Nuclear Medicine Procedures at Christchurch Hospital
advertisement

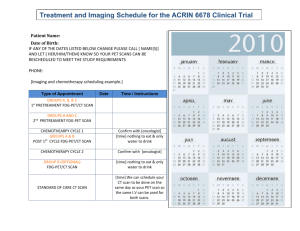
NUCLEAR MEDICINE DEPARTMENT AT CHRISTCHURCH HOSPITAL Information for Medical Practitioners & Nursing Staff For hospital staff with access to the CDHB Intranet, the following Information can be found in the CDHB Policy & Procedure Manual Volume 14: Radiology and Nuclear Medicine Procedures Performed at Christchurch Hospital. Nuclear Medicine Procedures at Christchurch Hospital Name Authoriser Date General Information - Nuclear Medicine EDON 20 March 2012 Imaging Procedures EDON 20 March 2012 1 General Information 1.1 Introduction ....................................................................................................... 1 1.2 Imaging ............................................................................................................. 1 1.3 Process of Initiating a Nuclear Medicine Scan.................................................. 2 1.4 Reports ............................................................................................................... 3 1.5 Radiation Dose .................................................................................................. 3 1.6 The "Nuclear Medicine Study" Notice .............................................................. 4 1.7 Accompanying Staff and General Nursing Care ............................................... 4 1.8 Body Fluids ........................................................................................................ 5 1.9 Patient Preparation ............................................................................................. 5 1.10 Patient Information .......................................................................................... 6 1.11 Examination of Pregnant and Breastfeeding Women ..................................... 7 1.12 Adverse Reactions ........................................................................................... 7 1.1 Introduction Nuclear Medicine is a branch of medicine that uses radioactivity for diagnosis or therapy. Unlike x-rays, CT and MRI scans that give structural information, Nuclear Medicine imaging demonstrates the function of an organ or organ system by monitoring the passage, accumulation or excretion of a radiopharmaceutical. Because injuries or disease processes tend to affect the function of an organ before the structure is altered, Nuclear Medicine plays an essential role in helping with the early diagnosis of a wide variety of diseases and conditions, which in turn can make treatment more timely and effective. 1.2 Imaging Nuclear Medicine Imaging procedures are often referred to as “scans,”scintigraphy, “isotope studies or “radionuclide imaging. To perform a nuclear medicine scan, a radioactive pharmaceutical is first administered to the patient, usually intravenously. Depending on the type of scan, the pictures may be taken immediately and/or after a period of time during which the pharmaceutical localises in the target organ/system. The patient is asked to lie still on an imaging bed. The gamma camera or SPECT/CT camera is positioned above and below the area/s of interest. The camera detects the gamma rays that are emitted from the patient’s body. Images are obtained of the distribution within the body over a period of time. The scan may take between 10 and 120 minutes, depending on the type of study. The patient is required to lie still for the duration of the scan. It is not necessary for the patient to fully undress however traction slings may need to be removed. Different types of images can be acquired: A Static image is one picture taken over a set time period. Dynamic images are lots of continuous pictures which can be played back like a movie and used to measure the clearance of a radiopharmaceutical from the organ of interest. The camera remains set in one position for these scans. For a whole body scan, the imaging bed moves the patient past the detectors, imaging from head to toe. For tomography (SPECT) the detectors move round the patient to form a 3D image. Sometimes SPECT is followed by a low dose CT scan (SPECT/CT); the two sets of images are then fused to enhance anatomical localisation. The main advantages of SPECT/CT are represented by better attenuation correction, increased specificity and the accurate depiction of the localisation of abnormal uptake/disease and of possible involvement of adjacent structures eg. bone scans. Furthermore, SPECT/CT is especially helpful in aiding the planning of minimally invasive surgery as it assists in pre-surgical localisation eg. parathyroid imaging. 1.3 Process of Initiating a Nuclear Medicine Scan To request a Nuclear Medicine Scan, complete the Nuclear Medicine Request Form QF002787. This form is also available on the CDHB Intranet. Note that the patient’s weight is a mandatory requirement for most scans. Deliver or fax the form (ext. 80869) to the Nuclear Medicine Department. For urgent scans during working hours (Monday – Friday 0800 – 1700), telephone the Scanning room (ext. 80867) after faxing the requisition. Urgent requests are performed as soon as possible. Availability: All efforts are made to scan patients within the requested time frames indicated on the referrals. Some scans are only available on certain days and others are not routinely available (refer to individual scans in Imaging Procedures). Discuss with Nuclear Medicine staff before ordering these scans. 1.4 Reports Most Nuclear Medicine scans are reported within 48 hours. All scan reports are available on Éclair and CIS, and both the images and report are available on PACS. Contact the Nuclear Medicine Physician for urgent reports and clinical discussion. 1.5 Radiation Dose Most nuclear medicine diagnostic scans use a radioactive material called Technetium-99m. Technetium has a short half-life of only 6 hours. The short half-life means that even for Technetium-based radiopharmaceuticals that don’t clear rapidly from the body, the patient will receive only a small radiation dose. Radiation dose can be described in terms of a quantity called ‘effective dose’, which is measured in millisieverts (mSv). For the procedures listed below, an average effective dose is quoted. For comparison, the annual natural background radiation level is about 2 mSv per year. This average level varies according to which part of the country you live in. X-Ray Examination NM Investigation Chest X-ray Plain Abdominal X-ay 0.05mSv 1.5 mSv Lumbar Spine X-ray Lumbar Spine CT IVU CT Abdomen & Pelvis 2.0 mSv 3.5 mSv 4.0 mSv 15.0 mSv Thyroid Scan Perfusion Lung Scan 0.8 mSv 0.9 mSv Renogram Bone Scan 0.5 - 1.4 mSv 3.7 - 5.0 mSv Note: figures are based on adult doses. Please contact the medical staff in the department if you require further advice or assistance with explaining risk estimates to patients. In Nuclear Medicine every precaution is taken to ensure exposure to radiation is; Low: only small quantities are used for diagnosis. Short: the radioactive compounds used in diagnostic tests are quickly eliminated from the body. Carefully Controlled: facilities, equipment and materials meet strict safety standards. 1.6 The "Nuclear Medicine Study" Notice Although many nuclear medicine investigations don’t require any special nursing precautions, for most in-patient scans a “Nuclear Medicine Study” notice is issued before the patient leaves the Nuclear Medicine Department. This notice gives recommendations on how to minimise any radiation hazards associated with caring for these patients. They are based on a conservative approach to minimising hazards, and it is important to note that they only apply for the day of the procedure. 1.7 Accompanying Staff and General Nursing Care If possible do not schedule elective procedures on the same day as the scan e.g. OT, endoscopy. Please consult with Nuclear Medicine if there is a problem. For most diagnostic tests, no specific extra nursing care is required except that required by the patient’s clinical condition. This does not apply to radionuclide therapy, for which there are special procedures (consult the leaflet accompanying the patient). For diagnostic tests the risk to staff is extremely low. Even a small distance between nurse and patient greatly reduces the radiation dose received. This should be noted by escorts accompanying patients for nuclear medicine studies. Although there is unlikely to be a significant hazard to the foetus of pregnant escort nurses, it is sensible to avoid unnecessary radiation to a foetus. Please do not send a pregnant nurse as escort if at all possible, and do not direct a pregnant nurse to give continuous, close nursing care (‘specialling’ the patient) during the first 12 hours after a patient has been administered a diagnostic radiopharmaceutical. The patient does not need to be nursed separately from other patients. Patients from outlying hospitals must be accompanied by an appropriately trained staff member at all times. Prior arrangements can be made in consultation with Nuclear Medicine Staff, for a suitable place to wait during the period between injection and the scan. While every effort will be made to minimise the length of time the patient will be away from the ward, accompanying staff should be aware of and be prepared for unavoidable and occasionally long delays. 1.8 Body Fluids In some investigations urine or vomit may be slightly radioactive for a short time. This constitutes no danger to nursing staff provided they handle the body substances in an approved manner. Deal with them as biohazard, using Universal Precautions, i.e. wear gloves, dispose of correctly and wash hands. Flushing bed pans and vomit bowls down the sluice is acceptable. Catheter bags may be emptied into a sluice or toilet and the urine flushed away. Contaminated bed linen should be placed in a red linen bag and sent to the laundry. It is preferable that a 24-hour urine collection is not made within the day after a nuclear medicine investigation. If this is unavoidable, a “radioactive‟ sticker can be provided by the department to inform any staff handling the specimen of the radionuclide it contains. The specimen should be placed in a side room on the ward where no one will stand beside it for long periods. It should be taken directly to the laboratory when collection is complete. The laboratory staff should also be warned, in case the radioactivity should interfere with their analyses. Any spill of urine (or vomit), or any body fluid should be thoroughly washed from the skin and cleared from floors, etc, as is normal for a biohazard. As with any spillage, it is important that it is contained as soon as possible and not spread around the ward. However, appropriate patient care always has priority. If any staff are concerned about adequate decontamination following a spill they should contact the department. 1.9 Patient Preparation Most investigations within this department require little or no patient preparation (see Imaging Procedures). The patient will need to be transferred onto an imaging bed. If the patient weighs over 180kg or specialised lifting equipment is required then inform the Nuclear Medicine staff when booking the scan. If the patient is unable to tolerate lying still for the length of the scan due to pain, then medication will need to be administered before the start of the scan. If you think that it may be necessary to use sedation (usually reserved for small children with long scan times), please discuss with Nuclear Medicine staff when booking the scan. For some tests eg. Bone scan or Renogram, it is important that the patient is well hydrated. If a patient is unable to drink, IV fluids may need to be given. Some Nuclear Medicine scans may require a period of fasting prior to the study eg. Biliary scan. Specific instructions will be given, as appropriate. The iodine in contrast media used in radiology may block uptake by the thyroid of the radiopharmaceuticals used in thyroid or parathyroid scans. It is preferable to perform these scans before one that involves contrast media, otherwise the Nuclear Medicine scan may have to be postponed for several weeks. There are also medications which must be avoided before specific scans because they can interact with the radiopharmaceutical given (refer to individual scans in Imaging Procedures). In most circumstances, an IV luer is not required. However, babies, young children and adults with difficult venous access may require an IV luer to be inserted by Paediatric Outpatients or by ultrasound guidance prior to the radiopharmaceutical injection. 1.10 Patient Information The patient will receive an explanation of the test from departmental staff. However, as many patients have no idea what is involved, it is preferable for them to receive some information at the time the test is requested or booked. Patient information sheets are faxed to the ward when a scan is booked and they should be given to the patient. An explanation of the test by a member of the medical or nursing staff should be given at the same time. Outpatients are sent letters specific to the type of scan they are having, as well as a general information brochure. The brochures are also available in the CDHB Nuclear Medicine website. It is particularly important that a pregnant or breastfeeding woman receives an explanation about the test, or the necessity to interrupt breastfeeding before she comes to the department. Pregnancy and the postpartum period are an emotionally stressful time, and radiation in pregnancy has received negative publicity. The patient may wish for the advice and support of her partner. This is not always available if the explanation of the nature of the test is left until just before the investigation. 1.11 Examination of Pregnant and Breastfeeding Women If necessary, some tests can be performed on pregnant women, for example, lung scans for thromboembolic disease. Pregnancy is not an absolute contraindication to radionuclide investigations, but routine tests should not be performed on pregnant women if the result will not affect immediate management and they can be delayed until after the end of pregnancy. A request for an investigation on a pregnant woman should be discussed by a senior member of the clinical team responsible for the patient with a senior member of departmental staff. Some radiopharmaceuticals are excreted in breast milk. If tests are essential during lactation then interruption of breastfeeding will be advised for a short period. This time depends on the pharmaceutical concerned. If possible, the baby should be fed immediately before the investigation. The mother should be encouraged to express breast milk during the period of interruption, both for comfort and to ensure continuation of the supply. This breast milk must be discarded. Please contact the department for further advice if you wish to perform a study on a breastfeeding mother. 1.12 Adverse Reactions There are very few adverse reactions to radiopharmaceuticals. As with any intravenous injections there is always a risk that allergic rashes or minor vasovagal episodes may occur. No specific remedy is required, just symptomatic treatment. However, please report any suspected reaction to the Nuclear Medicine Department.
![The Politics of Protest [week 3]](http://s2.studylib.net/store/data/005229111_1-9491ac8e8d24cc184a2c9020ba192c97-300x300.png)