Clinical Case Chest Pain
advertisement
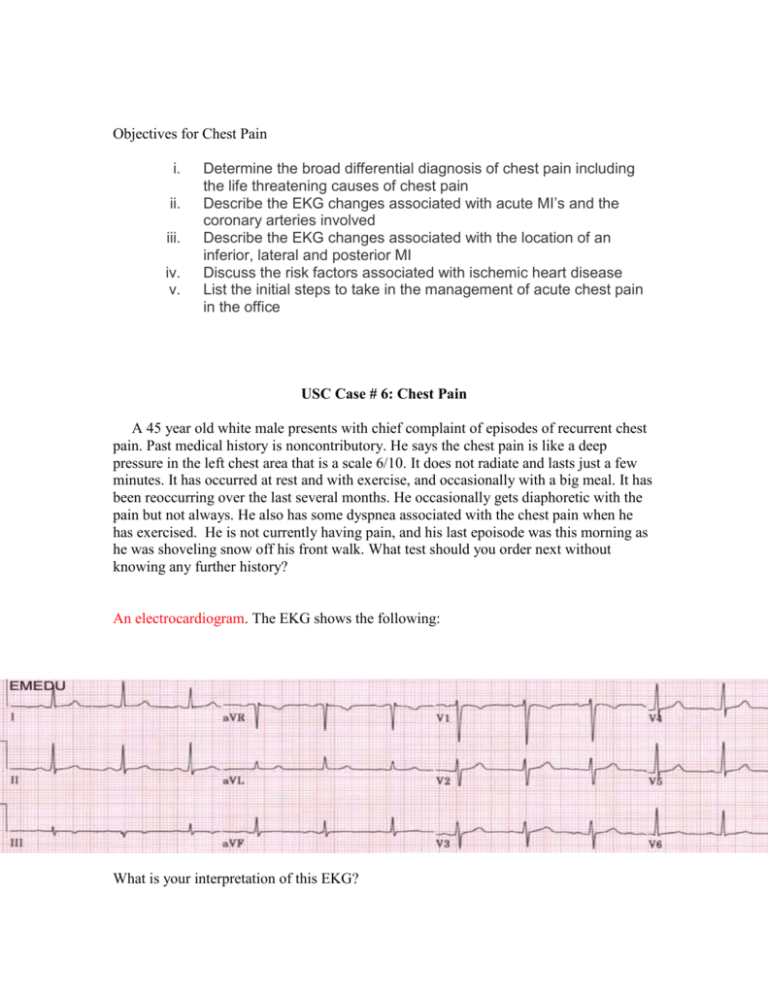
Objectives for Chest Pain i. ii. iii. iv. v. Determine the broad differential diagnosis of chest pain including the life threatening causes of chest pain Describe the EKG changes associated with acute MI’s and the coronary arteries involved Describe the EKG changes associated with the location of an inferior, lateral and posterior MI Discuss the risk factors associated with ischemic heart disease List the initial steps to take in the management of acute chest pain in the office USC Case # 6: Chest Pain A 45 year old white male presents with chief complaint of episodes of recurrent chest pain. Past medical history is noncontributory. He says the chest pain is like a deep pressure in the left chest area that is a scale 6/10. It does not radiate and lasts just a few minutes. It has occurred at rest and with exercise, and occasionally with a big meal. It has been reoccurring over the last several months. He occasionally gets diaphoretic with the pain but not always. He also has some dyspnea associated with the chest pain when he has exercised. He is not currently having pain, and his last epoisode was this morning as he was shoveling snow off his front walk. What test should you order next without knowing any further history? An electrocardiogram. The EKG shows the following: What is your interpretation of this EKG? Normal Sinus Rhythm . Chest pain can often be the presenting symptom of a life threatening condition. What are five major life threatening diagnoses that you must consider when a patient presents with chest pain? Pulmonary embolus Ischemic heart disease or cardiac problems (e.g. pericarditis, aneurysms) Pneumothorax Esophageal rupture Dissecting aortic aneurysm If the patient appears to be in distress, obtain O2 saturation and chest x-ray initially in addition to the EKG. Clinicians must avoid premature diagnosis of acute coronary syndrome (ACS). ●If acute coronary syndrome (ACS) is the leading diagnosis, initial assessment and interventions must be performed rapidly to minimize potential injury to the myocardium. During the initial assessment phase, the following steps should be accomplished for any patient at significant risk for ACS: •Airway, breathing, and circulation assessed Arrange for transfer to emergency Department •Preliminary history and examination obtained •12-lead electrocardiogram (ECG) interpreted •Resuscitation equipment brought to the bedside •Cardiac monitor attached to patient •Oxygen given •IV access and blood work obtained •Aspirin 162 to 325 mg given •Nitrates and morphine given (unless contraindicated ●The initial ECG is often NOT diagnostic in patients with ACS. In patients without a clear diagnosis but at risk for ACS, ECGs may be repeated at frequent intervals (every 10 to 15 minutes) until the patient's chest pain resolves or a definitive diagnosis is made. ECG assessment is described in the text. ●Certain characteristics of the patient's chest discomfort and associated symptoms increase the likelihood of ACS, while others make the diagnosis unlikely.. Caution should be employed in evaluating possible ACS in women, diabetics, and the elderly, who are more likely to present with "atypical" symptoms even in the presence of acute coronary ischemia. Of note, relief of symptoms following the administration of therapeutic interventions (eg, nitroglycerin, "GI cocktail" of viscous lidocaine and antacid) does NOT reliably distinguish nonischemic from ischemic chest pain. ●The initial physical examination should focus on findings that permit rapid triage and aid in immediate diagnosis and management. Initial laboratory work should include: serum cardiac biomarkers (cTnI or cTnT (troponins) CKMB preferred), CBC with platelet count, PT and INR, PTT, electrolytes, magnesium, BUN, creatinine, blood glucose, and serum lipid profile. ●Approximately 2 to 4 percent of patients with an ACS are mistakenly discharged from the office or emergency department; these patients have an increase in short-term mortality. Patients whose ACS was missed were more likely to be women less than 55 years of age, non-whites, patients with shortness of breath as the major presenting symptom, and patients with a normal or nondiagnostic initial ECG. __________________________________________ The patient appears not to be in distress. He is a good historian and is not presently having chest pain. History: ROS: negative except for chest pain, diaphoresis and dyspnea with exertion. PMH: tobacco abuse, possibly a high cholesterol taken at a health fair. PSH: none FMH: father living with hypertension, mother NIDDM, siblings healthy, maternal grandfather deceased with stroke, maternal grandmother deceased Alzheimer’s dementia, paternal grandparents living in their 90’s with good health. Social hx: married, 2 sons (3,5 y.o.), works as a mechanic, he does not exercise, smokes 2 packs per day for 27 years, drinks 1 beer a month. Allergies: NKDA Meds: none Immunization hx: up to date with last tetanus 2 years ago. Pain: scale 6/10 left chest deep pressure non-radiating, last 2-3 minutes at rest and exercise, occasional dyspnea and diaphoresis, no certain things relieve the pain. Physical Exam BP 145/95, P 85, R 16, T 98.6, HT 6’0”, WT 265 Gen : Alert and oriented x 3, pleasant, obese. Skin: warm, moist, pink. HEENT: normal except for slight A/V nicking and arteriole atherosclerosis on the Fundoscopic exam. Heart: regular, rate and rhythm without murmur, no carotid bruits. Lungs: bilaterally clear to auscultation with decreased breath sounds diffusely. Abdomen: soft, nontender, normal bowel sounds x 4, no masses, no organomegaly, no bruits. Extremities: no cyanosis, no edema, good pulses. Back: normal Genitalia: normal Rectal: heme negative, no masses, prostate soft Neuro: No focal deficits Osteopathic: Thoracic T2 SlRr LABS: CBC: wbc 10.5, hgb 15.5, hct 46.5, platelets 245,000, MCV 95 CMP: glucose 127, remaining normal Lipid: HDL 20, LDL 185, CHOL 285, TG 325 (all labs fasting) How many risk factors does he have for heart disease? Answer: 7 1. 2. 3. 4. 5. 6. 7. High blood pressure Obesity Family medical history Diabetes mellitus (fasting blood sugar greater than 126) Hyperlipidemia ( elevated chol, low HDL, high LDL, high TG all risks) Male gender Tobacco abuse The patient is referred to a cardiologist to be seen as soon as possible but refuses to see him till he has a day off which is three weeks away. He is warned of the risk factors involved of not seeing him in a timely manner. All his risk factors are discussed with counseling on diet, blood sugar control and smoking. He states he will try to be better, and refuses any kind of medication because his grandfather took some heart and cholesterol pills and had problems. The Hgb A1C test for his diabetes is pending at the time he is discharged. He is instructed not to do any strenuous labor until evaluated by cardiology with stress testing pending. Two weeks later the patient presents again with chest pain that will not stop. This time the pain is a scale 9/10 with a pressure that feels like an elephant sitting on his chest. It radiates to his left arm and he is very diaphoretic. He denies any dyspnea, but states he is very nauseated. He started having chest pain at home while digging up a tree. An ambulance is called for but there is only one in the area and the patient will have to wait till one can arrive. An intravenous access line is started . An O2 saturation is done showing 98% saturation on room air and the patient is placed on nasal cannula oxygen at 3 lpm. A chest xray is done which is normal. He has an ekg done which shows the following. What’s your diagnosis? Answer: Acute inferior infarction. The patient has classic ST-segment elevation in leads II, III and AVF. He appears to have normal sinus rhythm. There are no Q-waves in these leads, but it is does not have to be present especially in the early phases of a myocardial infarction. Q-waves usually coincide with the development of cell necrosis which may occur within hours to days and persistent on an ekg with loss of the ST segment elevation. 20% of patients presenting with acute MI have a normal ekg and history should play an important role determining treatment and testing. 20-30% of patients with acute MI are completely asymptomatic at the onset of coronary occlusion. Some ST segment changes are seen in V1, V2 and can occur occasionally with inferior infarcts. The patient had nausea with the chest pain. Why? Inferior infarcts involve the inferior portion of the heart which sits on the diaphragm. Irritation or somato-somatic reflexes could cause nausea and vomiting due to adrenergic innervation through common pathways. What’s the sympathetic level of innervation to the heart? What is the parasympathetic innervation to the heart T 1-5 (some textbooks state T2-5 on the left) sympathetic. Vagus nerve parasympathetic. What artery is most likely to be involved in an inferior infarct? What arteries are involved in infarcts to other areas of the heart and their ekg changes? What are some of the ekg changes associated with ischemia? What laboratory tests would indicate a myocardial infarction? Troponin appearing in 3-6 hours CK isoenzymes MB appearing 4-8 hours LDH within 24 hours and AST Erythrocyte Sedimentation Rate appearing 3 days after Leukocytes within several hours and peaking within 2-4 days (if your in a rural area a stat CBC may give you a hint of possible myocardial infarction) Risk factors for arteriosclerotic heart disease (ASHD) should be evaluated on every patient that is seen in an outpatient setting. These should be addressed and treated as possible. This patient had multiple risk factors with most of them being treatable. Name some of the risk factors for ASHD? Risk Factors -Elevated low density lipoprotein (LDL) -Decreased high density lipoprotein (HDL) -Elevated triglycerides -Smoking -Family history -Hypertension -Diabetes mellitus -Sedentary lifestyle -Stress -Obesity -Increasing age -Male sex -Metabolic syndrome -Multiple other risk factors with new evidence being found This patient had multiple risk factors falling under the heading of metabolic syndrome with many of these factors correctable. A sedentary lifestyle is a major factor for heart disease and recent studies have shown an obese person who exercises regularly has less risk than a thin person who lives a sedentary lifestyle. Diabetes mellitus is a major risk factor for heart disease. Most diabetics die from large vessel disease. Maintaining an active lifestyle and controlling blood sugar levels with a Hemoglobin A1C level below 6.5 greatly decreases the risks. Prediabetics probably have a greater risks and future Hgb A1C levels may be dropped even further. Hyperlipidemia is a treatable risk factor and should be addressed in every patient who you see in your office. Recent studies have lowered the LDL levels below 100 and may possibly be below 70 to reduce the progression of atherosclerosis. Hypertension is a treatable disease. A systolic pressure below 130 and diastolic below 85 are the only acceptable numbers. The morbidity and mortality increase in a linear proportion as the blood pressure elevates. The pulse pressure (difference between systolic and diastolic pressure) is a risk factor for vascular disease and should be addressed especially in the elderly population, as many elderly believe that only the diastolic pressure is important as a risk factor. Smoking risks have been well studied and is a preventable problem if the patient is willing to quit. Chewing tobacco has risks also as levels of nicotine may be as high as 20X that found with smoking. There are factors which we have not discovered that contribute to heart disease. Genetic history appears to contribute greatly to the problem. Some research suggests inflammation may be a large contributor to heart disease. 50% or greater people who die from myocardial infarction have normal coronary arteries, and soft plaques or inflammation may cause thrombosis with secondary infarction. Recent studies also have shown non-occlusive coronary artery disease has almost a high risks of morbidity and mortality as occlusive coronary artery disease. This patient was transferred to the hospital and had an excellent outcome. Inferior wall MI usually has a good prognosis as compared to most other MIs. Post treatment should be aggressive to decrease the risk factors involved. Cardiac rehab whenever possible should be started post MI. Prevention of coronary artery disease should start early in life with most factors being modifiable. Counseling early on about multiple risk factors should be addressed and corrected. Heart disease is the number one cause of death in the United States and prevention should be a major objective of physicians. Reading: Rakel’s Textbook of Family Medicine pp 529 - 541