VASCULAR SURGERY CURRICULUM
advertisement

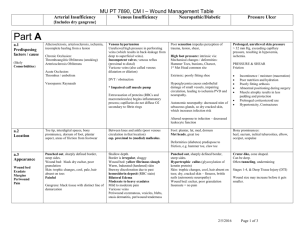
VASCULAR SURGERY CORE CURRICULUM: V-CORE Each content area, where applicable, will be organized as follows: DISEASES AND CONDITIONS I. Definition II. Epidemiology III. Etiology IV. Pathology / Pathophysiology V. Signs and symptoms VI. Differential Diagnosis VII. Diagnosis A. History and Physical examination B. Appropriate Tests / Imaging VIII. Treatment Options A. No treatment 1. Prognosis 2. Outcomes B. Medical Management C. Interventions 1. Anatomy a. Endovascular - Access site(s) - Arterial path to intervention b. Open: surgical exposures and options 2. Endovascular Surgery a. guide wires b. sheaths / catheters c. balloons d. stents e. stent grafts f. thrombolysis – lytic agents g. other. – laser, atherectomy, cryotherapy 3. Minimally Invasive Techniques a. laparoscopic surgery b. combined endovascular / open surgery 4. Open Surgery a. thromboembolectomy b. endarterectomy c. direct repair – i.e. aneurysmorrhaphy d. patch angioplasty e. bypass - in-line anatomic bypass - extra-anatomic bypass - conduit 1. vein 2. graft a. prosthetic b. other D. Complications 1. Acute graft occlusion 2. Graft stenosis and Graft degeneration A. Myointimal hyperplasia B. fabric tears C. graft aneurysm formation 3. Infections a. wound b. graft 4. Others a. cerebrovascular accident b. pneumonia c. PE d. paralysis e. mesenteric ischemia f. renal failure g. limb loss h. bleeding i. death IX. Prognosis / Outcomes X. Basic Science (where applicable) Every section highlighted in yellow will have an editor. VASCULAR MEDICINE I. Diabetes Mellitus A. Hemoglobin A1C levels B. Oral agents C. Injectable insulin; insulin pumps for DM 1 1. Pre-op 2. Sliding scale II. Hypertension A. Medications – po / IV III. Hypercholesterolemia A. HDL / LDL – ratios for treatment B. Oral agents – 1. Mechanisms of action 2. Goals 3. Complications IV. Tobacco Use A. Cessation programs B. Medications V. Risk Reduction A. Pre-operative screening 1. Cardiac work-up a. EKG b. Echocardiography c. Stress testing – echo / nuclear B. Pulmonary 1. COPD 2. PFTs VI. Medical Management of Peripheral Arterial Disease (PAD) VII. Chronic Kidney Disease A. Increased Creatinine 1. Management for endovascular and open surgery B. Post-op management – acute / chronic VIII. Hypercoagulable States A. Work-up – panel of tests B. Treatment / Management 1. Pre-op 2. Intra-op 3. Post-op IX. Antibiotic therapy: The Basics X. Erectile Dysfunction A. DDx – arterial, venous, neurological, psychological B. Diagnosis C. Treatment XI. Non-Atherosclerotic Diseases D. Raynaud’s Syndrome E. Vasculitis (Takayasu, GCA, Behcet) F. Arteriopathies 1. Marfan’s syndrome 2. Ehlers-Danlos syndrome 3. Cystic medial necrosis 4. Pseudoxanthoma elasticum 5. Arterial magna syndrome G. Congenital Conditions 1. Abdominal coarctation 2. Persistent sciatic artery 3. Popliteal entrapment syndrome 4. Fibromuscular dysplasia 5. Adventitial cystic disease 6. Compartment syndrome 7. Homocystinuria XI. Embryology of the Vascular System: The Basics CRITICAL CARE – A. General: homeostasis; fluid and electrolyte management; blood transfusions; metabolism and feeding; malnutrition/nutrition; surgical aspects of diabetes; management of hyper and hypoglycemia; hemodynamic monitoring, mechanical ventilation; anticoagulation; management of shock; management of systemic sepsis; SIRS, surgical infections, antibiotic therapy; wound healing; immune response to surgery and its complications B. Intracranial/Neurologic-cerebrovascular: intracranial hemorrhage, mass lesions, hydrocephalus, seizures, hyperperfusion syndrome, cerebral edema, acute stroke (including lytic therapy) C. General D. Cardiac: arrhythmias; CHF; diastolic dysfunction; acute coronary syndromes; non STEMI; valvular disease (AS, MR); echocardiography; Swan-Ganz catheterization and management E. Pulmonary: basic airway management; ventilator management; PE; acute pulmonary failure; ARDS; pneumonia/sepsis; COPD and emphysema, acute exacerbation; bronchodilators F. Hepatic: cirrhosis; jaundice; shock liver; coagulopathy; variceal hemorrhage G. GI: small bowel obstruction and perforation; ulcer disease (perf, penetration); stress gastritis; colon obstruction and pseudoobstruction; Ogilvie’s syndrome; volvulus; small bowel ischemia; ischemic colitis; clostridium difficile colitis H. Renal: acute renal failure; RRT; volume overload; hypovolemia I. Extremity: DVT; compartment syndrome; rhabdomyolysis J. Skin and soft tissue: gangrene (dry, wet synergistic); necrotizing fasciitis; skin, soft tissue, and wound infections; venous, arterial, and other ulcers K. Heme: management of acute bleeding and clotting disorders; hypercoagulable states; HITT VASCULAR SURGERY All sections include treatment of acute and chronic disease as well as follow-up and reinterventions for recurrent symptoms and/or disease. I. Cerebrovascular Editor: A. Carotid 1. Occlusive disease – emboli (TIA, AF, CVA), occlusion a. Management of asymptomatic and symptomatic disease based on percentage of stenosis 2. Dissection 3. Aneurysm 4. Carotid body tumor B. Vertebral 1. VBI 2. Embolic disease C. Intra-cranial 1. Circle of Willis a. components b. complete versus incomplete and implications D. II. Concomitant diseases (Aneurysm, AVM, occlusive diseases)FMD Thoracic Aorta A. Aortic Arch Disease – vasculitis B. Ascending Thoracic Aorta – aneurysmal disease C. Descending Thoracic Aorta 1. Aneurysmal disease 2. Dissection 3. Trauma – pseudo aneurysm 4. Occlusive disease – emboli 5. Intramural hematoma 6. Penetrating aortic ulcer III. Upper Extremity A. Occlusive disease – ischemia and emboli B. Aneurysmal disease IV. Thoracic Outlet Syndrome: arterial, venous, neurogenic V. Mesenteric: Celiac / SMA A. Entrapment/compression: Median arcuate ligament syndrome B. Occlusive disease – mesenteric ischemia 1. chronic arterial 2. acute arterial 3. SMV thrombosis C. Aneurysms D. Dissection VI. Renal Artery A. Occlusive disease 1. Hypertension 2. Renal insufficiency B. FMD C. Aneurysms 1. Peripheral 2. Hilar VII. Abdominal Aorta – including supra-celiac, supra-renal and infra-renal A. Aneurysms 1. Elective 2. Ruptured 3. Infected 4. Fistula (caval and enteric) 5. Emboli 6. Thrombosis B. Arteritis VIII. Iliac Arteries A. Aneurysms – CIA, IIA B. FMD IX. Aorto-iliac Occlusive Disease – combined disease with treatment options X. Lower Extremity A. Occlusive disease (acute versus chronic) 1. Emboli 2. Claudication 3. Limb threatening ischemia (CLI) B. Aneurysms 1. Femoral 2. Popliteal 3. Pseudo aneurysms – with and without infection XI. Portal Hypertension XII. Wound Care Management A. Wound types – ulcers 1. Venous 2. Arterial 3. Diabetic 4. Neuropathic 5. Infectious 6. Traumatic 7. Malignant 8. Hypertensive 9. Other – Rheumatic, sickle cell, inflammatory (pyoderma), B. Debridement C. Dressings – including VACs D. HBO E. Whirlpool F. Allografts, xenografts, skin grafts, and other methods/materials for coverage G. Tissue flaps and free flaps H. Wound care center XIII. Venous Disease A. Coagulation Cascade B. DVT and Venous thromboembolism C. Chronic venous insufficiency D. Varicose veins – Management 1. Medical 2. Sclerotherapy 3. Endovascular 4. Open surgical XIV. Angio-access A. Indications – ESRD, nutrition B. AVF vs AVG C. Salvage and Maintenance D. Catheters E. Complications (steal, infection, pseudoaneurysm) XV. Lymphatic Disease – Primary and Secondary XVI. Vascular Trauma A. Evaluation – non-arteriographic and arteriographic B. Penetrating Injuries 1. Carotid 2. Vertebral 3. Upper / Lower Extremities 4. Thoracic Aorta 5. Abdomen – celiac, SMA, renal arteries, iliac arteries, etc C. Blunt Injuries 1. Carotid and Vertebral 2. Upper / Lower Extremities 3. Thoracic 4. Abdominal Arteries 5. Orthopedic Injuries – i.e. posterior dislocation of the knee D. Concomitant Venous Injuries – to repair or not to repair E. Complications 1. Of Catheterization manipulization 2. Reperfusion syndrome 3. Compartment syndrome F. Spinal exposures XVII. Amputations A. Appropriate Amputation Levels B. Toe and TMA C. Through knee amputations D. AKA E. BKA F. Hip disarticulation G. Upper extremity amputations VASCULAR IMAGING AND PHYSIOLOGIC TESTING. A. Non-invasive Vascular Laboratory 1. Fundamental hemodynamics 2. Carotid / Vertebral 3. Upper / Lower Extremity – Duplex and Physiologic 4. Renal / Mesenteric 5. Venous – DVT, venous mapping 6. Abdominal – aorta, EVAR follow-up 7. Aneurysm – AAA, femoral, Popliteal 8. Pseudo-aneurysm diagnosis and treatment (compression and injection) 9. Vascular bypass / stent follow-up imaging and velocities 10. AV Access follow-up B. Axial imaging: 1. CT / CTA – cross sectional and 3D reconstruction – computer remodeling and interpretation 2. D. MR / MRA – cross sectional and 3D imaging and interpretation Angiography: 1. . techniques and interpretation a. Arch and carotids b. Vertebrals c. Intra-cranial d. Upper / Lower Extremity e. Thoracic Aorta f. Celiac / SMA g. Renals h. Abdominal Aorta and Iliacs i. Endoleaks j. Venous – extremities, IVC (Filters), AV Access 2. Intra-Operative Imaging - Duplex, Angiography 3. IVUS, TEE 4. Radiation Safety: The Basics MISCELLANEOUS: A. Basis of Contract Negotiations B. Practice Management C. Coding and Billing ______________________________________________________________ OPERATIONS AND PROCEDURES – Including Endovascular and Open Surgical (2008 CPT Code Book on Pages 157 to 180) We also need to include amputations, skin grafts, etc, which are elsewhere in CPT book. Should we use RRC Case Log format, or CPT Code Book? I would favor the latter.