Biventricular
pacemaker/
implantable
cardiac
defibrillator
Patient discharge
instructions
If you have questions or concerns regarding your
device, please contact your doctor. Someone should be
available from your doctor’s office 24 hours a day, 7 days
a week. Use this space to write down your doctor’s name
and phone number.
In any emergency, always call 911.
My doctor: ___________________________________
Phone number: _______________________________
If you cannot reach your doctor, call us at 617-667-8800
for further instructions. You may call 24 hours a day, 7
days a week.
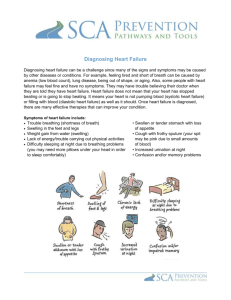
In some people with heart
failure, the two lower chambers
of the heart, called the
ventricles, are not beating at the same time. When this happens, the heart is less able to pump
blood to the body effectively.
The biventricular pacemaker delivers small electrical impulses that coordinate the beating of
the right and left ventricles. This helps the heart to
pump blood more efficiently so that symptoms of
Important information for patients
heart failure may occur less frequently. This is
with heart failure
called cardiac resynchronization therapy.
Within the pacemaker, there is an implantable
cardioverter/ defibrillator (ICD). This component
of the pacemaker is programmed to detect lifethreatening, abnormal heart rhythms. When
detected, the device delivers a jolt of electricity to
restore regular heart rhythm.
Heart failure is a condition that reduces the
heart’s ability to pump blood. Because of heart
failure, the heart cannot pump enough blood to
supply the body’s need for oxygen. As a result,
fluid may build up and you may experience
shortness of breath, swelling of the feet and
legs, and weight gain.
As a patient with heart failure, you should:
This sheet contains important instructions
regarding your device. If you have any questions,
please be sure to ask your doctor or nurse.
How should I take care of my
incision?
The following are general instructions for taking
care of the incision. In some situations, your
doctor may provide you with more detailed
instructions.
You should keep the dressing on for 72 hours.
You may take a tub bath or sponge bath during
weigh yourself every morning
follow a low-salt diet (2 grams of sodium or
less per day)
take medication as prescribed
You should call your doctor or nurse if you
notice:
weight gain of three pounds or more in two
days, or five pounds or more in five days
worsening shortness of breath
swelling of the feet or legs
dry, hacking cough
1
this time, as long as the dressing does not get wet.
After 72 hours, you may remove the outside dressing and shower. Please do not allow water to spray directly
onto the incision and do not rub soap in the area of the incision.
Over
Please do not remove the small paper strips (steri-strips) that are directly on your skin. They will fall off on their
own. (This may take several weeks.)
You might have slight itching at the incision. Try not to scratch the incision or rub it.
Do not apply lotion or powder to the incision.
Bruising into the upper arm may be seen.
Let your doctor know right away if you note any of the following:
redness, swelling, or drainage at or near your incision
temperature of 101 or more (fever)
pain that is getting worse instead of better
any opening at the site of the device
May I go back to my usual activities?
Please follow these guidelines regarding activity. Ask questions about any other activities you aren’t sure about.
You may be asked not to drive for a certain amount of time during your recovery. This is different for everyone.
Please ask your doctor when you may drive.
For six weeks, don’t lift, carry, push, or pull anything weighing more than five pounds using the arm on the side
where the device was device was inserted.
During the first six-eight weeks, you will need to watch how you use the arm on the side where your device was
inserted. You may wash your face, brush your teeth, shave, and comb your hair. Do not raise your elbow above
the height of your shoulder. You may not swim or play tennis or golf.. This is a good time to ask for help with
things like raking leaves, cleaning, painting, ironing, vacuuming, or walking a dog.
What medicines should I take?
Before you leave the hospital, you will be given a list of all the medicines you should take once you are at
home. Please be sure to ask any questions you have about medicines. If something you normally take is not
on the list, please ask whether you should continue taking it. This includes prescription medicines,
nonprescription medicines, vitamins, herbs, and supplements.
You may be given a prescription for antibiotics to take for a short time when you get home.
2
If needed, you may take acetaminophen (Tylenol) every six hours as needed for discomfort. (Never take more
than 4 grams, or 4,000 milligrams, of acetaminophen in 24 hours.) If your discomfort is severe or is not relieved
by acetaminophen, please call your doctor.
Use of electronic and other equipment
Electrical items in your home that are in good condition should not interfere with your pacemaker. This includes
things like microwaves, TV remotes, electric blankets, food processors, hair dryers, shavers, or vacuum cleaners.
There is a small chance that putting your cellular phone too close to your pacemaker could cause temporary
interference with the functioning of your pacemaker. To reduce the chance of any problem:
Hold the phone to the ear on the opposite side of your body from the pacemaker.
Keep the phone at least six inches away from the pacemaker.
When carrying the phone in a pocket or on a belt, store it on the opposite side from your pacemaker,
being sure it is at least six inches away from the device.
A security system (a gate, archway, or total body scanner) at an airport, government building, or other location
will likely detect your pacemaker as a metal object. Before going through the system, show your ID card to the
security personnel. When moving through a security gate or archway, walk through the system at a normal pace
– do not linger or walk slowly. This will decrease the chance that the system will interfere with your device. If
you feel symptoms, such as a rapid heartbeat or dizziness, move away from the device. If you are being screened
with a hand-held wand, ask the security personnel to avoid putting the wand directly over your device for a
prolonged period. If you are being screened using a body scanner, you may enter the scanner in the normal
fashion and follow the instructions you are given.
Anti-theft gates at retail stores are not likely to cause a problem if you walk through them at normal speed and do
not linger near the anti-theft device.
When using power tools, keep a six-inch distance between the tool’s motor and your pacemaker. For gasolinepowered devices, such as a lawn mower, snow blower, leaf blower, etc., keep 12 inches between the ignition
system of the device and your pacemaker.
Do not carry magnets, or any products containing magnets, close to your device.
Chain saws or welding equipment are more likely to interfere with your pacemaker than other electronic devices.
Please do not use this equipment.
Additional cautions may apply if you are using high-powered industrial or commercial tools. If this applies to
you, please ask your doctor for more information.
What happens if I get a shock from the ICD that is part of my pacemaker?
Most patients feel the ICD if it gives a shock. Fortunately, it is very quick, but it can be uncomfortable. Some people
say it feels like being kicked in the chest, but it lasts less than a second. You will want to inform your doctor if your
device gives you a shock. If there is more than one shock or if you have symptoms, you need immediate attention.
Please follow these guidelines when deciding what kind of help you need.
3
If you get a shock but don’t have any symptoms such as dizziness, palpitations, chest pain, shortness of breath,
or fatigue, you should call the doctor who put in your device right away to report the shock.
If you get a shock and feel poorly in any way, or if you get more than one shock, you should call 911 and go to
the emergency room.
Over
Other important information
Always tell any doctor, dentist, or other health care provider who treats you that you have a pacemaker/ICD.
Because of your pacemaker, you should never have an MRI (magnetic resonance imaging) to any part of your
body. MRI is a special test that uses a magnet to look inside the body. Exposure to the MRI magnet can ruin the
pacemaker, causing it to malfunction.
A pacemaker/defibrillator identification card will be mailed to your home in the coming weeks. You should
carry it with you at all times.
You should also carry a list of your medications, a brief summary of your medical history, a list of any allergies,
and your doctors’ phone numbers.
You may wish to purchase a medical identification bracelet or necklace that informs anyone caring for you that
you have a pacemaker.
Follow-up appointments
Prior to your discharge home, you will be given information about your follow-up appointments. Be sure to ask any
questions you may have about your appointments.
Call for help if:
Call for help if you have:
redness, swelling, drainage, or any opening at the area of your incision
temperature of 101 or more
pain from the incision that is getting worse instead of better
a shock from your device (call 911 if you get more than one shock or have symptoms along with the shock)
swelling of the feet or legs
weight gain three pounds or more in two days, or five pounds or more in five days
worsening shortness of breath
dry, hacking cough
a return of symptoms you had before your pacemaker insertion or any other symptom that concerns you
Note: You underwent a procedure performed under fluoroscopic (x-ray) guidance. Fluoroscopy is a type of medical imaging that shows a series of xray images on a monitor, much like an x-ray movie. The amount of radiation used depended on many factors, including your body size and the level
of complexity encountered during the procedure. Procedures involving a greater amount of radiation may result in some changes to the skin.
Although most patients do not develop any problems, we want to remind you that this procedure may cause injury to the exposed skin and hair. These
effects may be increased if you have had previous radiation exposure to the same skin area, particularly within the past 12 months. Radiation injury
4
to the area of exposed skin can take many forms, including redness, blistering, loss of the hair over the skin, and breakdown of skin. These effects can
appear after a few weeks or even after several months. Please remind your primary care provider to examine your skin periodically over the next 12
months for evidence of radiation injury, as skin changes may not appear immediately. If at any time you notice changes to your skin, please contact
us 617-667-8800 to arrange further evaluation.
This material was prepared by clinicians from the CardioVascular Institute at Beth Israel Deaconess Medical Center. It is produced and distributed by The Beth Israel
Deaconess Learning Center. ©2010, Beth Israel Deaconess Medical Center. All rights reserved. MC1581Rev. 12/10
5