Laryngology Seminar
advertisement

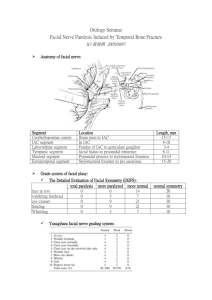
Otology Seminar Management of Complications from Temporal Bone Fractures R3 郭士偉 2006/06/27 Classification of Temporal Bone Fractures traditional classification (1946): originally based on simulated impact studies on cadaver skulls. Longitudinal and transverse at frequencies of approximately 80% and 20%, respectively. Ghorayeb and Yeakley (1992): CT findings of 150 temporal bone fractures, 75%- oblique, 12%- transverse, 3%- longitudinal, and 9%- mixed. (oblique fractures lie in a horizontal plane and cross the petrotympanic fissure, whereas longitudinal fractures run in a vertical plane and lie within the petrotympanic fissure.) Yanagihara et al. (1997): type 1- mastoid process; type 2- EAC; type 3pyramidal and horizontal portion of facial nerve; type 4- geniculate ganglion, labyrinthine and horizontal segment of facial nerve (figure) Kelly and Tami (1994)- “otic capsule sparing” and “otic capsule violating” (CSF fistula, severe SNHL, facial paralysis) Stacey (2004): petrous fracture (FN injury and CSF leak) and nonpetrous fractures (middle ear- CHL, mastoid) Statistic Datas Management of Complications 1. Cerebrospinal fluid leak clear otorrhea or rhinorrhea noted on clinical examination Diagnosis: acute posttraumatic CSF fistula: high probability of early spontaneous closure and a low incidence of meningitis can be treat conservatively for 7-10 days total bedrest with elevation of head of the bed; stool softners; instructions to avoid nasal blowing, sneezing, and straining; repeat lumbar punctures or lumbar drain if the leak persists CSF fistulae persisting for > 7 days resulted in a significantly increased risk of meningitis Incidental adequate prophylactic antibiotics was defined as 5 days of treatment within the first week of CSF leakage, or for the duration of the CSF fistula for leaks that lasted for < 1 week. Antibiotic coverage for < 5 days during the first week of leakage was classified as inadequate prophylaxis most common infecting organisms in meningitis occurring in the presence of a CSF fistula: Pneumococcus, Streptococcus, and Hemophilus influenza. Positive cultures in our series most commonly demonstrated E. coli and Pseudomonas closure of fistulae persisting > 7–10 days is recommended. approach chosen to close a CSF fistula: (a) the status of hearing in the affected and contralateral ear; (b) the presence of brain herniation through the tegmen; (c) the status of the ear canal; and (d) location of the fistula. In a patient with a fracture of the otic capsule resulting in profound sensorineural hearing loss, obliteration of the mastoid and middle ear is recommended. (The ear canal, tympanic membrane, incus and malleus, and middle ear mucosa are all excised. The external auditory meatus is closed in a two layer closure and a complete mastoidectomy is performed. The mucosa of the Eustachian tube is inverted, and a muscle plug is inserted. The incus is then inserted as well, wedging the muscle into place. The Eustachian tube and fracture line are covered by temporalis fascia, and the mastoid cavity and middle ear are obliterated with an abdominal fat graft. only hearing ear ipsilateral to the CSF fistula: A complete mastoidectomy is performed and the site of leakage is identified. A. If the fistula is in the region of the tegmen mastoideum or into the posterior cranial fossa, fascia is placed over the leak and the antrum and the mastoid cavity obliterated. B. if the leak passes through the tegmen tympani a mini-middle fossa craniotomy approach is utilized in order to avoid injury or interference with the function of the ossicular chain. A pedicled temporalis fascia flap is rotated into the middle fossa and placed over the defect in the tegmen tympani. temporal lobe herniates through the tegmen: the damaged brain is debrided via the transmastoid approach and the remaining brain and dura are elevated back up into the middle fossa by way of the middle fossa craniotomy. Temporalis fascia flap is used to cover the dural defect using an extradural approach. The window of bone harvested with the middle cranial fossa craniotomy is then inserted along the floor of the middle fossa in order to cover the defect and prevent subsequent prolapse. Additional fascia is placed along the tegmen from the undersurface and across the antrum. The mastoid cavity is then obliterated with fat. Gunshot wounds to the temporal bone: high risk of external auditory canal stenosis and cholesteatoma formation. In this situation, the CSF fistulae are generally closed with resection of the external auditory canal and tympanic membrane and obliteration of the mastoid and middle ear. (avoid leaving any fragments of epithelium which may subsequently lead to cholesteatoma formation). All mucosa is removed and the Eustachian tube and external meatus are closed 2. Facial nerve palsy Delayed onset group: which ranged from 1 to 16 days, was defined as normal function at the time of admission, followed by diminished or absent function on any subsequent exam. The incidence of complete paralysis was greater in the immediate onset group compared with the delayed onset group. Fisch: the degeneration on electroneuronography (ENOG) reaches 90% within 6 days of onset of palsy poorer outcome and consequently should be decompressed. delay of onset of paralysis following temporal bone fracture is an important predictive factor. Complete spontaneous recovery: 94% severity of paresis is also an important criteria in the management of facial nerve. Incomplete paresis rarely fails to resolve spontaneously unless an additional insult to the nerve occurs such as infection. The rate of good recovery of facial function following decompression was 55%. Exploration in patients with complete immediate onset paralysis The site of injury to the facial nerve in temporal bone fractures is in the perigeniculate region in 80–93% of patients Fisch advocates a translabyrinthine approach for transverse fractures and a combined transmastoid/middle cranial fossa approach for longitudinal fractures. May described a transmastoid/supralabyrinthine approach to the region of the geniculate ganglion for facial nerve decompression. Yanagihara: type 1 & 2: transmastoid approach (distal half of the horizontal segment and the stylomastoid foramen); type 3 or 4: transmastoid/supralabyrinthine approach +\- middle cranial fossa approach Timing of facial nerve repair is also controversial. McCabe advocated repairing the nerve within the first 3 days or delaying facial nerve reanastomosis for 20 days postinjury. (regeneration and axoplasmic flow were greatest at 3 weeks postinjury) Barrs studied the timing of facial nerve repair in micropigs and found no advantage of waiting the three weeks until the neuronal cell body metabolic activity was maximal. Fisch advocates exploration when the ENOG indicates 90% degeneration occurring within 6 days. He argues that decompression should be performed early to minimize further degeneration; May also advocates early exploration. ANTONIO: in patients unable to be operated on early, who present 1–3 months after TBF with >95% denervation on EnoG, FN decompression can still have a beneficial effect. 3. Hearing loss Twenty-one percent of the ears with documented hearing loss had a conductive loss, 57% had a sensorineural loss, and the remaining 22% had a mixed loss Conductive HL: spontaneous resolution, ossicular reconstructions SNHL: longitudinal fractures were three times more likely than transverse fractures to be associated with SNHL Bil. Profound SNHL: cochlear implant any fracture through the otic capsule can lead to complete loss of auditory and vestibular function. Even after severe injury, adequate numbers of spiral ganglion cells appear to exist for successful cochlear implantation Labyrinthitis ossificans: most frequent site of ossification appears to be the basal turn of the scala tympani 1. inserted into scala vestibuli; 2. drilling out the obliterated portion of the basal turn; 3. partial labyrinthectomy has been proposed to gain access to the round window facial nerve stimulation: explanted and have the contralateral ear implanted preoperative CT scan; Preoperative promontory stimulation testing High-resolution T2 sequences on MRI may be a more sensitive method for determining patency of the cochlea. A 25-year-old male, bil. Transverse temporal bone fracture (otic capsule violating) References 1. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol 1997;18(2):188-97. 2. Camilleri AE, Toner JG, Howarth KL, Hampton S, Ramsden RT. Cochlear implantation following temporal bone fracture. J Laryngol Otol 1999;113(5):454-7. 3. Darrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C, Bebear JP. Management of facial paralysis resulting from temporal bone fractures: Our experience in 115 cases. Otolaryngol Head Neck Surg 2001;125(1):77-84. 4. Ishman SL, Friedland DR. Temporal bone fractures: traditional classification and clinical relevance. Laryngoscope 2004;114(10):1734-41. 5. Levine SC. A complex case of cochlear implant electrode placement. Am J Otol 1989;10(6):477-80. 6. Quaranta A, Campobasso G, Piazza F, Quaranta N, Salonna I. Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Acta Otolaryngol 2001;121(5):652-5. 7. Simons JP, Whitaker ME, Hirsch BE. Cochlear implantation in a patient with bilateral temporal bone fractures. Otolaryngol Head Neck Surg 2005;132(5):809-11. 8. Steenerson RL, Gary LB, Wynens MS. Scala vestibuli cochlear implantation for labyrinthine ossification. Am J Otol 1990;11(5):360-3. 9. Yanagihara N, Murakami S, Nishihara S. Temporal bone fractures inducing facial nerve paralysis: a new classification and its clinical significance. Ear Nose Throat J 1997;76(2):79-80, 83-6