The influence of prison-based methadone maintenance treatment
advertisement
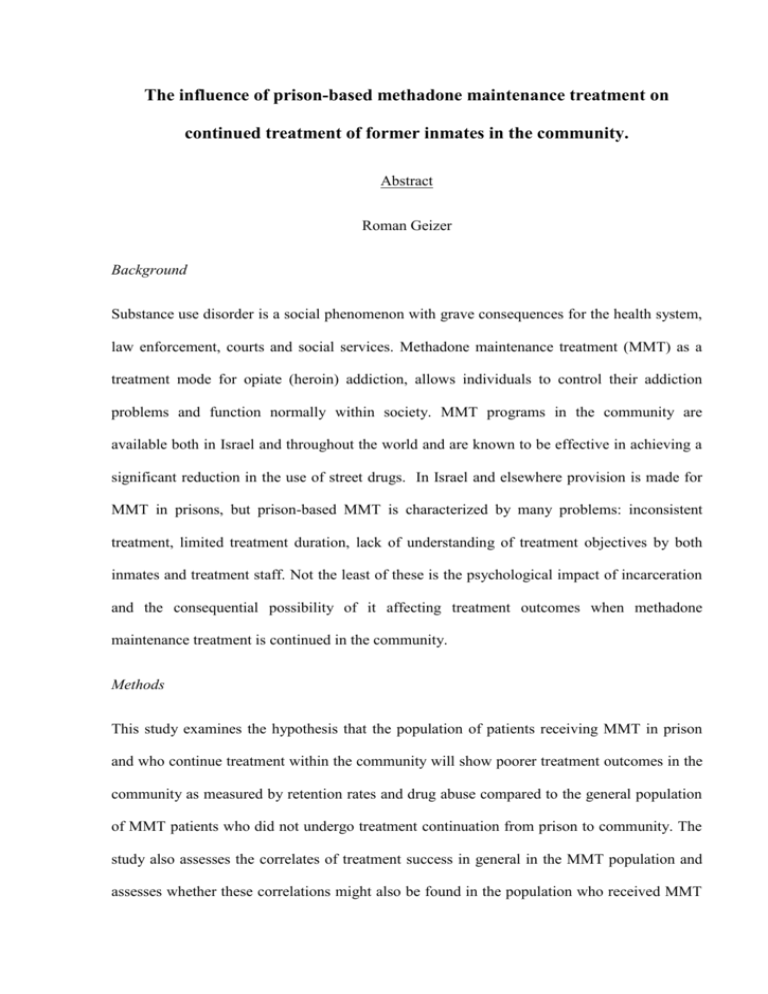
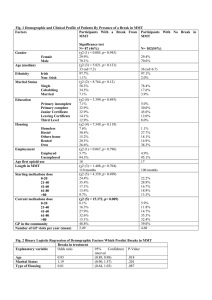
The influence of prison-based methadone maintenance treatment on continued treatment of former inmates in the community. Abstract Roman Geizer Background Substance use disorder is a social phenomenon with grave consequences for the health system, law enforcement, courts and social services. Methadone maintenance treatment (MMT) as a treatment mode for opiate (heroin) addiction, allows individuals to control their addiction problems and function normally within society. MMT programs in the community are available both in Israel and throughout the world and are known to be effective in achieving a significant reduction in the use of street drugs. In Israel and elsewhere provision is made for MMT in prisons, but prison-based MMT is characterized by many problems: inconsistent treatment, limited treatment duration, lack of understanding of treatment objectives by both inmates and treatment staff. Not the least of these is the psychological impact of incarceration and the consequential possibility of it affecting treatment outcomes when methadone maintenance treatment is continued in the community. Methods This study examines the hypothesis that the population of patients receiving MMT in prison and who continue treatment within the community will show poorer treatment outcomes in the community as measured by retention rates and drug abuse compared to the general population of MMT patients who did not undergo treatment continuation from prison to community. The study also assesses the correlates of treatment success in general in the MMT population and assesses whether these correlations might also be found in the population who received MMT in prison. Cross-sectional retrospective research design is employed to facilitate comparison between the former prison population sample and the general sample of patients. The samples cover 542 patients accepted at the Methadone Community Center in Jerusalem during the years 1991-2007. Data used in relation to randomized urine screening tests for street drugs, two-year retention rates and demographics were obtained from the Center’s database. Results Patients who received continued MMT treatment from prison to community spent on average fewer days in treatment and used more cocaine during the first year of treatment compared to the patients that did not receive MMT in prison. No differences between the groups were found as to the use of opiates, benzodiazepines and the pattern of use of any kind of illicit drugs over the 2 years period. A small number of demographic factors were found to be correlated to treatment outcomes, although none of them were distinctive features of the former prison inmates group. Conclusions Prison-based MMT is a risk factor for the continuation of MMT treatment in community. It can affect negatively treatment tenure in general and abstinence from cocaine during the first year of treatment. Possible explanations are the long-term implication of deficient and inadequate methadone treatment in prison along with the psychological impact of incarceration and institutionalization to the prison environment. The Clinical implication are that MMT programs should consider the former prison inmates population that received MMT in prison to be at a high risk for dropping out of treatment. Therefore, increased treatment input and psychological interventions specifically designed for the needs of this group may reduce dropout. The influence of prison-based methadone maintenance treatment on continued treatment of former inmates in the community. By: Roman Geizer Supervised by: Dr. Marc Gelkopf THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE MASTER DEGREE University of Haifa Faculty of Social Welfare and Health Sciences Department of Community Mental Health October, 2009 The influence of prison-based methadone maintenance treatment on continued treatment of former inmates in the community. Roman Geizer THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE MASTER DEGREE University of Haifa Faculty of Social Welfare and Health Sciences Department of Community Mental Health October, 2009