damage
Stimulate immune response
Promote healing
Causes of inflammation
• Infection
• Trauma—physical, chemical, thermal,
radiation
• Immune hyper-sensitivity reactions
INFLAMMATION---types
• Acute
– Redness, heat, pain, swelling (rubor, calor,
dolor, tumor)
– Altered function (functio laesa) has been added
• Subacute
• Chronic---Longer duration
– Granuloma formation—massive numbers of
macrophages
Fig 6-3
Clotting
Cytokines in acute inflammation
Local Inflammatory Response
• Margination and diapedesis of WBC
• Vascular Response—increased permeability
• Arterial dilation—increased local BP
• Endothelial cells of blood vessels (venules)
separate
• Exudation—significant amounts of protein lost into
interstitial space
• Water follows protein to maintain osmotic balance
Results of water movement
• Interstitial swelling pulls flaps of lymphatic
capillaries apart
• Increased flow of lymph
• Protein, cells enter lymphatics
• Lymphangitis/lymphadenitis (lymphadenopathy)
may result
Mediators of inflammation
• Histamine—mast cells
• Activated Factor XII--Clotting System
• Arachidonic acid metabolites
• COX and LOX pathways
• Complement cascade
• Miscellaneous cell factors
Fatty acids
Chronic inflammation
Exudates
• Serous—protein in interstitial fluid
• Fibrinous—fibrinogen accumulates on serous
surfaces
• Mucinous—mucous membranes—cellular
secretion
• Neutrophillic—purulent—bacterial
infection/necrotic cells
• pus is suppurative exudate of neutrophils and dead bacteria
Systemic Manifestations of
Inflammation
• Fever
• Leukocytosis
• Increased Erythrocyte Sedimentation Rate
Wound Healing
• Healing by first intention
• Healing by second intention (granulation)
Fig 6-21
Indications of wound infection
• Abscesses, furuncles (boils), carbuncles
• Cellulitis—widespread purulent
inflammation
• Mixed exudate from wound
– Fibrinopurulent
– Mucopurulent
– Serofibrinous
Factors that Delay Wound Healing
•
•
•
•
•
•
Oxygen deficiencies/ Ischemia
Nutrition deficiencies
Fluid/ electrolyte imbalances
Age
Medications or other disease
Extent of tissue damage
• Dehiscence/ evisceration may result from premature suture
removal
Complications of healing
• Scaring
– strictures, contractures
• Adhesions
• Keloids