Cartilage and Bone histology
advertisement

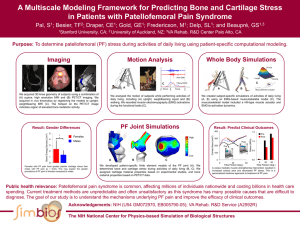
Dr. Abdulla ------------------------------------Histology----------------------------2ststage 1 Cartilage is a specialized form of connective tissue that forms the "skeletal" basis of some parts of the body. Cartilage can endure considerably more stress than loose and dense connective tissues. However, it is not rigid and hard like bone, these features due to the matrix that consist of a dense network of collagen fibers and elastic fibers firmly embedded in chondroitin sulfate, a gel like component of the ground substance. The cells of mature cartilage, called chondrocytes occur singly or in groups within space called lacunae in the extracellular matrix, it is typically a large cells often exceeding 40 µm in diameter. A membrane of dense irregular connective tissue called the perichondrium covers the surface of most cartilage. Unlike other connective tissue, cartilage has no blood vessels or nerves, except in the perichondrium therefore cartilage cells received their nutrition by diffusion from the vessels in the perichondrium. Since cartilage has no blood supply (avascular tissue), it heals poorly following an injury. Development of Cartilage Cartilage is deriving (embryologically) from mesenchyme. Some mesenchymal cells differentiate into cartilage forming cells (chondroblasts) which produce the intercellular matrix as well as collagen fibers that form the intercellular substance of cartilage. Chondroblasts that become imprison within this matrix become chondrocytes. Some mesenchymal cells that surround the developing cartilage form the perichondrium. Depending on the number and variety of fibers that embedded in the matrix, the cartilages classified to:1- Hyaline cartilage (hyalos=glass):This type of cartilage is bluesh/wihte in the fresh state and is the most prevalent form contains a resilient homogenous ground substance. Many collagen fibers are embedding in the matrix, and prominent chondrocytes found in the spaces called lacunae. Toward the center of a mass of hyaline cartilage, the cells are large and are usually present in groups of two, four or more called cell-nests (isogenous group). Division of a single parent cell forms these groups. Toward the periphery of the cartilage, the cells are Dr. Abdulla ------------------------------------Histology----------------------------2ststage 2 smaller. Most hyaline cartilage is surrounding by perichondrium. The matrix consists of chondromucoprotein (polymer of mucoprotein with chondroitin-4-sulfate and chondroitin-6-sulfate these components gave the matrix acidophilic, therefore react with basophilic substances as haematoxyline and eosin stains gave blue (fig.1). Fig1: Hyaline cartilage showing matrix in which (Ch) chondrocytes localized within (L) lacuna; that surrounded by (Cap) Capsule; and perichondrium (P) at the periphery. Distribution of hyaline cartilage Hyaline cartilage is widely distributed in the body as follow:1- Costal cartilage: - there are bars of hyaline cartilage that connect with the sternum. 2- Articular Cartilages: - the articular surfaces of most synovial joints lined by hyaline cartilage (which is not covered by perichondrium kept moist by synovial fluid which also provides nutrition to them). 3- Larynx: - thyroid cartilage, the cricoid cartilage, and the arytenoid cartilage. 4- Tracheal and bronchial rings. 5- Nose and nasal septum. 6- Embryonic and fetal skeleton. 2- Fibrocartilage Chondrocytes of this type of cartilage are scattered among clearly visible bundles of collagen fibers within the extracellular matrix. Fibrocartilage lacks a perichondrium, combines strength and rigidity, and is the strongest of the three types of cartilage. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 3 Distribution of Fibrocartilage cartilage Fibrocartilage is most conspicuous in:1- Secondary cartilaginous joints or symphysis (symphyses) like pubic symphysis, and intervertebral discs. 2- Articular surfaces of synovial joints formed by membrane bones (mandible, clavicle). 3- Articular discs: - (menisci, temporomandibular joint, and sternoclavicular joint. 4- Insertion of tendons into cartilages and it is run into groove which lined by fibrocartilage. 3- Elastic cartilage In this tissue, chondrocytes are located within a threadlike network of elastic fibers within the extracellular matrix. A perichondrium is present. Elastic cartilage possesses greater flexibility than hyaline cartilage and maintains the shape of certain structures. Distribution of elastic cartilage The sites where elastic cartilage is found are as follow:1- It form the skeletal basis of the auricle (pinna or external ear) Dr. Abdulla ------------------------------------Histology----------------------------2ststage 4 2- The wall of the medial part of the auditory tube. 3- In the laryngeal cartilages (the epiglottis and the apical part of arytenoid cartilage). If we examination a longitudinal section across a long bone (such as the thigh) we see that the wall of the shaft is tubular and encloses a large marrow cavity. In naked eye examination, the wall of the tube made up of a hard dense material this type of bone called (compact bone). The marrow cavity does not extend to bone ends. They are filling by a meshwork of tiny rods or plates of bone and contain numerous spaces this appearance like sponge this type of bone called (spongy bone). The entire outer surface of bone is covering by a membrane called (periosteum) except the bone ends which play a part in forming joints they are covering by a layer of articular cartilage. A membrane called (endosteum) lines the wall of the marrow cavity. The marrow cavity and the spaces of the spongy bone are filling by a vascular tissue called bone marrow. At the bone ends, the marrow is red in color that contains numerous masses of blood forming cells (haemopoitic tissue) and blood cells at various stages of formation. In the shaft of bone of an adult the marrow is yellow, which is made up of predominantly of fat cells some is land of haemopoitic tissue may be seen here also. The entire bone marrow is red in bones of a fetus or young children. Function of bone: 1- Bone supports soft tissues. 2- Bone protects vital organs. 3- House red bone marrow, which produces blood cells. Moreover, contain yellow bone marrow a storage site for triglyceride. 4- Calcium and phosphorus storehouse. Bone is a rigid form of connective tissue composed of cells embedded in an intracellular matrix of collagen Dr. Abdulla ------------------------------------Histology----------------------------2ststage 5 fibers, glycosaminoglycans and calcium phosphate deposited as hydroxyapatite. Bone is a living tissue supplied with blood vessels and nerves. Bone cells There are three types of cells: 1- Osteocytes: - The mature bone cells only one osteocytes found in each lacuna. Flat almond shape, irregular nuclei, eosinophilic or lightly basophilic cytoplasm. Delicate cytoplasmic processes arising from it occupy canaliculi. 2- Osteoblasts: - The bone forming cells, located at the surfaces of bone tissue are varying shapes, ovoid nuclei, basophilic cytoplasm, cytoplasmic processes arising from each cell contact with adjacent cells. 3- Osteoclasts: - The bone removing cells, they multinucleated giant cells (100 µm), they have numerous nuclei (up to 20 or more). Bone types 1- Compact bone:- it is made of layers or lamellae that a thin plate of bone consisting of collagen fibers and minerals salts that are depositing in a gelatinous ground substance, these lamellae placed over one another leave small spaces between adjoining lamellae called (lacunae), which lying the osteocytes. From each lacunae here spreading out fine canals (canaliculi) that communicate with other lacunae. Delicate cytoplasmic processes arising from osteocytes occupy these canals. Collagen fibers of one lamellus arranged parallel to each other, but those of adjoining lamellae run at varying angles to each other. Most of the lamellae are arrange in the form of concentric rings that surround a narrow canal called (Haversian canal) that occupied by blood vessels, nerves and some cells. One Haversian canal and the lamellae around it constitute a (Haversian system or osteon). Haversian canal run along the length of the bone, branched, and anastomoses with each other. They also communicate with marrow cavity and with external surface through channels that called (Volkmann canales). Blood vessels and nerves pass through all these channels. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 6 Spongy bone (cancellous bone):- the bone plates or rods that form the meshwork of spongy bone called (trabeculae). Each trabeculus made up of a number of lamellae. Between lamellae there is lacunae which contain osteocytes also these lacunae spreading the canaliculi which containing the processes of osteocytes. The trabeculae enclose wide spaces which are filled in by bone marrow they received the nutrition from the blood vessels in the bone marrow. Bone Matrix The ground substance (matrix) of bone consists of the follow:1- Organic matrix contains proteins and mucopolysaccharides. 2- Inorganic ions present are predominantly calcium and phosphorus. Magnesium, carbonate, hydroxyl, chloride, fluoride, and citrate ions are also present in significant amounts. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 7 Periosteum 1- The outer layer is a fibrous membrane. 2- The inner layer is cellular (fibroblasts or osteogenetic in young bone and osteogenic in adult bone) Endosteum It is lines marrow cavity within the bone and composed of a single layer of flattened osteogenic cells and a very small amount of connective tissue. Functions of periosteum: 1- Provide muscles, tendons, and ligaments attachments. 2- The periosteum performs a nutritive function because of the blood vessels passing from periosteum into bone. 3- The periostium can form bone when required by cellular layer. Bone repair in fracture Ossification (Bone formation) All bone is of mesodermal origin. There are two kinds of bone formation 1- Intramembranous ossification. Firs stage: - Membrane formation a-The mesenchymal cells become densely (Mesenchymal condensation). b- The region becomes vascular. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 8 c- Some of mesenchymal cells lay down bundles of collagen fibers in the mesenchymal condensation. Second stage: osteoid formation Some of mesenchymal cells become osteoblasts (enlarged and acquire a basophilic cytoplasm) they lei along the bundles of collagen fibers, then secrete a gelatinous matrix in which the fibers embedded this swollen fibers and matrix called osteoid. Third stage: First lamellus formation Under osteoblasts calcium salts deposited in the osteoid as soon as called lamellus. Fourth stage: second lamellus formation Over the first lamellus, another layer of osteoid laid down by the osteoblasts that move away from the first lamellus to line the new layer of osteoid. Some of osteoblasts caught between the lamellus and the osteoid. The cell trapped between the two lamellae become osteocytes. Fifth stage: trabeculus formation A number of lamellae laid down one over another and they together form a trabeculus of bone. In this way, typical spongy bone will be form that converted into compact bone. 2- Endochondral ossification Firs stage: - hyaline cartilage formation (cartilaginous model) 1- The mesenchymal cells become densely (Mesenchymal condensation). 2- Some of mesenchymal cells become chondroblasts and lay down hyaline cartilage. 3- Some of mesenchymal cells on the surface of the cartilage form a membrane called perichondrium vascular and contain osteogenic cells. 4- The cells of the cartilage at first small and irregularly arranged. They begin enlarge. Second stage: - primary areolae formation 1- The intercellular substance between the enlarged cells becomes calcify, under the influence of enzyme called alkaline phosphatase, which secreted by the cartilage cells. Then the nutrition to the cells thus cut off and they die leaving behind empty spaces called primary areolae. 2- Perichondrium called periostium as soon as bone formation. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 9 Third stage: - secondary areolae formation 1- Blood vessels and osteogenic cells now invade the calcified cartilaginous matrix this mass of vessels and cells called (periosteal bud). 2- Periosteal bud eat away much of calcified matrix forming the wall of the primary areolae and thus creates large cavities called secondary areolae. 3- The walls of secondary areolae formed by thin layers of calcified matrix (plates) the osteogenic cells become osteoblasts and arrange themselves along the surfaces of these plates. Fourth stage: - osteoid formation 1- The osteoblasts lay down a layer of (osteoid). 2- The osteoblasts lay down another layer of osteoid over the first lamellus. 3- The osteoblasts that caught between the two lamellae form osteocytes, more lamellae lay down then bony trabeculae formed. Then typical spongy bone will be form that converted into compact bone. Fig1: Histogenesis of hyaline cartilage. A: The mesenchyme is the precursor tissue of all types of cartilage. B: Mitotic proliferation of mesenchymal cells gives rise to a highly cellular tissue. C: Chondroblasts are separated from one another by the formation of a great amount of matrix. D: Multiplication of cartilage cells Conversion spongy bone to Compact bone All newly formed bone is spongy. It is converting into a compact bone as follow: 1- Primary osteons (atypical Haversian system). Each space between trabeculae of spongy bone comes to be line by a layer of osteoblasts that lay down lamellae of bone. Subsequently concentric lamellae lay Dr. Abdulla ------------------------------------Histology----------------------------2ststage 10 down inside this ring thus forming a haversian system or osteon the original space becomes smaller and form a haversian canal. 2- Secondary osteons (typical haversian systems). The primary osteons do not have a typical lamellar structure and chemical composition. They are invading by blood vessels and by osteoblasts, which bore a new series of spaces through them, these new spaces filled in by new bony lamellae to form secondary osteon. Development of a typical long bone Hyaline cartilage formation (cartilaginous model) 1- Endochondral ossification starts in the central part of the cartilaginous model this area called primary center which ossification gradually toward ends of shaft. 2- Perichondrium now called periostium and the osteogenic cells of it lay down bone on the surface of the cartilaginous model by intramembranous ossification. 3- At about the time of birth the developing of bone consist of a- Diaphysis (shaft) formed by primary center ossification. b- Epiphysis (ends) formed by secondary center ossification. c- Epiphyseal plate is separating the bone of the epiphysis and the bone diaphysis this play a vital role in the growth of the bone. Growth of a long Bone A growing bone increase in both length and girth directions. 1- Osteogenic cells of periostium lay down layers of bone on the surface of the cartilaginous model by intramembranous ossification. 2- When bone lay down layer of bone outside, osteoclasts remove layer of bone from inside. Then the bone growth in diameter and its wall does not become too thick. 3- Trabeculae of bone in the center removed also that formed by endochondral ossification, in this way a marrow cavity is form and extend toward the end of the diaphysis but not reach to epiphyseal plate. Metaphysis Dr. Abdulla ------------------------------------Histology----------------------------2ststage 11 The portion of the diaphysis adjoining the epiphyseal plate called metaphysis. Characteristic by:1- Active portion of bone formation, for this reason, it is high vascular. 2- Dose not have marrow cavity. 3- Muscles and ligaments usually are attachment sites. 4- Act as a storehouse of calcium. 5- It is frequently the site of infection. Blood supply of bone 1- Nutrient artery Pierced the shaft at nutrient foramen and enter the marrow cavity the divided into ascending and descending branches. 2- Epiphyseal arteries. 3- Metaphyseal arteries. 4- Periosteal arteries: - which small arteries arise from periosteal vessels and enter the bone through minute foramina then reach the haversian canals through the Volkmann canals. 5- The marrow cavity contains a large central venous sinus is drained by numerous veins which accompany the arteries. 6- Lymphatic vessels are present in periostium, but not in bone substance. 7- Nerve accompany the blood vessels into the marrow cavity and into haversian canals, they are most numerous near joints. BONE Marrow (Myeloid or myelogenous haemopoitic tissue): Is the primary site for the production of all blood cells in the adult (Hemopoiesis). All bone marrow begins as Red marrow, also called Active, or Hematogenous marrow. During growth, the blood cells of this active hematopoietic tissue are gradually depleted and replaced by adipocytes. In adult, red marrow is restricted to the skull vertebrae, ribs, sternum, and the proximal epiphyses of some long bones. The fatty, non hematopoietic replacement tissue found in other bony cavities is termed yellow marrow. Dr. Abdulla ------------------------------------Histology----------------------------2ststage 12 Histology of Red marrow: 1- A dipocytes (from up to 75%). 2- Macrophages. 3- Reticular cells and reticular fibers. 4- Hematopoietic stem cells. Hemopoiesis (blood cell production) It is includes both the proliferation and the differentiation of hematopoietic stem cells. May be subdivided according to the cell type: a. Erythropoiesis . b. Leucopoiesis. c. Granulopoiesis d. Agranulopoiesis e. Lymphopoiesis f. Thrombopoiesis (platelet formation). Regulation of hematopoiesis : Involves specific colony stimulating factors ( CSFs) . a- Erythropoietin. b- Leucopoiesis. c- Thrombopoietin