Fractures of the thoracolumbar spine
advertisement
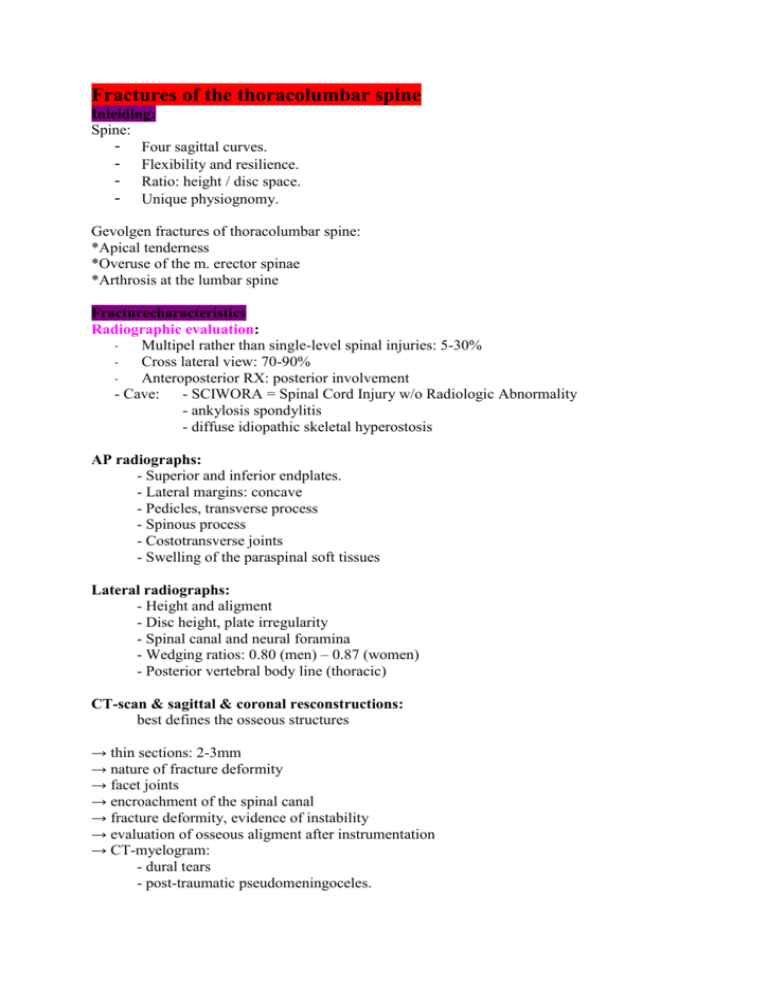
Fractures of the thoracolumbar spine Inleiding: Spine: - Four sagittal curves. - Flexibility and resilience. - Ratio: height / disc space. - Unique physiognomy. Gevolgen fractures of thoracolumbar spine: *Apical tenderness *Overuse of the m. erector spinae *Arthrosis at the lumbar spine Fracturecharacteristics Radiographic evaluation: Multipel rather than single-level spinal injuries: 5-30% Cross lateral view: 70-90% Anteroposterior RX: posterior involvement - Cave: - SCIWORA = Spinal Cord Injury w/o Radiologic Abnormality - ankylosis spondylitis - diffuse idiopathic skeletal hyperostosis AP radiographs: - Superior and inferior endplates. - Lateral margins: concave - Pedicles, transverse process - Spinous process - Costotransverse joints - Swelling of the paraspinal soft tissues Lateral radiographs: - Height and aligment - Disc height, plate irregularity - Spinal canal and neural foramina - Wedging ratios: 0.80 (men) – 0.87 (women) - Posterior vertebral body line (thoracic) CT-scan & sagittal & coronal resconstructions: best defines the osseous structures → thin sections: 2-3mm → nature of fracture deformity → facet joints → encroachment of the spinal canal → fracture deformity, evidence of instability → evaluation of osseous aligment after instrumentation → CT-myelogram: - dural tears - post-traumatic pseudomeningoceles. MRI: complementary information - intervertebral disc - spinal ligaments - thecal sac - epidural haematome - cord damage - pathological fracture: tumor & infection. - paravertebral soft tissues Myelography:= contraströntgenogram vh RM en de subarachoïdale ruimte - same indication as those for MRI - particular useful: - nerve root avulsions - dural tears Classification: - A comprehensive classification of thoracic and lumbar injuries F. Magerl - Load Sharing Classification R. Gaines Classifications: based on pathomorphological criteria Magerl et al. 1994 Categories: - according to the main mechanism of injury Compression (Type A) Distraction (Type B) Axial torque (Type C) - pathomorphological uniformity - progressive scale of morphological damage severity of injury expressed by its ranking Pathology: Flexion-trauma (90%) - Anteriorly: Vertebral body disc - Anteriorly & posteriorly: posterior arch ligaments - Anteriorly & posteriorly & rotation facetjoints ligaments typeA typeB typeC Anterior Column Fracture of the vertebral Body Disruption of the Disc Posterior Column Fracture Rupture of the Ligaments Signs of Rotation Type A Type B Type C Type A fractures Spinal canal clearance: < 4 days: correction to 60% > 4 days: correction to 30% Type B fractures Flexion-distraction Chance fracture = Horizontal fracture through the spinous process, laminae, pedicles and vertebral body Type C fractures common characteristics: - two-column injuries - potential for translational displacement in all directons of the horizontal plane - disruption of all longitudinal ligaments and/or discs - fractures of articular processes, usually unilateral - rib dislocations or fractures close to the spine - fractures of the transverse processes - lateral avulsion fracture of the endplate - irregular fractures of the neural arch - asymmetrical fractures of the vertebral body Slide 30 en 31 incidentie en kans neurology Modified Frankel Functional Classification (Eismont 1983) A1: A2: B: C: D1: D2: complete motor & sensory loss complete motor & sensory loss sacral sparing lower extremity sensation, no motor function presence of sensation trace of motor power, not useful useful motor function to allow walking with orthoses motor strength allowing walking without appliances E: normal function abnormal reflexes and spacticity may be present ASIA Classification: American Spinal Injury Association Defines the level of neurologic injury as the most distal level with at least grade 3 motor function, consistent with grade D Spinal-cord injuries: < 8 h of injury Methylprednisolone: NASCI scheme. - Loading dose: 30 mg/kg - Maintenance dose: 5.4 mg/kg/h for 23 hours. 1.Central cord syndrome = A syndrome associated with traumatic injury to the cervical or upper thoracic regions of the spinal cord characterized by weakness in the arms with relative sparing of the legs and variable sensory loss. This condition is associated with ischemia, hemorrhage, or necrosis involving the central portions of the spinal cord. Corticospinal fibers destined for the legs are spared due to their more external location in the spinal cord. This clinical pattern may emerge during recovery from spinal shock. Deficits may be transient or permanent. 2.Anterior cord syndrome 3.Posterior cord syndrome 4.Conus medullaris syndrome & Cauda equine = neurologisch uitvalsverschijnsel bij hernia nuclei pulposi, spina bifida, bloeding in het wervelkanaal en dergelijke, waarbij mictie en/of defaecatie aandrang zijn opgeheven en paresen kunnen optreden 5.Brown-Séquard syndrome = A syndrome associated with injury to the lateral half of the spinal cord. The condition is characterized by the following clinical features (which are found below the level of the lesion): contralateral hemisensory anesthesia to pain and temperature, ipsilateral loss of propioception, and ipsilateral motor paralysis. Tactile sensation is generally spared. Load Sharing Classification A) Comminution involvement 1) <30% 2) 30%-60% 3) >60% B) Apposition of the fragments - minimal displaced - at least 2mm displacement <50% - at least 2mm displacement >50% C) Deformity correction - Kyphotic correction <3° - Kyphotic correction 4° to 9° - Kyphotic correction >10° => Score: ≥ 7 anterior surgery! Treatment Treatment posteriorly: Type A: kyphosis > 20° scoliosis > 10° Type B: posteriorly or combined procedure Type C: LSC >/= 7 Load Sharing Classification Cobb’s angle = hoek tss twee eindplaten (meetbaar door er loodrechten op te tekenen en de hoek daartss te meten maat voor scoliose Complete rotational burst fracture: Type C Hybrid allograft Treatment anteriorly: - anterior spinal canal decompression. - perform anterior stabilization when there is deficient bone anteriorly. - Burstfarctures of L3 or above with neurology. - Burstfarctures of L3 or above without neurology. Load Sharing Classification score ≥ 7 - Flexion-distraction injuries (2nd time). - Fracture-dislocations (2nd time). - Fractures due to metastatic disease. - Late posttraumatic kyphosis (flexible). Load Sharing Classification: Why? -> Recurrent kyphosis after removal of the implant. due to the Disc >>> vertebra -> Spinal canal clearance. < 4 days: correction to 60% > 4 days: correction to 30% correlatie kyphose follow-up met pre-operatieve kyphose: correlatie is 0,807; p<0,0001 Fractures of the thoracolumbar spine - Bony elements, ligaments - disc? Minimal invasive techniques: - Kyphoplasty seu vertebroplasty - Sextant-procedure - Endoscopic procedures Kyphoplasty seu vertebroplasty Kyphoplasty in Trauma: Founded in 1994 in California, US. First kyphoplasty in Europe in 1999. More then 22.000 Kyphoplasties already performed. X-Ray: AP & Lateral CT: fracture pattern posterior wall MRI: # indication The more recent the fracture, the better the result Procedure limited to: 1. Lumbar spine 2. Thoracic spine => Thoracic spine Transpedicular / Extrapedicular operatie Balloonkyphoplasty Biomaterial PMMA Calcibon Low viscosity Pressure injection High compressive strength Radiopaque Biodegraded Biocompatibility of Calcibon® Calcibon® PMMA lokaal hoopje verspreidt over trabekels Nadelen: *Fracture fragments will be crushed: - Movements - Not well fixed *Injection not under pressure! *Calcibon not well fixed Kyphoplasty & vertebroplasty: voordelen -> Minimal Invasive -> Restores Vertebral height -> Immediate pain relief -> Fast return to daily activities -> Preservation of disc function -> Prevention of disc problems and late kyphosis -> Safe Procedure Kyphoplasty: - Minimal invasive ‘kyphoplasty’ is indicated: A.1 & A1.2 fracture. B-type and A.3.1 fractures in combination with a posterior instrumentation. - Reduction of pain and hospital stay comparable with a vertebroplasty. - Calcibon is biocompatible. Vertebroplasty: leakage, no reduction of fracture possible Sextant-procedure: Sextant-procedure:L1: superior incomplete burst # Sextant: benefits - Minimally invasive posterior stabilization. - Minimal dissection and retraction. - No muscle stripping. - Complete preservation of posterior elements. - Minimal blood-loss. Endoscopic Approach 4 gaatjes Complete rotational burst fracture: Type C Conclusion: - A non anatomical result does not mean a poor functional result. - Treatment: Type A: posteriorly: controversial anteriorly: LSC Type B & C: posteriorly or combined (LSC) - Minimal invasive: Kyphoplasty seu vertebroplasty Sextant-procedure endoscopic-procedure (2nd-time) - Discs: endoscopic-procedure