SOAP Note Review: Medical Documentation Guide
advertisement
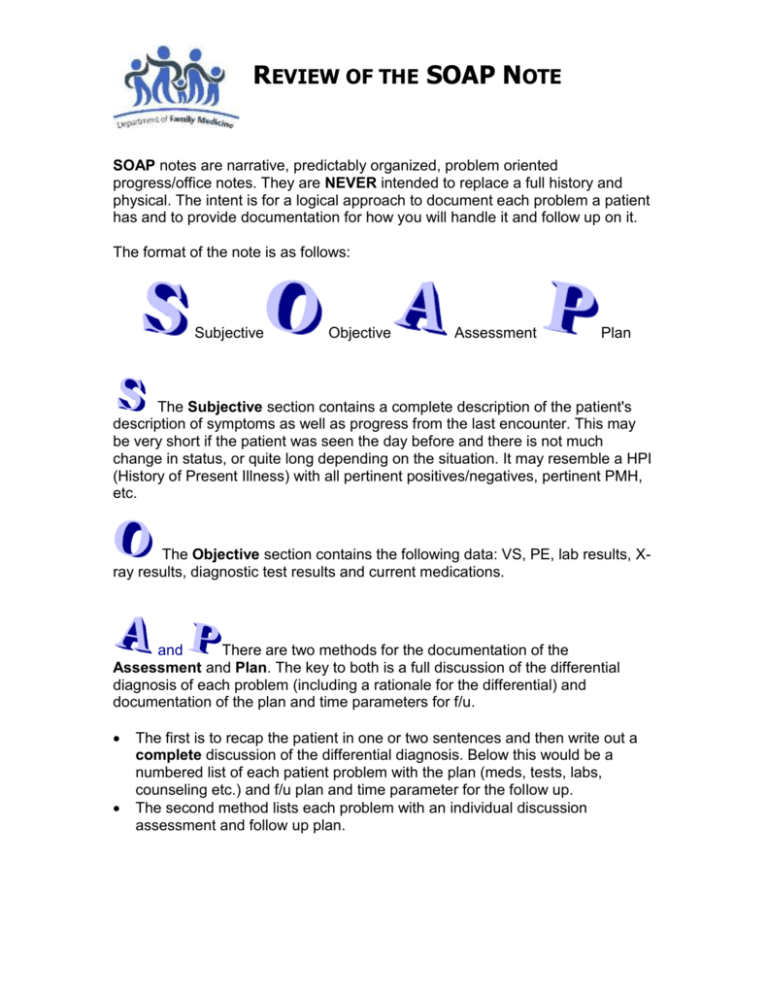
REVIEW OF THE SOAP NOTE SOAP notes are narrative, predictably organized, problem oriented progress/office notes. They are NEVER intended to replace a full history and physical. The intent is for a logical approach to document each problem a patient has and to provide documentation for how you will handle it and follow up on it. The format of the note is as follows: Subjective Objective Assessment Plan The Subjective section contains a complete description of the patient's description of symptoms as well as progress from the last encounter. This may be very short if the patient was seen the day before and there is not much change in status, or quite long depending on the situation. It may resemble a HPI (History of Present Illness) with all pertinent positives/negatives, pertinent PMH, etc. The Objective section contains the following data: VS, PE, lab results, Xray results, diagnostic test results and current medications. and There are two methods for the documentation of the Assessment and Plan. The key to both is a full discussion of the differential diagnosis of each problem (including a rationale for the differential) and documentation of the plan and time parameters for f/u. The first is to recap the patient in one or two sentences and then write out a complete discussion of the differential diagnosis. Below this would be a numbered list of each patient problem with the plan (meds, tests, labs, counseling etc.) and f/u plan and time parameter for the follow up. The second method lists each problem with an individual discussion assessment and follow up plan. REVIEW OF THE SOAP NOTE The SOAP note should include the following: a differential diagnosis (for new sx) a rationale for the differential medications prescribed note that side effects of medications were discussed - documentation of patient education follow up interval noted warnings regarding complications of condition warranting re-contact A "gold-standard" SOAP note will have a differential (if the problem is as of yet undiagnosed) and a brief discussion of the rationale for the differential diagnosis. You should use this format during this clerkship, and after. Examples of SOAP note formats: First Style: S: Ms Smith, 25 year old female, presents to the office with a complaint of right lower quadrant pain increasing in intensity over the last 12 hours. She states she was well until around 8PM last evening when she developed a dull achy pain in the periumbilical region which shortly localized to the right lower quadrant. It has increased in intensity gradually through the night and she thinks that she slept very little. There is no radiation. She is slightly nauseated but has had no vomiting, diarrhea, cramping, flatulence or dysuria. She and her boyfriend had leftover chicken last night for dinner and he shows no signs of illness. She has no appetite this morning. Her LMP was 2 weeks ago with her last period being light but otherwise normal. She has had no bleeding since. Ms Smith uses condoms only for birth control and is in a monogamous relationship. Her boyfriend has no history of or symptoms of a sexually transmitted disease. She has not traveled in two years and currently works as a computer analyst in a small information technology company. Her only med is a MVI daily. She smokes 1PPD and does not use other drugs or alcohol. She has had no previous surgery. REVIEW OF THE SOAP NOTE O: HEENT: Lungs: Cor: Abd: Rectal: Pelvic: Extremities: tired and anxious appearing woman T: 100, FP:90, BP:110/70 Pale, slightly dry mucous membranes Clear Regular rate and rhythm with no murmurs, gallops or rubs Occasional bowel sounds, tender right lower quadrant with slight rebound tenderness, no palpable masses, no hepatosplenomegaly/. No CVA tenderness no tenderness, quaiac negative Cervix appears normal with no obvious d/c. Tenderness without mass or fullness in the R culdesac with mild cervical motion tenderness Normal Neurologic Exam Screening normal A: Ms Smith presents with RLQ pain of 12 hour duration. She has tenderness and slight rebound with tenderness in the R culdesac as well and a low grade fever. Possibilities include acute appendicitis, R ovarian torsion, middleschermz, ectopic pregnancy, PID , or a viral syndrome. Given the lack of d/c and the very minimal cervical motion tenderness PID is less likely. Ovarian torsion is a possibility although the pain has been so constant and with torsion there can be an intermittent quality. Middleschermz and viral syndromes are diagnosis of exclusion. With the lack of urinary symptoms or CVA tenderness it is unlikely that she has UTI of pyelonephtitis. P: #1 Abdominal Pain: Obtain CBC with differential, UA, stat urine pregnancy test (if negative send blood for HCG) . Obtain surgical consult for pain with rebound #2 Contraception: Will make appointment to see patient when out of acute situation to discuss other options for birth control in addition to condoms. #3 Tobacco abuse: will discuss at f/u visit for #2 REVIEW OF THE SOAP NOTE Second Style: S: Ms Smith, 25 year old female, presents to the office with a complaint of right lower quadrant pain increasing in intensity over the last 12 hours. She states she was well until around 8PM last evening when she developed a dull achy pain in the periumbilical region which shortly localized to the right lower quadrant. It has increased in intensity gradually through the night and she thinks that she slept very little. There is no radiation. She is slightly nauseated but has had no vomiting, diarrhea, cramping, flatulence or dysuria. She and her boyfriend had leftover chicken last night for dinner and he shows no signs of illness. She has no appetite this morning. Her LMP was 2 weeks ago with her last period being light but otherwise normal. She has had no bleeding since. Ms Smith uses condoms only for birth control and is in a monogamous relationship. Her boyfriend has no history of or symptoms of a sexually transmitted disease. She has not traveled in two years and currently works as a computer analyst in a small information technology company. Her only med is a MVI daily. She smokes 1PPD and does not use other drugs or alcohol. She has had no previous surgery. O: HEENT: Lungs: Cor: Abd: Rectal: Pelvic: Extremities: tired and anxious appearing woman T: 100 F, P:90 BP: 110/70 Pale, slightly dry mucous membranes Clear Regular rate and rhythm with no murmurs, gallops or rubs Occasional bowel sounds, tender right lower quadrant with slight rebound tenderness,no palpable masses, no hepatosplenomegaly/. No CVA tenderness no tenderness, quaiac negative Cervix appears normal with no obvious d/c. Tenderness without mass or fullness in the R culdesac with mild cervical motion tenderness Normal Neurologic Exam Screening normal REVIEW OF THE SOAP NOTE A&P: #1 Abdominal Pain: Ms Smith presents with RLQ pain of 12 hour duration. She has tenderness and slight rebound with tenderness in the R culdesac as well and a low grade fever. Possibilities include acute appendicitis, R ovarian torsion, middleschermz, ectopic pregnancy,PID, or a viral syndrome. Given the lack of d/c and the very minimal cervical motion tenderness PID is less likely. Ovarian torsion is a possibility although the pain has been so constant and with torsion there can be an intermittent quality. Middleschermz and viral syndromes are diagnosis of exclusion. With the lack of urinary symptoms or CVA tenderness it is unlikely that she has UTI of pyelomephtitis 1. Obtain CBC with differential, UA, stat urine pregnancy test (if negative send blood HCG) 2. Obtain surgical consult for pain with rebound #2 Contraception: Will make appointment to see patient when out of acute situation to discuss other options for birth control in addition to condoms. #3 Tobacco abuse: will discuss at f/u visit for #2