The LIVER and HHT
advertisement

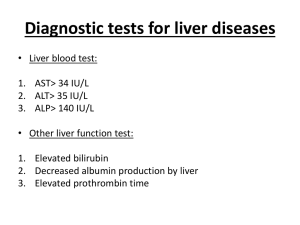
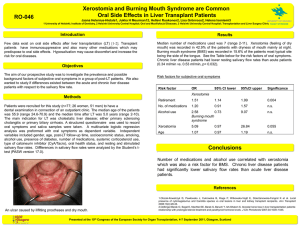
The LIVER and HHT The majority of people with HHT have vascular malformations in the liver. The malformations are usually small telangiectasia, similar to the telangiectasia that occur on the skin, and do not cause any problems. However, approximately 5% of people with HHT have liver vascular malformations that will cause symptoms, usually later in adult life. The symptoms of HHT liver involvement tend to fall into one of three groups. The three types of liver involvement are as follows: 1. Heart failure type. This is the most common of the three types of liver involvement and can cause fatigue, shortness of breath, and swelling of the legs. These symptoms occur because blood passes rapidly through the abnormal blood vessels in the liver and immediately back to the heart, instead of going through smaller blood vessels where the blood is normally slowed down. This can put an extra load on the heart, causing it to work harder than it normally would. After some time, this can lead to heart failure. People with this type of liver involvement also often have a “bruit” over the liver. A “bruit” is a sound over the liver that a physician can hear with a stethoscope. 2. Portal hypertension type. This type of liver involvement can cause fluid in the abdomen (ascites) and enlarged blood vessels in the esophagus, which can bleed. These symptoms occur because of elevated pressure in the veins of the liver. 3. Biliary type. This type of liver involvement can cause abdominal pain, abnormal liver tests and studies such as ultrasound or computed tomography (CT) scan show bile duct abnormalities or cysts in the liver. This type of liver involvement occurs because the blood supply to the ducts carrying bile from the liver (bile ducts) is reduced because of abnormal blood flow. In more severe cases, there may be jaundice (yellow coloration of the skin and eyes) and fever. There are many causes for heart failure, abdominal pain, and the other symptoms listed above so it is important to work with your physician and with an HHT treatment center when being evaluated for these problems. Screening for Liver Involvement Although there is no agreement regarding screening for liver involvement, there are currently very few HHT Centers screening all HHT patients for liver involvement. Screening is usually performed only if an individual has symptoms that could be due to liver HHT. Specialized abdominal ultrasound (including a technique called Doppler) or abdominal CT can show vascular malformations in the liver. These tests are best interpreted by physicians with experience in managing HHT and liver vascular malformations. Finally, abdominal angiography (inserting a small catheter into an artery in the groin, advancing it into the artery to the liver and injecting dye) can be performed with multiple x-ray pictures. Strain on the heart can be detected with echocardiography in severe cases. In other cases, cardiac output can be measured at the time of angiography or during cardiac catheterization, to evaluate the strain on the heart. Again, we highly recommend that one of the HHT treatment centers be involved in any evaluation of your liver. Some tests, such as ERCP (endoscopic retrograde cholangio-pancreatography) and liver biopsies, can be dangerous in people with HHT liver involvement and must be avoided. Treatment Treatment for liver involvement is only recommended if the liver malformations are causing symptoms. If the liver malformations are not causing symptoms, the current recommendation is to do nothing. Management of patients with liver malformations is not currently standardized and treatment is decided on a case by case basis and should be managed by a treatment center familiar with HHT. Treatment depends on the symptoms. For example, for high output heart failure, treatment usually involves medical therapy (medications, diet). It is very important to treat anemia in patients with liver VMs. More invasive treatments, such as embolization and liver transplantation have been reported. Treatment with embolization has been successful in a few patients, but has also caused sudden liver failure and death in others. We currently have no method to confidently distinguish which patients can be safely and successfully treated by liver embolization techniques. Embolization has led to severe complications when performed in the liver – even though it has been very successful in treating lung AVMs. For this reason, if you or someone in your family has liver VMs with significant symptoms, we urge immediate consultation with an HHT center before any decision is made regarding invasive diagnostic tests or treatment. A few reports reveal that successful liver transplantation can be done in patients in whom there are severe symptoms caused by the liver VMs. We need to gather more information as it becomes available. While liver transplantation has been done successfully in the North America and Europe, only small numbers of patients have undergone this procedure to date. REFERENCES: Garcia-Tsao G, Korzenik JR, Young L, Henderson KJ, Jain D, Byrd B, Pollak J, White RI Jr., Liver Disease in Patients with hereditary hemorrhagic telangiectasia. New England J Med. 2000. Vol 343(13): 931-935. Odorico JS, Hakim MN, Becker YT, Van der Werf W, Musat A, Knechtle SJ, D'Alessandro M and Kalayoglu M Liver Transplantation as Definitive Therapy for Complications After Arterial Embolization for Hepatic Manifestations of Hereditary Hemorrhagic Telangiectasia" from Liver Transplantation and Surgery, Vol. 4, No. 6, (November) 1198, pp 483-490 Hisamatsu K, Ueeda M, Audo M, Koike K, Matsuo N, Marsu-ura K, Ueda H, Hirohata M, Imai M Peripheral arterial coil embolization for hgepatic arteriovenous malformations in Osler-WeberRendu disease; useful for controlling high output heart failure, but harmful to the liver:. >From Intern Med 1999 Dec; 38 (12); 962-8. Boillot O, Bianco F, Viale JP, Mion F, Gille D, Delaye J, Pallard P, Plauchu H. Liver Transplantation resolves the hyperdymanic circulation in hereditary Hemorrhagic Telangiectasia with hepatic involvement. Gastroenterology 1999 Jan: 116 (1): 187-92 Miller FJ Jr, Whiting JH, Korzenik JR, White RI Jr. Causation with use of hepatic embolization in the treatment of hereditary hemorrhagic telangiectasia (letter) PMID: 10580979UI: 20056752 Comment on: Radiology 1998 Dec; 209 (3): 735-9 Welk C, Johannas W, Janssen J, Ggreiner L The Liver and Hereditary Hemorrhagic Telangiectasia Z GASTROENTEROL 2000 Jan: 38 (1): 31-37