BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS
advertisement

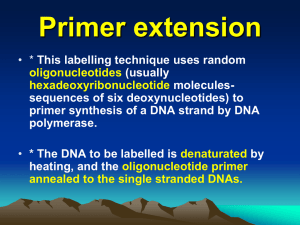
BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS Dr. Apr. Dieter Deforce 2 1. Introduction In order to define what “biotechnological techniques used in medical diagnosis” are lets first take a look at the definition of the word “biotechnology”: “The means or way of manipulating life forms (organisms) to provide desirable products for man's use.” A common misconception is that biotechnology refers only to recombinant DNA (rDNA) work. However, recombinant DNA is only one of the many techniques used to derive products from organisms, plants, and parts of both for the biotechnology industry. A list of areas covered by the term biotechnology would more properly include: recombinant DNA, plant tissue culture, rDNA or gene splicing, enzyme systems, plant breeding, mammalian cell culture, immunology, molecular biology, fermentation, and others. The biotechnological techniques used in medical diagnosis can be devided into two big categories: molecular genetic techniques (such as PCR, sequencing, …) and techniques based on immunology. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 2 3 2. Molecular techniques The development of molecular biological techniques in the diagnosis of viral infection has been very fast and has led to the discovery of new viruses, the rapid identification of drug resistance and the active monitoring of the efficacy of therapy. Some of the technologies described in what follows already have application in medical diagnosis which are approved by various regulatory organisms such as the FDA or other national offices. In addition to these validated tests some technologies are in the process of getting these validations and some technologies already have applications which are validated and some new applications of the same technology are now being investigated. Other technologies have no widespread or commercial use in medical diagnostics yet but the technology is in our opinion very promising and/or they are being used for research purposes in the field of medical diagnosis. Some general basic techniques which have applications in the different technologies described further are: Base-pairing hybridization assays. Base-pairing is the mechanism with which complementary DNA strands “hold” together. These strands can be dissociated from each other at temperatures above their Tm (melting temperature), and associated at temperatures below their Tm. The Tm is the temperature at which 50% of the strands are dissociated. In the standard hybridization assays the target DNA is immobilized on a solid support such as nitrocellulose or nylon to which single stranded DNA readily binds. Hybridization of labeled probe to the immobilized target DNA followed by washing and drying allows for the detection of specific DNA sequences. The reverse hybridization techniques which have become popular fix an unlabeled probe to the solid support, while the target DNA is labeled and allowed to hybridize. Hybrids DNA-DNA or DNA-RNA RNA-RNA Oligo-DNA or oligo-RNAd Tm (°C) 81.5 + 16.6(log10[Na+]a) + 0.41(%GCb) – 500/Lc 78 + 16.6(log10([Na+]a/1+0.7[Na+]a)) + 0.7(%GCb) - 500/Lc For <20 nucleotides: 2(In) For 20-35 nucleotides: 22 + 1.46(In) a Or for another monovalent cation, but only accurate in the 0.01-0.4 M range in M (0.05 M = standard) Only accurate for %GC in the 30% to 75% range c L=length of duplex in base pairs d Oligo, oligonucleotide; In, effective length of primer = 2 x (no. of G+C) + (no. of A+T) b Note that for each 1% formamide, the T m is reduced by about 0.6°C, while the presence of 6M urea reduces the Tm by about 30°C. Nucleic acid hybridization involves mixing single strands of two sources of nucleic acids, a probe which typically consists of a homogeneous population of identified molecules (e.g. cloned DNA or chemically synthesized oligonucleotides) and a target which typically consists of a complex, heterogeneous population of nucleic acid molecules. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 3 4 If either the probe or the target is initially double-stranded, the individual strands must be separated, generally by heating or by alkaline treatment. After mixing single strands of probe with single strands of target, strands with complementary base sequences can be allowed to reassociate. Complementary probe strands can reanneal to form homoduplexes, as can complementary target DNA strands. However, it is the annealing of a probe DNA strand and a complementary target DNA strand to form a labeled probe-target heteroduplex that defines the usefulness of a nucleic acid hybridization assay. Denaturation of double-stranded probe DNA is generally achieved by heating, a solution of the labeled DNA to a temperature which disrupts the hydrogen bonds that hold the two complementary DNA strands together. The energy required to separate two perfectly complementary DNA strands is dependent on a number of factors, notably: · strand length - long homoduplexes contain a large number of hydrogen bonds and require more energy to separate them; because the labeling procedure typically results in short DNA probes, this effect is negligible above an original length (i.e. prior to labeling) of 500 bp; · base composition - because GC base pairs have one more hydrogen bond than AT base pairs, strands with a high % GC composition are more difficult to separate than those with a low % GC composition; · chemical environment - the presence of monovalent cations (e.g. Na+ ions) stabilizes the duplex, whereas chemical denaturants such as formamide and urea destabilize the duplex by chemically disrupting the hydrogen bonds. A useful measure of the stability of a nucleic acid duplex is the melting temperature (Tm). This is the temperature corresponding to the midpoint in the observed transition from double-stranded to single-stranded form. Conveniently, this transition can be followed by measuring the optical density of the DNA. The bases of the nucleic acids absorb 260 = ultraviolet (UV) light strongly. However, the adsorption by doublestranded DNA is considerably less than that of the free nucleotides. This difference, the so-called hypochromic effect, is due to interactions between the electron systems of adjacent bases, arising from the way in which adjacent bases are stacked in parallel in a double helix. If duplex DNA is gradually heated, therefore, there will be an increase in the light absorbed at 260 nm (the optical density260 or OD260) towards the value characteristic of the free bases. The temperature at which there is a midpoint in the optical density shift is then taken as the Tm. For mammalian genomes, with a base composition of about 40% GC, the DNA denatures with a Tm of about 87°C under approximately physiological conditions. Often, hybridization conditions are chosen so as to promote heteroduplex formation and the hybridization temperature is BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 4 5 often as much as 25°C below the Tm. However, after the hybridization and removal of excess probe, hybridization washes may be conducted under more stringent conditions so as to disrupt all duplexes other than those between very closely related sequences. Probe-target heteroduplexes are most stable thermodynamically when the region of duplex formation contains perfect base matching. Mismatches between the two strands of a heteroduplex reduce the Tm for normal DNA probes, each 1% of mismatching reduces the Tm by approximately 1°C. Although probe-target heteroduplexes are usually not as stable as reannealed probe homoduplexes, a considerable degree of mismatching can be tolerated if the overall region of base complementarity is long. Increasing the concentration of NaCl and reducing the temperature reduces the hybridization stringency, and enhances the stability of mismatched heteroduplexes. This means that comparatively diverged members of a multigene family or other repetitive DNA family can be identified by hybridization using a specific family member as a probe. Additionally, a gene sequence from one species can be used as a probe to identify homologs in other comparatively diverged species, provided the sequence is reasonably conserved during evolution.Conditions can also be chosen to maximize hybridization stringency (e.g. lowering the concentration of NaCl and increasing the temperature), so as to encourage dissociation (denaturation) of mismatched heteroduplexes. If the region of base complementarity is small, as with oligonucleotide probes (typically 15-20 nucleotides), hybridization conditions can be chosen such that a single mismatch renders a heteroduplex unstable. Non-isotopic labeling Two types of non-radioactive labeling are conducted: • Direct nonisotopic labeling, where a nucleotide which contains the label that will be detected is incorporated. Often such systems involve incorporation of modified nucleotides containing a fluorophore, a chemical group which can fluoresce when exposed to light of a certain wavelength. • Indirect nonisotopic labeling, usually featuring the chemical coupling of a modified reporter molecule to a nucleotide precursor. After incorporation into DNA, the reporter groups can be specifically bound by an affinity molecule, a protein or other ligand which has a very high affinity for the reporter group. Conjugated to the latter is a marker molecule or group which can be detected in a suitable assay. The reporter molecules on modified nucleotides need to protrude sufficiently far from the nucleic acid backbone to facilitate their detection by the affinity molecule and so a long carbon atom spacer is required to separate the nucleotide from the reporter group. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 5 6 Two indirect nonisotopic labeling systems are widely used: • The biotin-streptavidin system utilizes the extremely high affinity of two ligands: biotin (a naturally occurring vitamin) which acts as the reporter, and the bacterial protein streptavidin, which is the affinity molecule. Biotin and streptavidin bind together extemely tightly with an affinity constant of 1014 one of the strongest known in biology. Biotinylated probes can be made easily by including a suitable biotinylated nucleotide in the labeling reaction. • Digoxigenin is a plant steroid (obtained from Digitalis plants) to which a specific antibody has been raised. The digoxigenin-specific antibody permits detection of nucleic acid molecules which have incorporated nucleotides containing the digoxigenin reporter group. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 6 7 A variety of different marker groups or molecules can be conjugated to affinity molecules such as streptavidin or the digoxigenin-specific antibody. They include various fluorophores, or enzymes such as alkaline phosphatase and peroxidase which can permit detection via colorimetric assays or chemical luminescence assays, etc. 2.A. Polymerase Chain Reaction The polymerase chain reaction (PCR) has become one of the most widely used techniques in molecular biology. Since the technique is so well known, the basics of the technique will not be repeated here. It forms the basis for a lot of diagnostics based on molecular techniques, and a lot of variants have already been developed. We will discuss some of these variants which have applications in medical diagnostics. We will also discuss some precautions which should be kept in mind. The last chapters will discuss some of the specially adopted detection techniques for PCR products which have applications in medical diagnosis. An important advantage of PCR in the field of medical diagnosis is that PCR techniques only require very small amounts of sample. This makes the technique very useful for prenatal diagnosis, since it requires only such small amounts of sample chorionic villus samples at about 12 weeks of gestation can be used. PCR also has its place in bacteriology (see chapter 14, in The science of Laboratory Diagnosis, John Crocker and David Burnett, ISIS Medical Media, 1999). 2.B.1. Reverse transcriptase PCR (RT-PCR): this technique is used to amplify RNA from samples. The template for RT-PCR can be either total RNA or poly(A)+ selected RNA. RT reactions can be primed with random primers, oligo(dT), or a gene-specific primer. The most commonly used technique BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 7 8 (which is thechnique used for most applications which will be described in this course) uses a oligo-dT primer to prime the reverse transcription process and uses a two step process (see Figure). 5’ mRNA Oligo(dT) primer 3’ AAAAAAAAAAA(A) A + 3’ 5’ Anneal 3’ 5’ AAAAAAAAAAA(A) A 3’ 5’ Add reverse transcriptase 3’ 5’ AAAAAAAAAAA(A) A 3’ 5’ RNase H treatment 3’ 5’ single stranded cDNA ready for PCR A good overview of the different RT-PCR techniques and things to consider for optimalisation is given in the manual to be found at: http://www.lifetech.com/Content/TechOnline/molecular_biology/manuals_pps/pcrtechguide.pdf The RT-PCR technique is very useful for the detection of viral RNA in biological samples (eg. Hepatitis C). In the field of virology, the speed of detection and identification is extremely important and RT-PCR techniques offer the advantage over more traditional techniques such as ELISA and viral culture. As an example a protocol for the detection with RT-PCR of foot-and-mouth disease is available at http://www.iah.bbsrc.ac.uk/virus/Picornaviridae/Aphthovirus/fmd.htm 2.B.2. Inverse PCR: this is a general method for amplifying DNA flanking a previously characterized region. It uses primers derived from the extremities of the known region but instead of pointing towards each other the 5’ 3’ direction of the primers point away from each other. This would normally not lead to a PCR product, here however the DNA is first cut with restriction enzymes such that the known DNA is present in a BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 8 9 small restriction fragment (see Firgure). The cut DNA is then circularized with a ligation enzyme at very low DNA concentrations (low DNA concentration favors circularization versus ligation to another fragment).Using conventional PCR the flanking regions can now be amplified and characterized. This is important in the study of viral tumourigenesis, when attempting to identify possible insertion sites of viruses in host DNA and for the assessment of clonality in lymphoid tumours (Hall et al., Hum. Immunol. 1995, 43, 207-218). 2.B.3. Allele-specific PCR (ARMS test): in this technique primers are designed to discriminate between target DNA sequences which differ only a single nucleotide in the region of interest. This is a form of allele-specific PCR where the primers are designed to differ at the nucleotide(s) that occur at the 3’ terminus. This technique is based on the fact that in a PCR reaction it is crucial to have a correct base-pairing at the 3’ end (see Figure). This method is used to detect specific pathogenic mutations and is also called the amplification refractory mutation system (ARMS) and some commercial kits are available for disease diagnosis (such as cystic fybrosis), some can be found on: http://www.diagnostics.astrazeneca.com/elkits.htm BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 9 10 2.B.4. Real-time PCR (Quantitative PCR): Several variants already exist of this technology, but the core idea is the same for all of them. The idea is to detect how much PCR products are present after each PCR cycle. This allows for reliable quantitation of PCR products. End-point detections for the determination of PCR products (where first a normal PCR reaction is performed and the detection is done at the end) and estimation of the amount of starting material are not reliable since the exponential accumulation of PCR products reaches a plateau when a certain amount of PCR product has been generated. Specificity of the detection of the PCR products can be based solely on the selection of primers (using SYBR Green I double stranded DNA binding dye, see Figure) or additional selectivity can be added by using probes. The latter technique also commonly known as TaqMan PCR. This TaqMan PCR uses the 5’-3’ nuclease activity of Taq DNA polymerase to detect target sequences during amplification by PCR (see Figure). In addition to the conventional primers a probe, (usually 20-30 mer in length) is included in the PCR mix, designed to hybridize within the target sequence and to be non-extendible at the 3’ end. The fluorescent emission activity of a fluorescent repoter BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 10 11 molecule attached at the 5’ end is neutralized by a quencher molecule at the 3’ end. When hybridized to its target sequence, the intact probe shows no signal due to the proximity of the reporter molecule to the quencher molecule. During amplification Taq DNA polymerase, through its 5’-3’ nucleolytic activity, cleaves the probe into fragments, separating the reporter from the quencher and allowing for its detection. The level of fluorescence is directly proportional to the amount of specific amplification of the target. Real-time PCR as described here is thus the technique of choice to study the expression level of certain selected genes. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 11 12 Using a slight modification this technique can also be used to detect mutations or determine polymorphisms. In this setup two differently labeled probes are used. Since the machine can detect multiple colors we are able to determine which products get formed and thus which sequences are present (see Figure). The ARMS assay can also be modified to be performed using these real-time PCR technologies. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 12 13 2.B.5. Special precautions to be taken in performing PCR for diagnostic purposes: Contamination is one of the major reasons for misinterpretation of results with PCR and occurs when exogenous DNA or RNA, proteases, nucleases and various inhibitors of Taq polymerase are introduced into the reaction mix and lead to false positive or negative results. All tubes, tips and containers must be sterile and disposable. Since PCR is so extremely sensitive and powerful, extreme care should be taken not to contaminate the sample with exogenous DNA or previously amplified PCR products. For this reason one should always use positive displacement or barrier pipettes and there should be separate sets and working areas for samples pre- and post PCR. There should be a one way traffic of materials and samples from the pre- to the post-PCR working area. And one should always use positive and negative controls. 2.B.6. PCR-product carry over prevention (AmpErase): this technology is a simple yet powerful way to prevent that PCR products would be reamplified in subsequent PCR amplifications, thereby preventing false positive results. This method involves substituting dUTP for dTTP in the PCR mixture, and pretreating all subsequent PCR mixtures with the enzyme Uracil N-glycosylase (UNG) also calles AmpErase, prior to PCR amplification (see Figure). Products of the PCR reation will contain deoxyuridine, and are thus biochemically different from native DNA molecules which contain thymidine instead of deoxyuridine. UNG catalyses the cleavage of deoxyuridine containing DNA at deoxyuridine residues by opening the deoxyribose chain at the C1-position. UNG will not degrade native DNA (containing thymidine) or RNA because the uridine in RNA is a ribose sugar and the UNG enzyme only cleaves deoxyribose sugars. When heated in the first thermal cycling step at the alkaline pH of the PCR reaction, the contaminating carry-over PCR product breaks at the positions of the deoxyuridine. Newly synthesized BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 13 14 PCR products in the PCR reaction will not be degraded because the temperature is maintained above 55°C, and the UNG enzyme is not active at these high temperatures. After amplification the UNG is chemically denatured. 2.B.7. The Line Probe Assay (LiPA): This is a technique for the sequence specific detection of PCR products. This technique was developed by Innogenetics. The LiPA tests are based on the reverse hybridization principle (see Figure, see also chapter 2E on allele specific oligonucleotide probes). One of the primers used during the PCR reaction is biotinylated at the 5’ end. Amplified biotinylated PCR-products are then chemically denatured and the single stranded amplified target DNA is hybridized with specific oligonucleotide probes which are immobilized as parallel lines on a nitrocellulose strip. This strip contains several probes with varying sequences for known mutations or polymorphisms of genes, thus allowing for mutation analysis or genotyping of the sample. After hybridization, streptavidin labeled with alkaline phosphatase is added and binds to the biotinylated bound PCR product. This phosphatase converts the added chromogen (NBT/BCIP) to a purple precipitate allowing for detection of the bound DNA. Subsequently the places of hybridization can be read on the strip. The advantage of this technology is that only one PCR amplification and one hybrydization step are needed to obtain multiple answers. Kits have been developed to perform HLA-typing (Human Leukocyte Antigens) and for the detection of infectious diseases and prediction of their drug resistance based on the detection of mutation in the genomic material of these infectious diseases. A very important feature of this technique is that the strip can contain many different sequences so that in one assay a lot of mutations or polymorphisms can be screened/determined. More information can be found on: BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 14 15 http://www.innogenetics.be/Website/Website.nsf/Diagnostic+Products?Op enView&Start=1&Count=30&Expand=6#6 2.B.8. AMPLICOR technology: this is a technique for detecting specific PCR products. The technique also gives limited quantitation of the starting material. This technique was developed by Roche. As with the LiPA test, the AMPLICOR test is based on the reverse hybridization principle. The PCR reaction used is based on the AmpErase technique and one of the primers is biotinylated at the 5’ end. Immediately after amplification, the strands are chemically denatured by the addition of an alkaline solution. Denaturation occurs because the hydrogen bonds linking the two strands are weak and breakdown at high pH. The single strands are then hybridized onto oligonucleotide capture probes linked to BSA (Bovine serum albumin) which are bound to a plastic microwell plate. After hybridization, streptavidin conjugated with horseradish peroxidase is added and binds to the biotinylated bound PCR product. This peroxidase oxidizes the tetramethylbenzidine substrate in the presence of hydrogen peroxide to a blue colored complex, the reaction is stopped after which the blue turns yellow and the absorbance is measured using a photometer. This technique allows for the detection of a certain DNA sequence and gives an idea of the copy number of the target present in the sample. In contrast to the LiPA technology this technique is not used for detecting mutations or polymorphisms it is used for detecting the presence or absence of a certain BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 15 16 target and to give an idea of the amount of the copies present in the starting material. Kits have been developed to screen for infectious diseases such as HIV, HTLV, M. tuberculosis, CMV and others. More information can be found on: http://us.labsystems.roche.com/ldpage.htm 2.B. Sequencing Nowadays almost all sequencing is performed using cycle sequencing and using fluorescently labeled terminators. This technique which is based on the Sanger chain termination method will be discussed here in more detail. Cycle sequencing, also called linear amplification sequencing, uses like the standard PCR reaction thermostable DNA polymerase and a temperature cycling format of denaturation, annealing and elongation. The difference is that cycle sequencing employs only one primer and includes fluorescently labeled ddNTP chain terminators in the reaction. The ddNTP’s are added in the reaction in much lower amounts than the regular dNTP’s. Whenever the polymerase adds a fluorescently labeled ddNTP the reaction stops since further elongation is not possible. The four ddNTP’s used are all four labeled with a different fluorescent dye (see Figure). The use of only one primer means that unlike the exponential increase in product during PCR reactions, the product accumulates linearly. Given the much lower amplification power of cycle sequencing it is evident that much more starting material is required than for a PCR reaction. To overcome this problem one can first perform a PCR amplification of the sequence of interest. After amplification the primers of the PCR reaction first have to be removed and the purified PCR product is then used as the template in the cycle sequencing process. If the sequence which is being cycle sequenced is not polymorphic, this cycle sequencing results in the accumulation of single stranded products which differ 1 base in length and all products of the same length end with the same fluorescently labeled ddNTP. When this reaction is then separated on a high resolution sieving matrix (comparable to polyacrylamide gels) and detection of the products is being performed with laser fluorescence the sequence can be read as seen in figure. This is also called automated DNA sequencing. Detection of these sequences can now be performed by electrophoresis over sieving matrix filled capillaries. A typical sequence length of 700 bases can be read on one capillary with an analysis time of 2 hours. Modern systems can contain upto 96 capillaries in one machine allowing for 96 DNA sequences of 700 bases to be read in 2 hours. More information on this technique can be found at: http://www.appliedbiosystems.com/ga/ BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 16 17 1200000 PCR cycle sequencing 1000000 800000 600000 400000 200000 0 0 5 10 15 20 The very nature of sequencing makes it the most alround technique to search and diagnose mutations or polymorphisms. Although very versatile and in some cases the only available technique it is very costly and previously described methods (if available) might be easier and cheaper to use. Some kits for HLA-typing and for mutation screening in HIV are being sold commercially http://www.appliedbiosystems.com/molecularbiology/md/ BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 17 18 2.C. DNA microarrays The DNA microarray technology is a very recent technique in molecular biology, other terms used to describe this technology are: biochip, DNA chip, gene array, GeneChip (Affymetrix) and genome chip. Although this technology is mainly used for exploratory research purposes and gene-discovery, already it has identified some diagnostic uses (which will be discussed later on). A major limitation of the technique is the large amount of RNA required for one array (50-200 µg total RNA or 2-5 µg mRNA). This translates to 107108 cells or 1 to 10 mg of tissue, however as the technique advances the amount of material required will continue to go down. Base-pairing or hybridization is the underlying principle of DNA microarray technology. More specifically a reverse nucleic acid hybridization (see also chapter 2E on allele specific oligonucleotide probes) approach is employed: the probes are unlabeled DNA fixed to a solid support (the arrays of DNA or oligonucleotides) and the target is labeled and in solution. The DNA microarray is an orderly arrangement of probes (with known identity, being unlabeled DNA) on a glass or nylon support to which the target nucleic acids can bind based on complementary base-pairing. The probes are generally present in spots smaller than 200 microns each enabling the research on thousands of genes simultaneously. Two kinds of probes are used, which define two major variants in DNA microarray technology: 1) cDNA-probes: (500 to 5000 bases long) The cDNA probes are immobilized to a solid surface such as glass or membranes using a “spotting” robot. Here the DNA clones for the DNA probes have been prepared in advance and are then printed onto the surface of a microscope slide. A good review on how these cDNA probes are selected and immobilized is given in the nature genetics review to be found at: http://www.nature.com/cgitaf/DynaPage.taf?file=/ng/journal/v21/n1s/full/ng0199supp_10. html 2) oligonucleotide arrays: (20 to 25-mer oligos) These oligos can be synthesized in-situ (being on the chip) or they can be synthesized the conventional way followed by on-chip immobilization. This technology was developed at Affymetrix (www.affymetrix.com) and involves a combination of photolithography technology from the semiconductor industry with the chemistry of oligonucleotide synthesis, a good review of the production and use of the technology can be found at: http://www.nature.com/cgitaf/DynaPage.taf?file=/ng/journal/v21/n1s/full/ng0199supp_20. html DNA microarrays can be used to determine expression levels of genes, (in this case usually the gene transcription is compared between two or more different kinds BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 18 19 of cell-types (or between treated and non-treated cells)), or to identify sequence (gene mutation). 1) Expression profiling: In this application RNA is isolated from the cells to be analyzed. Using an oligo-dT primer, the mRNA is reverse transcribed into fluorescently labeled cDNA using the fluorescent labels Cye3-dUTP and Cye5-dUTP. A problem with this cDNA reverse transcription is the reverse transcription bias, this is not a problem when comparing the same mRNA across two cell populations (unless it causes the mRNA not to be transcribed at all), but it prohibits quantitative comparisons between different mRNA’s on one array. Since expression profiling is generally done according to the scheme depicted in FIGURE ARRAY1, a first cDNA pool (a reference, or non-stimulated cell pool) is fluorescently labeled with Cye3 and the cDNA pool of the test sample is labeled with Cye5. The two pools of cDNA are then diluted to have the same overall fluorescent intensity and after mixing they are hybridized to the DNA microarray. If a target contains a sequence complementary to the DNA probe, it will hybridize and be detectable by fluorescence. After hybridization and washing the array is scanned by exciting the fluorescent markers with laser light at their excitation wavelength, and the light emitted at the specific wavelength of each dye is detected with a chargecoupled device (CCD). Then computer comparisons give the ratio of expression between both tested cell types. A typical result can be seen in: http://llmpp.nih.gov/lymphoma/figures.shtml BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 19 20 2) Sequence information: Or screening of DNA variation, has to be performed by oligonucleotide arrays. This technique offers a huge potential for assaying for mutations in known disease genes, as recently shown in the case of the breast cancer susceptibility gene, BRCA1. In addition, this technique can be used to identify human single nucleotide polymorphism (SNP) markers. (see below for both applications). A good review on this application can be found at: http://www.nature.com/cgitaf/DynaPage.taf?file=/ng/journal/v21/n1s/full/ng0199supp_20. html Applications to diagnostics: I. SNP http://www.affymetrix.com/products/gc_HUSNP1.html II. Classifying cancers and predicting outcome (see abstract) Int J Cancer 2001 Feb 15;91(4):474-80 CDNA microarray gene expression analysis of B-cell chronic lymphocytic leukemia proposes potential new prognostic markers involved in lymphocyte trafficking. Stratowa C, Loffler G, Lichter P, Stilgenbauer S, Haberl P, Schweifer N, Dohner H, Wilgenbus KK Boehringer Ingelheim Austria, Vienna, Austria. Human cancer is characterized by complex molecular perturbations leading to variable clinical behavior, often even in single-disease entities. We performed a feasibility study systematically comparing large-scale gene expression profiles with clinical features in human Bcell chronic lymphocytic leukemia (B-CLL). cDNA microarrays were employed to determine the expression levels of 1,024 selected genes in 54 peripheral blood lymphocyte samples obtained from patients with B-CLL. Statistical analyses were applied to correlate the expression profiles with a number of clinical parameters including patient survival and disease staging. We were able to identify genes whose expression levels significantly correlated with patient survival and/or with clinical staging. Most of these genes code either for cell adhesion molecules (L-selectin, integrin-beta2) or for factors inducing cell adhesion molecules (IL-1beta, IL-8, EGR1), suggesting that prognosis of this disease may be related to a defect in lymphocyte trafficking. This report demonstrates the feasibility of a systematic integration of largescale gene expression profiles with clinical data as a general approach for dissecting human diseases. A good overview, with a lot of helpful links can be found at the webpage: www.gene-chips.com. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 20 21 It seems likely that eventually oligonucleotide arrays of one sort or another will replace most other methods for routine mutation screening in the more common diseases, and that automated DNA sequencing will be increasingly used for the rarer diseases. 2.D. Allele specific oligonucleotide hybridization The allele-specific oligonucleotide (ASO) hybridization is also referred to as dot-blotting. The general procedure of dot-blotting involves taking an aqueous solution of target DNA, for example total human genomic DNA, and simply spotting it on to a nitrocellulose or nylon membrane then allowing it to dry. The variant technique of slot-blotting involves pipetting the DNA through an individual slot in a suitable template. The target DNA can also be purified PCR products. In both methods the target DNA sequences are denatured, either by previously exposing to heat, or by exposure of the filter containing them to alkali. The denatured target DNA sequences now immobilized on the membrane are exposed to a solution containing single stranded labeled probe sequences. After allowing sufficient time for probetarget heteroduplex formation, the probe solution is decanted, and the membrane is washed to remove excess probe that may have become nonspecifically bound to the filter. lt is then dried and exposed to an autoradiography film. A useful application of dot-blotting involves distinguishing between alleles that differ by even a single nucleotide substitution, mutation detection. This technique has applications in mutation identification of diseases (eg. Mutations in the Von Willebrand factor). To do this allele-specific oligonucleotide (ASO) probes are constructed from sequences spanning the variant nucleotide site. ASO probes are typically 15-20 nucleotides long and are normally employed under hybridization conditions at which the DNA duplex between probe and target is stable only if there is perfect base complementarity between them: a single mismatch between probe and target sequence is sufficient to render the short heteroduplex unstable (see Figure). Typically, this involves designing the oligonucleotides so that the single nucleotide difference between alleles occurs in a central segment of the oligonueleotide sequence, thereby maximizing the thermodynamic instability of a mismatched duplex. Such discrimination can be employed for a variety of research and diagnostic purposes. Although ASOs can be used in conventional Southern blot hybridization (see below), it is more convenient to use them in dot-blot assays (see Figure). Another method of ASO dot blotting uses a reverse dot-blotting approach. This means that the oligonucleotide probes are not labeled and are fixed on a filter or membrane whereas the target DNA is labeled and provided in solution (examples using this technique are the LiPA and AMPLICOR technology). Positive binding of labeled target DNA to a specific oligonucleotide on the membrane is taken to mean that the target has that specific sequence. This approach, and related DNA microarray methods (already discussed), have many diagnostic applications. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 21 22 2.E. Oligonucleotide ligation assay The oligonucleotide ligation assay (OLA) tests for base substitution mutations. The test is based on the principle that two oligonucleotides BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 22 23 constructed to hybridize to adjacent sequences in the target, with the join sited at the position of the mutation will only be covalently joined by DNA ligase if they are perfectly hybridized. Various formats of the technique exist but the most recent and advanced technique uses modified tails on one probe and fluorescent tags (FAM, HEX or TET) on the other probe with the ligation products being electrophoresed and analysed on an automated sequencer. These modifications have allowed the number of known point mutation sites which can be screened at any one time to be increased and Applied Biosystems now have kits capable of screening for 31 known CF mutations in a single reaction tube and single lane of an electrophoresis run. In this test a cocktail of fifteen pairs of primers is used to amplify regions of the CFTR gene where common mutations are located. Each amplified segment (or amplicon) is probed with three oligonucleotide probes. The common probe hybridises to the amplicon at a sequence that is present in both normal and mutant alleles and is labeled with one of three fluorescent tags. The mutant and normal probes are allelic and can be distinguished by their length since they have varying numbers of mobility modifying tails attached. These tails are composed of Pentaethylene oxide (PEO) units (Figure). At any one locus, if the mutation is not present only the normal and common probe will form a ligation product, if a homozygous mutation is present only the mutant and common probes will ligate and in heterozygous samples both normal and mutant probes will ligate to the common probe in equal amounts but giving products of different mobility. The rTth DNA ligase facilitates ligation by catalysing the formation of a phosphodiester bond between the 5' phosphate of the common probe and the 3' hydroxyl of either the normal or mutant probe. This reaction will ONLY occur when both probes are hybridised and perfectly matched to the complementary target amplicon. Following ligation, the product for each amplicon has a unique combination of electrophoretic mobility and fluorescence which allows identification of the sample phenotype by size separation of the ligation product in each of the three colours (the CF kit is designed to have 10-12 blue, 10-12 green and 9-11 yellow peaks). A red labelled internal size standard allows Genescan analysis software to size products precisely, label fragment data and display fragments as labelled peaks in plot displays (Figure). This technique is suitable to mutation detection in any gene where a number of known mutations or common polymorphisms occur. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 23 24 BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 24 25 2.F. In Situ amplification BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 25 26 Also called in situ PCR represents for most histopathologists the marriage of standard histopathology and molecular biology. In situ PCR is able to amplify a single copy target nucleic acid sequence so that it can be detected in fixed tissues and cells and aims to correlate PCR results with morphology. Although in situ hybridization (ISH) has traditionally been used to localize nucleic acid sequences within the cell, this method cannot detect low copy numbers of target sequences (1-20 copies). This technique holds great potential for the field of diagnostic histopathology. Sample preparation is of great importance for these techniques. The objective of sample preparation is to provide within single cells a discrete reaction chamber to contain the PCR reaction. Cells, either in suspension or fixed to some form of solid phase support, are rendered sufficiently permeable so that oligonucleotide primers and other reaction components may diffuse into the cell. The permeation is controlled so that the products of amplification are retained within the cells upon thermal amplification and tissue morphology is retained so that meaningful histopathological interpretations can be made. Typical pretreatments are to fix cells or tissue in formalin or paraformaldehyde and affix the cells or tissue to glass slides using (for example) Denhardt's solution (dewaxing and rehydration is, necessary for paraffin waxembedded tissues). Tissues or cells are then digested with a carefully optimized low concentration of proteinase-K over 60 minutes to prepare for in situ PCR. A number of alternatives have been described including detergent, chemical denaturant, or microwave pre-treatments (see Figure). The PCR reagents are then added directly onto the cells or tissue and the reaction is sealed of with a cover slide which is sealed to the microscope slide to avoid evaporation of the reaction during the thermal cycling process. The PCR reaction itself is analogous to a traditional PCR reaction and involves the same reagents. After amplification the PCR products are detected by different techniques. A more detailed description of the technique and its many possible variations (analogous to the variations described in the previous chapter on PCR) can be found in chapter 52 “In Situ Amplification” of the book “The Science of Laboratory Diagnosis” by Crocker and Burnett (ISIS Medical Media, 1999). When applied to cancer studies in situ PCR can allow researchers to observe the expression of genes and the presence of mutations in the abnormal cells of tissue sections. The technique an also be used to locate cells with gene rearrangements and chromosomal translocations, to pinpoint unique gene alterations associated with neoplastic disorders, to detect latent viral infections and many more. In contrast to the situation in acute virus infection, in latent or persistent infection virus-infected cells comprise only a small fraction of the total number of cells in the tissue or tissue fluids under examination. Thus conventional in situ hybridization methods may not reveal infection. The techniques provide important tools for the study of viral pathogenesis. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 26 27 2.G. Southern blotting In this procedure, the target DNA is digested with one or more restriction endonucleases, size-fractionated by agarose gel electrophoresis, denatured and transferred to a nitrocellulose or nylon membrane for hybridization (Figure). Fragments are fractionated by size in a conventional agarose gel electrophoresis system. Following electrophoresis, the test DNA fragments are denatured in strong alkali. As agarose gels are fragile, and the DNA in them can diffuse within the gel, it is usual to transfer the denatured DNA fragments by blotting on to a durable nitrocellulose or nylon membrane, to which single-stranded DNA binds readily. The individual DNA fragments become immobilized on the membrane at positions which are a faithful record of the size separation achieved by agarose gel electrophoresis. Subsequently, the immobilized single-stranded target DNA sequences are allowed to associate with labeled single-stranded probe DNA. The probe will bind only to related DNA sequences in the target DNA, and their position on the membrane can be related back to the original gel in order to estimate their size. More detailed information on the technique http://www.protocol-online.net/molbio/DNA/southern.htm BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS can be found on: 27 28 2.G.1. Restriction fragment length polymorphisms: this technique uses the Southern blotting technique. Because the genomic DNA samples are fractionated by separation of restriction fragments according to size, mutations which alter a restriction site, and significantly large insertions or deletions occurring between neighboring restriction sites, can be typed. Such mutations will result in altered restriction fragment lengths, that is restriction fragment length polymorphisms (RFLPs). Direct detection of pathogenic point mutations by restriction mapping is an application of RFLP technology to diagnostics. Very occasionally, a pathogenic mutation directly abolishes or creates a restriction site, enabling direct screening for the pathogenic mutation. For example, the sickle cell mutation is a single nucleotide substitution (A T) at codon 6 in the -globin gene, which causes a missense mutation (Glu Val), and at the same time abolishes an MstII restriction site which spans codons 5 to 7. The nearest flanking restriction sites for MstII, located 1.2 kb upstream in the 5'-flanking region and 0.2 kb downstream at the 3' end of the first intron, are well conserved. Consequently, a -globin DNA probe can differentiate the normal A -globin and the mutant S-globin alleles in MstIIdigested human DNA: the former exhibits 1.2 kb and 0.2 kb MstII fragments, whereas the sickle cell allele exhibits a 1.4 kb MstII fragment (Figure). RFLP is also a powerful tool for the study of viral pathogenesis and for the genotypic classification of viruses. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 28 29 2.G.2. Restriction mapping: this technique, which also uses the Southern blotting technique is used to detect gene deletions. Certain diseases are associated with a high frequency of deletion of all or part of a gene. If a partial restriction map has been established for the gene under investigation, deletions can be screened by Southern blot hybridization using an appropriate intragenic DNA probe. If the deletion is a small one, for example a few hundred base pairs, it is often apparent as a consistent reduction in size of normal restriction fragments in the gene. An individual who is homozygous for this mutation, or is a heterozygote with one normal allele and another with a small deletion, can easily be identified by detecting the aberrant size restriction fragments. Large deletions will lead to absence of specific restriction fragments. Homozygous deletion of large DNA segments can easily be detected as complete absence of appropriate restriction fragments associated with the gene. If, however, an individual is heterozygous for a relatively large gene deletion, the deletion may still be detected by demonstrating comparatively reduced intensity of specific gene fragments. For example, patients with 21-hydroxylase deficiency often have deletions of about 30 kb of the 21-hydroxylase/C4 gene cluster. Such pathological deletions eliminate the functional 21-hydroxylase gene, CYP21, and an adjacent C4B gene, leaving the related CYP21P pseudogene and C4A genes. Patients with homozygous deletions will show absence of diagnostic restriction fragments associated with CYP21 and C4B, while carriers of the deletion will show a 2:1 ratio of CYP21P:CYP21 and of C4A:C4B (Collier et al., 1989; Figure). BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 29 30 2.G.3. Northern blotting: Northern blot hybridization is a variant of Southern blotting in which the target nucleic acid is RNA instead of DNA. A principal use of this method is to obtain information on the expression patterns of specific genes. Once a gene has been cloned, it can be used as a probe and hybridized against a Northern blot containing, in different lanes, samples of RNA isolated from a variety of different tissues (see Figure). The data obtained can provide information on the range of cell types in which the gene is expressed, and the relative abundance of transcripts. Additionally, by revealing transcripts of different sizes, it may provide evidence for the use of alternative promoters, splice sites or polyadenylation sites. 2.H. Chromosome banding Chromosome banding is the technique used in cytogenetics. Cytogenetic analysis is a highly skilled laboratory discipline and it takes several years of training. We will restrict this to a basic explanation of the technique. Chromosomes can only be seen in dividing cells, and obtaining dividing cells directly from the human body is difficult. Bone marrow is a possible source, but it is much easier all round to take an accessible source of nondividing cells and culture them in the laboratory. Blood is the material of choice - most people don't mind giving a few millilitres, and the T lymphocytes in blood can be easily induced to divide by treatment with lectins such as phytohemagglutinin. Other common sources include fibroblasts grown from skin biopsies, and (for prenatal diagnosis) chorionic villi or fetal cells shed into the amniotic fluid. Although chromosomes were described accurately in some organisms as early as the 1880s, for many decades all attempts to prepare spreads of human chromosomes produced a tangle that defied analysis. The BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 30 31 key to getting analyzable spreads was a new technique, growing cells in liquid suspension and treating them with hypotonic saline to make them swell. This allowed the first good quality preparations to be made in 1956. White cells from blood are put into a rich culture medium laced with phytohemagglutinin and allowed to grow for 48-72 hours, by which time they should be dividing freely. Nevertheless, because M phase (Figure) occupies only a small part of the cell cycle, few cells will be actually dividing at any one time. The mitotic index (proportion of cells in mitosis) is increased by treating the culture with a spindle disrupting agent such as colcemid. Cells reach M phase of the cycle, but are unable to leave it, and so cells accumulate in metaphase of mitosis. Often it is preferable to study prometaphase chromosomes, which are less contracted and so show more detail. Cell cultures can be prevented from cycling by thymidine starvation; when the block is released the cells progress through the cycle synchronously. By trial and error, the time after release can be determined when a good proportion of cells are in the desired prometaphase stage. Meiosis can only be studied in testicular or ovarian samples. Female meiosis is especially difficult, as it is active only in fetal ovaries, whereas male meiosis can be studied in a testicular biopsy from any postpubertal male who is willing to give one. The results of meiosis can be studied by analyzing chromosomes from sperm, although the methodology for this is cumbersome. Meiotic analysis is used for some investigations of male infertility. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 31 32 Until the 1970s chromosomes were identified on the basis of their size and the position of the centromeres. This allowed chromosomes to be classified into groups but not unambiguously identified. The introduction of banding techniques finally allowed each chromosome to be identified, as well as permitting more accurate definition of translocation breakpoints, subchromosomal deletions, etc. Banding resolution can be increased by using more elongated chromosomes, for example chromosomes from prometaphase or earlier, rather than metaphase. Typical highresolution banding procedures for human chromosomes can resolve a total of 400, 550 or 850 bands (Figure). BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 32 33 Chromosome Banding techniques G-banding - the chromosomes are subjected to controlled digestion with trypsin before staining with Giemsa, a DNA-binding chemical dye. Dark bands are known as G bands. Pale bands are G negative (Figure). Q-banding - the chromosomes are stained with a fluorescent dye which binds preferentially to AT-rich DNA, such as Quinacrine, DAPI (4',6-diamidino-2-phenylindole) or Hoechst 33258, and viewed by UV fluorescence. Fluorescing bands are called Q bands and mark the same chromosomal segments as G bands. R-banding - is essentially the reverse of the G-banding pattern. The chromosomes are heat-denatured in saline before being stained with Giemsa. The heat treatment denatures AT-rich DNA, and R bands are Q negative. The same pattern can be produced by binding GC-specific dyes such as chromomycin A3, olivomycin or mithramycin. T-banding - identifies a subset of the R bands which are especially concentrated at the telomeres. The T bands are the most intensely staining of the R bands and are visualized by employing either a particularly severe heat treatment of the chromosomes prior to staining with Giemsa, or a combination of dyes and fluorochromes. C-banding - is thought to demonstrate constitutive heterochromatin, mainly at the centromeres. The chromosomes are typically exposed to denaturation with a saturated solution of barium hydroxide, prior to Giemsa staining. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 33 34 The chromosome constitution is described by a karyotype that states the total number of chromosomes and the sex chromosome constitution. Human females and males are 46,XX and 46,XY respectively. When there is a chromosomal abnormality the karyotype also describes the type of abnormality and the chromosome bands or subbands affected. Chromosomes are displayed as a karyogram (often loosely described as a karyotype). Karyograms such as shown in the Figure are prepared by cutting up a photograph of the spread, matching up homologous chromosomes and sticking them back down on a card – or nowadays more often by getting an image analysis computer to do the job. Chromosome banding picks out structural organization on a 1-10 Mb scale. Various treatments involving denaturation and/or enzymatic digestion, followed by incorporation of a DNA-specific dye, can cause human and other mitotic chromosomes to stain as a series of light and dark bands. Banding patterns are interesting (as well as being useful to cytogeneticists) because they provide evidence of some sort of structure over 1-10 Mb regions. The banding patterns correlate with other properties. Regions that stain as dark G bands replicate late in S phase of the cell cycle and contain more condensed chromatin, while R bands (light G bands) generally replicate early in S phase, and have less condensed chromatin. Genes are mostly concentrated in the R bands, while the later replicating, more condensed G-band DNA is less active transcriptionally. There are also differences in the types of dispersed repeat elements found in G and R bands. Bands similar to G bands can be produced by staining with quinacrine, which preferentially binds to AT-rich DNA, while the R-banding pattern can be elicited using chromomycin, which preferentially binds GC-rich DNA. However, the AT content of human G band DNA is only a few per cent higher than R band DNA. The differences depend on the differences in the scaffold-loop structure. Chromatin loops are thought to attach to the chromosome scaffold at special scaffold attachment regions (SARs). There are more SARs per unit length of DNA in G bands than in R bands. G bands have smaller loops and a tighter 'queue' of SARs along the scaffold, so that there are more SARs per unit length of chromosome, leading to stronger staining with ATselective stains like Giemsa. Clinical cytogenetics is now established as a vital medical technique enabling the clinical diagnosis of many genetic conditions (such as the Down syndrome). More information in the analysis of the chromosome can be found in “Chromosome Analysis” of the book “The Science of Laboratory Diagnosis” by Crocker and Burnett (ISIS Medical Media, 1999). 2.I. In situ hybridization (ISH) The ISH technique is used to localize specific nucleic acid sequences in the cell (compare to in situ amplification). 2.J.1. Chromosome in situ hybridization: A simple procedure for mapping genes and other DNA sequences is to hybridize a suitable labeled DNA probe against chromosomal DNA that has been denatured in situ. To do this, an air- BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 34 35 dried microscope slide preparation of metaphase or prometaphase chromosomes is made, usually from peripheral blood lymphocytes or lymphoblastoid cell lines. Treatment with RNase and proteinase K results in partially purified chromosomal DNA, which is denatured by exposure to formamide. The denatured DNA is then available for in situ hybridization with an added solution containing a labeled nucleic acid probe, overlaid with a coverslip. Depending on the particular technique that is used, chromosome banding of the chromosomes can be arranged either before or after the hybridization step. As a result, the signal obtained after removal of excess probe can be correlated with the chromosome band pattern in order to identify a map location for the DNA sequences recognized by the probe. Chromosome in situ hybridization has been revolutionized by the use of fluorescence in situ hybridization (FISH) techniques. The sensitivity and resolution of in situ hybridization has significantly increased by the use of FISH. In this technique, the DNA probe is either labeled directly by incorporation of a fluorescentlabeled nucleotide precursor, or indirectly by incorporation of a nucleotide containing a reporter molecule (such as biotin or digoxigenin) which after incorporation into the DNA is then bound by fluorescently labeled affinity molecule. To increase the intensity of the hybridization signal, large DNA probes are preferred, usually cosmid clones containing around 40 kb of insert. Because such large sequences will contain many interspersed repetitive DNA sequences, it is necessary to use chromosome in situ suppression hybridization. Essentially, this is a form of competition hybridization: before the main hybridization, the probe is mixed with a large excess of unlabeled total genomic DNA and denatured, thereby saturating the repetitive elements in the probe,' so that they no longer mask the signal generated by the unique sequences. FISH has the advantage of providing rapid results which can be scored conveniently by eye using a fluorescence microscope. In metaphase spreads, positive signals show as double spots, corresponding to probe hybridized to both sister chromatids (Figure). Using sophisticated image processing equipment and reporter-binding molecules carrying different fluorophores, it is possible to map and order several DNA clones simultaneously. The maximum resolution of conventional FISH on metaphase chromosomes is several megabases. The use of the more extended prometaphase chromosomes can permit 1 Mb resolution but, because of problems with chromatin folding, two differentially labeled probe signals may appear to be side-by-side, unless they are separated by distances greater than 2 Mb. Recently, however, new variations have been developed, permitting very high resolution. There are numerous applications for chromosome FISH. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 35 36 Tissue in situ hybridization: In this procedure, a labeled probe is hybridized against RNA in tissue sections. Tissue sections are made from either paraffin-embedded or frozen tissue using a cryostat, and then mounted on to glass slides. A hybridization mix including the probe is applied to the section on the slide and covered with a glass coverslip. Typically, the hybridization mix has formamide at a concentration of 50% in order to reduce the hybridization temperature and minimize evaporation problems. Although double-stranded cDNAs have been used as probes, single-stranded complementary RNA probes (riboprobes) are preferred: the sensitivity of initially single-stranded probes is generally higher than that of double-stranded probes, presumably because a proportion of the denatured double-stranded probe renatures to form probe homoduplexes. cRNA riboprobes that are complementary to the mRNA of a gene are known as antisense riboprobes and can be obtained by cloning a gene in the reverse orientation in a suitable vector such as pSP64. In such cases, the phage polymerase will synthesize labeled transcripts from the opposite DNA strand to that which is normally transcribed in vivo. Useful controls for such reactions include sense riboprobes which should not hybridize to mRNA except in rare occurrences where both DNA strands of a gene are transcribed. Labeling of probes is performed using either selected radioisotopes, notably 35S, or by nonisotopic labeling (Figure). In the former case, the hybridized probe is visualized using autoradiographic procedures. The localization of the silver grains is often visualized using only darkfield microscopy (direct light is not allowed to reach the objective; instead, the illuminating rays of light are directed from the side so that only scattered light enters the microscopic lenses and the signal appears as an illuminated object against a black background). However, bright-field microscopy (where the image is obtained by direct transmission of light through the sample) provides better signal detection. Fluorescence labeling is a popular nonisotopic labeling approach and detection is accomplished by fluorescence microscopy. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 36 37 A more detailed description of the ISH technique can be found in chapter 51 “In Situ Hybridization” of the book “The Science of Laboratory Diagnosis” by Crocker and Burnett (ISIS Medical Media, 1999). Some commercial kits are available for diagnosis of diseases such as cytomegalovirus, Epstein-Barr virus (more information can be found on http://www.novocastra.co.uk/ish.htm ). BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 37 38 3. Immunological techniques A broad range of immunological techniques have well established applications in the field of medical diagnosis. A good overview of these techniques and some necessary background information can be found in chapter 2 in the book: Immunobiology, Janeway and Travers, Garland Publishing Inc., 1997. 3.A. Serological techniques Essentially serological techniques include all techniques based on the use of antibodies. The term derives from the fact that originally these assays were conducted using the sera from immunized individuals. The use of antibodies is often called serology. Since this description includes almost the entire field of immunological techniques used in medical diagnosis, we will describe in this chapter some “serological techniques” which cannot be classified in one of the chapters below although these chapter also could be classified by the definition under the term serological techniques. 3.A.1 Blood grouping: A commonly used technique for blood grouping, which is very easy in its use is based on a gel system. Gel phase systems rely on trapping the reacted cells in a solid or semi-solid matrix, with negative results falling through the gel. In this system monoclonal antibodies directed against the A, B and D (rhesus system) antigens are chemically bonded to the matrix. Cells containing the corresponding are trapped in the matrix when they are pulled through the gel by centrifugation (see figure). 3.A.2 Latex agglutination: Polysterene latex micro-particles coated with viral (or other antigens) agglutinate when mixed with patient serum containing specific antibody. When a patient has antibodies to a viral antigen this implies that he/she has been infected with the virus. The antigen-coated latex particles are mixed with patient’s serum on a glass slide or in a microtiter well. A visible agglutination pattern appears if specific antibody is present. These tests are in wide use in virus BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 38 39 laboratories because of their speed, simplicity and ease of use. Currently good latex agglutination tests are available for viral antigens such as rubella, toxoplasmose and cytomegalovirus. This test is also used for the diagnose of bacterial infections such as Staphylococcus aureus http://www.bindingsite.com/micro.html . Staphylococcus aureus Rapid Latex test This kit incorporates a slide agglutination procedure for use in the differentiation of Staph. aureus from other staphylococci on the basis of protein A / coagulase production. Polystyrene latex particles are coated with fibrinogen and IgG, and will readily agglutinate in the presence of a suspension of Staph. aureus carrying clumping factor (coagulase) and/or protein A. The kit is available in 100 or 300 test packs which include latex reagent, control reagent, reaction cards and mixing sticks. 3.A.3 Hemagglutination This technique is in fact a variant of the latex agglutination. Here red blood cells are used as the “particle”. The antigens already present on the red blood cell can be used as in the blood grouping test explained on p 2:11 and 2:12 of the chapter in “Immunobiology”. Or the red blood cells can be coated with antigens, an example is the THPA test for Syphilis. 3.A.4 Complement based techniques These techniques use the complement system. This is a very complex system of proteins in our body. A short description of the essentials will be given here. Complement was discovered as a heat-labile component of normal plasma that allows some antibodies to kill bacteria. The complement system is made up of a large number of distinct plasma proteins; one is activated directly by bound antibody to trigger a cascade of reactions each of which results in the activation of another complement component. Some components of this complement system, especially the terminal complement components are able to directly kill cells by creating pores in their membrane. Especially bacteria and red blood cells are sensitive to complement killing. However under some conditions also nucleated cells get killed by the complement. A widely used example of the use of this technique is the traditional serological HLA-typing. Until recently, the 'traditional' method used to distinguish HLA non-identical individuals employed antibody. HLA-A and -B locus antigens were the first to be defined in this manner, using alloantisera obtained from subjects immunized by blood transfusions pregnancy or renal allograft rejection. Using this technique, called a microcytotoxicity assay, peripheral blood T lymphocytes (HLA class I BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 39 40 antigens) and B lymphocytes (HLA-DR, -DQ) from potential allograft recipients of unknown HLA type are incubated with antiserum of characterized HLA specificity. These cells are then exposed to complement. If antibody reacts with HLA proteins expressed on the cell surface, complement is activated and the cells are killedcomplement mediated lysis. In the absence of reaction no lysis occurs. Killing is visualized usually by a two-colour fluorescent dye system, one of which labels all viable cells green. The other can only penetrate killed cells, labelling them red, therefore killing is assessed semiquantitatively by loss of green cells and is usually expressed as a percentage. Thus, where lysis occurs, the specificity of the antibody identifies which HLA proteins are expressed. Several types of error are possible with serological typing. A failure to identify a rare or crossreactive antigen is a frequent problem. This is principally because the relevant antisera either have not been used, or are not available. Linkage disequilibrium, geographical origins and racial breeding patterns are contributing factors, moreover some antigens are expressed at a lower frequency or not at all in certain populations. Such errors are most likely to occur in laboratories using limited numbers of antisera. In addition, a misinterpretation of antiserum reactions can also produce errors. Antiserum may contain more than one antibody, each with differing HLA specificities and even monospecific HLA antibodies frequently cross-react with other HLA antigens. Furthermore HLA typing of DR antigens using serology is particularly susceptible to misinterpretation since B lymphocytes are both more cross-reactive to a wide range of DR antigens and more susceptible to non-specific complement mediated lysis, giving rise to 'falsepositive' results. Technical variations also account for a 15-30% inter-laboratory error in serological typing. Variation in complement activity between batches and quality of antiserum are the main contributory factors. Serotyping is a rapid method for HLA genotyping, however, the reagents used are not specific enough to determine the precise structural identity of MHC molecules in genetically non-identical individuals. This can only be achieved by direct analysis of the MHC genes themselves. 3.A.5 Line Immunoassay (LIA) This provides a highly specific and sensitive tool for detecting and characterizing specific antibodies to microorganisms or other antigens by virtue of their binding to antigens that have been affixed to nitrocellulose membranes. The antigens are produced by recombinant molecular techniques or artificially synthesized (synthetic peptides) and are then directly attached to a nitrocellulose membrane. The nitrocellulose membrane is then incubated with patient’s serum to allow antibody to bind to the antigens fixed to the membrane. Enzyme-labeled anti-human immunoglobulin is then added on a principle similar to that of ELISA. BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 40 41 Appropriate washing steps are included. On addition of substrate, antigen bands, to which specific antibody is present, become visible. The technique is unique in that antibody to single viral or bacterial proteins or other antigenic epitopes can be detected, hence making the test very specific. Commercial tests are available for the detection of HIV, Hepatitis C and human T-cell lymphotropic virus antibodies. LIA tests are also available for the detection of auto-antibodies implicated in an important group of autoimmune diseases: Sjogren's syndrome, systemic lupus erythematosus, drug induced lupus, diffuse scleroderma, mixed connective tissue disease, CREST, polymyositis/dermatomyositis. http://www.innogenetics.be/Website/Website.nsf/7df3b6bb9c0862e8c1 2567380052687f/e1e06bbd2ad052aec12569a700578ce8?OpenDocume nt 3.A.6 Western blotting This technique is described on p 2:23 of the chapter in “Immunobiology”. Western blotting is applied to the field of virology for the detection of the presence of antibodies specific for certain viruses (much as in the LIA assays). Western blotting can also be used to detect in stead of the presence of antibodies in a sample, the presence of certain antigens in a sample. It the latter setting the membrane is screened with specific monoclonal antibodies. In this setting it is also used for the diagnosis of prion infection. 3.B. ELISA The basics of the ELISA technique are explained on pages 2:9 to 2:10 of the chapter in “Immunobiology”. ELISA is such a basic technique that we will not further discuss the principles of the technique in this course. ELISA is probably also the most widely used technique in medical diagnosis. ELISA kits are commercially available for the detection and quantification of so much targets that giving a list is useless and impossible. Just as an example we would like to refer to an ELISA test for the detection of EPO in patient’s serum http://biochem.roche.com/packinsert/1693417A.pdf . A bit more explanation on variants of the ELISA technique used in diagnostics can be found on pages 218-219 in The science of Laboratory Diagnosis, John Crocker and David Burnett, ISIS Medical Media, 1999. 3.C. Flowcytometry Flowcytometry is another widely used technique in medical diagnostics, especially in the field of haematology. The background information on the technique and the machinery has been touched in the course “Biologisch-farmaceutische analyse”. For the application of flowcytometry to medical diagnosis monoclonal antibodies are used to study the presence of specific markers on cells, which can be BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 41 42 indicative of disease processes or of specific cells. These antibodies are labeled with fluorescent markers which can be detected by the flowcytometer. See also p 2:27 to 2:30 of the chapter in “Immunobiology”. Some applications of flowcytometry to haematology are discussed in Chapter 32 of The science of Laboratory Diagnosis, John Crocker and David Burnett, ISIS Medical Media, 1999. An immense array of antibodies with different fluorescent labels specially designed for flowcytometry are commercially available. One of the big suppliers is Pharmingen http://www.pharmingen.com . BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 42 43 4. European legislation http://europa.eu.int/eur-lex/en/lif/dat/1998/en_398L0079.html BIOTECHNOLOGICAL TECHNIQUES IN MEDICAL DIAGNOSIS 43