Chest Pain - Penn Medicine - University of Pennsylvania
advertisement

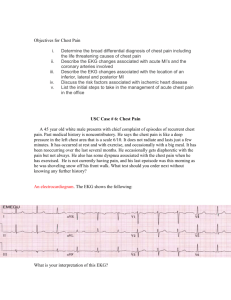
Benjamin S Abella, MD MPhil Department of Emergency Medicine University of Pennsylvania Benjamin.abella@uphs.upenn.edu CC: Chest pain vs. 1. ABC’s/Stabilization/Resuscitation IV, O2, monitor, pulse oximeter 2. ECG 3. +/- CXR CC: Chest pain 64 year old man presents with 5 hours of SS chest pressure associated with SOB, nausea and diaphoresis. Gradual onset while shoveling the snow. Improved with rest. PMH: HTN, DM Gen: Nontoxic appearing, apprehensive, mildly diaphoretic Vitals: 37.5ºC, RR16, HR 100, BP 160/95 CVS: RRR, Normal S1, S2, no M/R/G Resp: CTAB, easy respirations Abd: Soft, NTND Ext: No calf tenderness or swelling, no edema, strong distal pulses MedPixTM Epidemiology >6,000,000 Americans have CAD 500,000 deaths/yr. in the U.S. from CAD 250,000 pts. with prehospital cardiac arrest ▪ 6% survive to hospital discharge >4,000,000 E.D. visits per year for acute chest pain $100 billion per year Etiology Ischemia: imbalance between oxygen demand and oxygen supply Fixed atherosclerotic lesion vs. plaque disruption with platelet/thrombi aggregation vs. spasm Stable angina: transient, episodic chest discomfort that is predictable and reproducible. Unstable angina: angina that is new in onset, occurs at rest or is similar but somewhat “different” than previous episodes. Acute myocardial infarction Substernal chest discomfort > 15 minutes associated with dyspnea, diaphoresis, lightheadedness, palpitations, nausea and/or vomiting NSTEMI STEMI 12.5% of acute MI’s are clinically “silent” Smoking Hypertension Diabetes mellitis Hypercholesterolemia Family history of CAD prior to age 55 in a firstdegree relative Previous history of CAD or peripheral vascular disease Cardiac risk factors are very poor predictors of risk for ACS in the E.D Not helpful in distinguishing patients with ACS from those with noncardiac chest pain unless an alternative diagnosis is clear e.g. pneumothorax Normal cardiopulmonary exam is most common S3 in 15-20% with AMI Chest wall tenderness to palpation in ~15% with ACS The standard ECG is the single best test to identify patients with an AMI upon E.D. presentation But sensitivity is still far from ideal ST elevation in 50% of AMI’s 1-5% of AMI’s have a normal initial ECG 4 - 23% of pts. with unstable angina have a normal ECG CK-MB Sensitivity > 90% for MI 5-6h after symptom onset 50% sensitive shortly after presentation Troponin Tn-I: similar sensitivity and specificity to CK-MB for AMI in E.D. patients Tn-T: less sensitive for myocardial injury ▪ Independent marker of cardiovascular risk Marker Elevation Peak Duration CK-MB 3-12 h 18-24 h 2 days Troponin-I 3-12 h 18 h 5-10 d Troponin-T 3-12 h 12 h 5-14 d Aspirin Inhibits thromboxane A2 … decreases platelet aggregation Nitrates Decreases preload and afterload; increases coronary perfusion in obstructed vessels Beta blockers Decreases infarct size, cardiovascular complications, and mortality Consider heparin (or enoxaparin), antiplatelet agents, GIIb/IIIa inhibitors Fibrinolysis or PCI ST elevation > 0.1 mV in two or more continguous leads or new LBBB Time to therapy < 12 hours (Class I), 12-24 hours (Class IIb) Door to balloon time Epidemiology: 6% of pts. with cocaine-associated chest pain have an AMI 20-60% have transient myocardial ischemia Often atypical chest pain Can be delayed for hours to days after the most recent use Spasm Increased myocardial oxygen demand Clot formation Accelerated atherosclerosis and LVH Diagnosis: ECG less sensitive and specific for MI CK-MB less sensitive Troponin I may be more useful Prognosis: Favorable short-term prognosis 1 year mortality primarily due to comorbidities and/or continued cocaine use Treatment: Benzodiazepines Avoid Beta blockers >4 million E.D. visits per year for acute chest pain <15% with ACS 2-6% sent home from ED ultimately with ACS Chest pain units/Obs CC: Stroke 51 year old woman brought in by EMS with acute onset of right sided weakness and aphasia. PMH: HTN Gen: Somnolent, diaphoretic Vitals: 37.5ºC, RR16, HR 110, BP 180/110 CVS: Tachy, Normal S1, S2, no M/R/G Resp: CTAB, easy respirations Abd: Soft, NTND Ext: No calf tenderness or swelling, no edema, weak distal pulses Neuro: Right leg/arm 4/5 strength, +expressive aphasia Definition: Intimal tear with entry of blood into the media “dissects” between the intima and adventitia #1 site: ascending aorta at the ligamentum arteriosum Stanford Classification: A: involves Ascending aorta (w/ or w/o descending) ▪ 80% of dissections B: descending aorta only DeBakey Classification Increased risk: Group A: >50 yoa with hypertension Group B: younger pts. with Marfan’s, Ehler-Danlos, pregnancy Mortality Type A: ▪ Untreated: 75% ▪ Surgically treated: 15-20% Type B: ▪ 32-36% with or without surgery History: >90% with abrupt and severe pain in the chest or between the scapulae ▪ “tearing” or “ripping” ▪ Can be dull or pressure-like ▪ Anterior chest ~ ascending aorta; Back ~ descending Nausea, vomiting, diaphoresis common Associated symptoms based on progression of dissection: ▪ ▪ ▪ ▪ Carotid arteries: stroke Spinal arteries: paraplegia Abdominal aorta/renal arteries/iliacs: Abdominal/flank pain Coronary arteries: aortic insufficiency; pericardial effusion/tamponade ▪ Laryngeal nerve compression: hoarseness ▪ Tracheal compression: dyspnea/stridor/wheezing ▪ Esophageal compression: dysphagia Physical Exam: Symptoms/signs as above Most commonly: normal heart and lungs ▪ Aortic insufficiency murmur in 16-20% Unequal, decreased, or absent peripheral pulses only found in 50% CXR 85% with some abnormality ▪ widened mediastinum most common ▪ left pleural effusion; indistinct aortic knob; displaced, calcified intima > 6mm from outer aortic wall CT vs. TEE vs. aortogram Considering it? 2 large bore IV’s, monitor, T&C, ECG Blood pressure: Decrease the shear force on the intima to minimize progression ▪ Lower arterial blood pressure ▪ Decrease LV contractility Goal: SBP 100-110 mm Hg; HR 60-80 Options: A. Nitroprusside + esmolol B. Labetalol Early CT surgery involvement CC: Chest pain 40 year old woman brought in by EMS with acute onset pleuritic right sided chest sharpness associated with SOB. PMH: HTN Gen: Well appearing, mildly uncomfortable Vitals: 38ºC, RR 22, HR 120, BP 150/85 CVS: RRR, Normal S1, S2, no M/R/G Resp: CTAB, easy respirations Abd: Soft, NTND Ext: No calf tenderness but mild left-sided swelling, no edema, strong distal pulses MedPixTM 650,000 cases/year in the U.S. Mortality 2-10% if diagnosed and treated 30% if undiagnosed #3 cause of death overall #1 cause of nonsurgical maternal death in the peripartum period The source is lower extremity DVT in 80-90% of cases Upper extremity DVT in 10-15% Others: pelvic vein thrombosis; fat emboli; septic emboli; right heart thrombosis Virchow’s triad: 1. Venous stasis ▪ Prolonged travel; bed rest; etc. 2. Hypercoagulability ▪ Pregnancy; malignancy; estrogen therapy; deficiencies of protein C, protein S, AT III 3. Endothelial damage ▪ Recent surgery, trauma #1 risk factor = prior DVT/PE 10-15% of patients will have no identifiable risk factor at the time of presentation “Classic Triad”: Dyspnea, hemoptysis, pleuritic CP in only 20% of pts. Three notable findings: Pleuritic chest pain in 74% Dyspnea in 84% Respiratory rate > 16 in 92% Heart rate > 100 in only 44% Kline, 2003 Often normal > 40% with nonspecific ST and T wave abnormalities Sinus tachycardia is the most common rhythm disturbance. S1Q3T3 is seen in only 6% of patients with PE. Normal in ~30% and a concerning finding in the setting of dyspnea and hypoxemia w/o RAD Atelectasis in ~50% Elevated hemidiaphragm in 40% Hampton’s Hump: Pleural based wedge shaped infiltrate Westermark sign: Proximally dilated pulmonary artery with abrupt cut-off Needed for subsequent interpretation of the V/Q scan Clinical Likelihood Probability, % Scan Category High High Indeterm Low All 96 88 56 87 Intermediate 66 28 16 30 Low 40 16 4 14 Normal 0 6 2 4 Total 68 30 9 28 Normal Ventilation Abnormal Perfusion LE Doppler US Pulmonary angiography Spiral CT MRI Garg, 1999 Considering it: IV, O2 prn, monitor, pulse ox. High pretest probability: Anticoagulate 1st, then order your study Heparin 80 U/kg i.v. bolus; 18 U/kg/hr i.v. drip Low (+/- intermediate) pretest probability: Study 1st, then anticoagulate if appropriate Consider thrombolytics if unstable CC: “can’t catch my breath” 40 year old man presents with acute onset of SOB and pleuritic right sided chest sharpness. PMH: none Gen: Mildly uncomfortable Vitals: 37ºC, RR 22, HR 120, BP 145/95 CVS: Tacky, Normal S1, S2, no M/R/G Resp: Decreased bs on the right, tachypeic Abd: Soft, NTND Ext: No calf tenderness or swelling, no edema, strong distal pulses Especially tall, thin male smokers Only 10 – 20% occur with exertion Most thought to result from rupture of a subpleural bleb Symptoms vary with size and rate of progression of pneumothorax Acute pleuritic CP in 95% Dyspnea in 80% Decreased breath sounds over the affected lung in 85% Tachypnea > 24 in only 5% Hyperresonance in <1/3 Tension pneumothorax: Clinical presentation of pneumothorax with hemodynamic compromise Treatment is immediate needle decompression “Non-tension” spontaneous pneumothorax Upright PA CXR is 83% sensitive Tube thoracostomy Minicatheter or standard chest tube Catheter aspiration Single or sequential Observation x 6 hrs. with repeat CXR: o Stable; minimal/no symptoms; <25% ptx o No significant comorbidities Remember the “Big Five” life threatening causes of chest pain Acute coronary syndrome Aortic dissection Pulmonary embolism Tension pneumothorax Esophageal rupture ABCs; IV, O2, monitor, pOx The diagnosis of ACS/PE/dissection may be subtle.