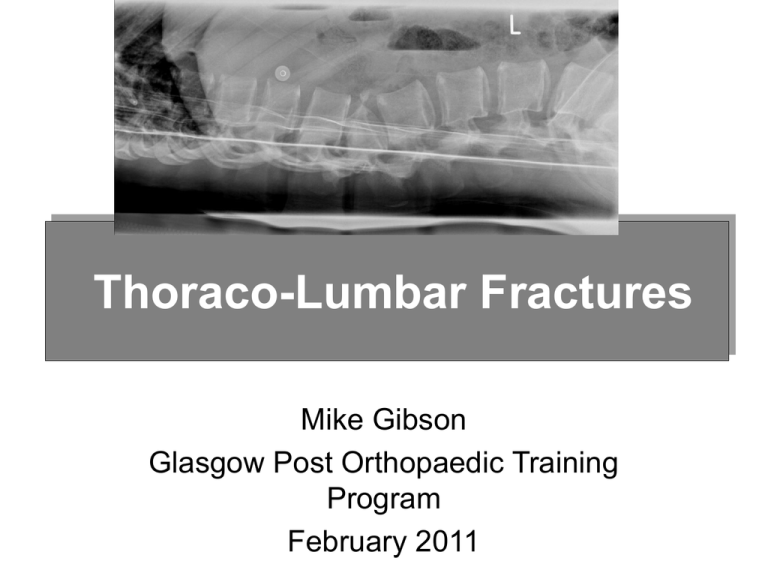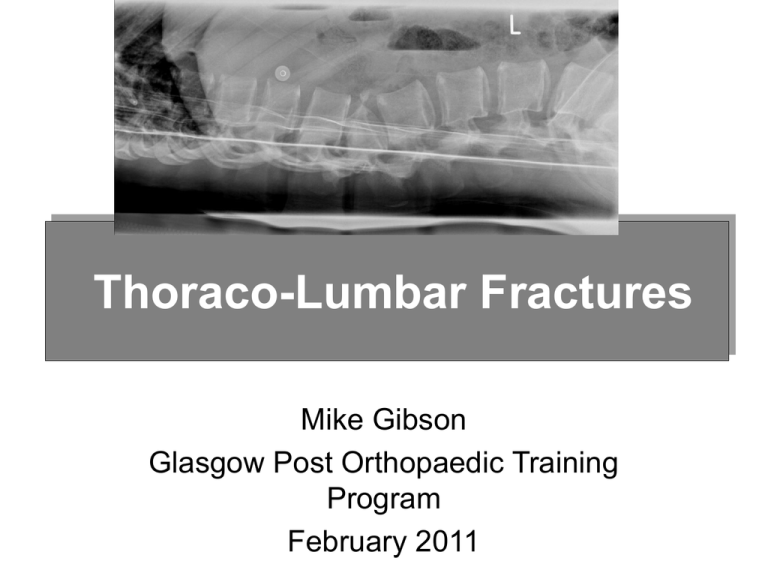
Thoraco-Lumbar Fractures
Mike Gibson
Glasgow Post Orthopaedic Training
Program
February 2011
Thoraco- Lumbar Fractures
•
•
•
•
•
•
Immediate Care and Assessment
Investigation
Classification
Non Operative Treatment
Surgical Treatment
Cases
IMMEDIATE CARE
• ATLS Protocol
–lateral XR’s thoracic and
lumbar spine
• Spinal board
• Log rolling
–enough people (5)
• High Index of Suspicion
Assessment of Spinal Fracture
• History
• Examination
• Imaging
X Rays
CT
MRI
Examination
• Vertebral assessment –
Log Roll
– Inspection of spine
• Bruising, deformity
– Palpation
• Localised tenderness,
step-off, anal tone &
sensation
Examination
• Neurological Assessment
– Motor - voluntary contraction of muscles, graded
• In unconscious involuntary movement to pain
• Compare both sides of body
– Sensation – soft touch in dermatomes
– Autonomic function – bladder/bowel control,
priapism
Clinical Features of Spinal Cord Injury
• Neurogenic Shock
– Disruption of descending sympathetic pathways
– Bradycardia, loss of smooth muscle tone
→hypotension (fluid overload : inotropes)
• Spinal Shock
– Loss of all cord function after injury causing
flaccidity & loss of reflexes
• Abnormal Breathing
– Lower Cx/upper thorx cause abd breathing & use
of intercostals
Trunk Control
• Patient will comfortably roll themselves
around the bed
• Useful sign of Stability ?
• Not early post injury
• Not in Intoxicated
• Not in Head injured or confused
Investigation of Spinal Trauma
•
•
•
•
Plain X Rays,
CT to Characterise the Fracture
MRI if Neurological Deficit
Standing X rays
Definition
of
Instability
DEFINITION OF INSTABILITY
When subjected to normal
physiological forces the fracture
will not displace sufficiently to
produce neurological deficit or a
significant deformity.
CLASSIFICATION SYSTEMS
Convey information
Produce treatment
plan
Monitor patient
progress
Research tool
CLASSIFICATION SYSTEMS
Spinal Column Injury
Spinal Cord Injury
2 Column Classifications
• Holdsworth
• AO
3 Column Classification
Denis
Anterior - Ant 1/3 of disc /VB
+ ALL
Middle - Post 1/3 of disc/VB
+ PLL
Posterior - Post Elements
Spinal Cord Injury
Accurately Document Neurological Status
Remember SPINAL SHOCK
Prognosis of deficit at 48hours
Spinal Cord Injury
FRANKEL
A
No motor
B
No motor
C
Motor(2-3)
D
Motor(4-5)
E
Normal
No sensation
Min. sensation
Sensation
Sensation
Normal
Spinal Cord Injury
A.S.I.A.
A
Complete - no motor or
sensation
B
Incomplete - sensation, no motor
C
Incomplete - sensation, motor<3
D
Incomplete - sensation, motor3
E
Normal
Spinal Cord Injury
Clinical Syndromes:
Central Cord
Anterior
Posterior
Brown-Sequard
Conus/Cauda Equina
Spinal Cord Injury- Power
MRC Grade
0
1
2
3
4
5
none
visible contraction
contracts, not against gravity
contracts against gravity not
resistance
contracts against resistance
normal
CONCLUSIONS
• Core knowledge allows transfer of
accurate information
• Monitor patients neurological status
• Remember SPINAL SHOCK
• Research tool
AO Classification
AO 1994 (Magerl et al)
• Type A = vertebral body compression
posterior column intact
• Type B = anterior and posterior column
injuries with distraction
• Type C = anterior and posterior column
injuries with rotation
AO Classification
A
A1 =
A2 =
A3 =
Impaction # (wedge)
Coronal split #
Burst #
• axial compression forces +/- flexion
• mainly vertebral body
• no translation
AO Classification
B
B1 =
posterior ligamentous mainly
(flex-distract)
B2 =
posterior osseous mainly
(flex-distract)
B3 =
anterior disc disruption
(hyperextend-shear)
• bilateral subluxation/ dislocation
• facet fractures
• frequent neurological injury
C1 =
C2 =
C3 =
AO Classification
C
type A with rotation
type B with rotation
rotational shear injuries
• high neural injury rate
• rotation and translation
• facets, TPs, ribs, neural arch #s
• all ligaments
• discs
AO alphanumeric system
• Type A – vert body compression
• 1 impaction
• 2 split
• 3 burst
• Type B – ant & post element inj with distraction
• 1 ligament
• 2 bony
• 3 + ant disruption
• Type C – ant & post element inj with rotation
• 1 Type A + rotation
• 2 Type B + rotation
• 3 rotational sheer
Non – Operative Treatment
Options
No treatment
advice / restrict activity
Spinal ‘immobilisation’
Bed rest
Lumbar pillow / Log
rolling
Casting / Bracing
Combination treatment
THE AIMS OF TREATMENT
Prevent neurological deterioration
Minimise spinal deformity
Fracture healing
Minimise complications
Acceptable function
Indications - Clinical
•
Other skeletal injuries
•
Co-existing medical problems (Unfit)
•
Co-operative patient
•
Normal Trunk Control
•
Age of patient
•
Patient preference
Stable Burst Fracture (A3)
Stable A3 Fracture
• Bed Rest until Normal Trunk Control
• Standing X Rays
• ? Use extension Brace or Cast
Time for Conservative Treatment
Bed rest
range:
1-8
weeks
usual:
4-6
weeks
TLSO
range:
6 - 26
weeks
usual:
6 - 12
weeks
Complications
Bed rest sequelae
Respiratory compromise
Worsening of deformity
Neurological deterioration
Surgical Management
Thoraco-Lumbar Fractures
• Unstable
• Displaced
• Neurological
Deficit
SPINAL TRAUMA
Advantages of Instrumentation
• Simplify care
• Early mobilisation
• Improve
anatomical result
• Better
neurological
recovery?
Scoliosis Research Society
Multicentre Spine Fracture Study
Gertzbein Spine Vol 17;528-540
Gertzbein- Neurology
• Surgical had greater % improvement in
Function.
• At one year surgical group signifigantly
greater relative improvement in motor
score.
Score 69.2% vs 14 (p<0.00001)
• At 2 yrs
Score 59% vs 16 (p,0.00003)
Gertzbein - Pain
• Kyphotic Deformity < 30 degrees@ 2 yrs
had significantly more pain
• Overall surgical group had less pain than
non surgical group.
Neurological recovery
improved?
Fixation Techniques for T/L Spine
Choice of Approach
•
•
•
•
•
•
•
Provide optimal exposure,
Anatomically based,
Extensile,
Appropriate to pathology,
Safe,
Low morbidity,
Fast and simple.
Extensile Approach
Exposure that will vie effectively with the
“Great arsenal of chance” must be a
match for every shift, and therefore have a
range, extensile like the tongue of the
chameleon, to reach where it requires.
Henry A.K. 1957 Extensile Exposure. Livingstone,
Edinburgh.
Posterior Fixation of Fractures
•
•
•
•
Short Segment Fixation
Restoration of Sagittal Alignment
Stable Fixation
Maintain Correction
USS2 Fracture Set –
Fixation of A3 Fracture
Treatment of A fractures
• A1 Conservative
• A2 Mostly
Conservative
(Depends on
Displacement on
Standing X Rays)
• A3 ?Conservative if
posterior column
intact
Treatment of A3 Fractures
• Retropulsed fragment
relevant only if neuro
deficit! (Fidler 1987)
• Middle column does
not exist
A3 Fractures Indications for surgery
•
•
•
•
•
•
Neuro Deficit
Loss of 50% Ant body height
Kyphosis > 25 degrees
Canal Encroachment > 50%
Persistent Post Tenderness
Slow to regain trunk control
Posterior ligamentous disruption
A3 Fracture
Neurological Deficit
• Complete -Stable
Short Segment
Fixation usually Front
and back
• Incomplete- Posterior
fixation repeat CT
scan if necessary
second stage anterior
decompression
Canal Clearance post Surgery
Plus Transpedicular Bone Grafting
Treatment of B Fractures
• Difficult to diagnose
• Easy to fix
• Close gap in posterior elements to restore
tension band function of posterior
elements
Anterior Ligamentous Injury
Treatment of C Fractures
•
•
•
•
Grossly Unstable
Comminuted
Rotational Injuries
Usually Require either;
Longer Fixation
Front & Back Fixation
C Type Fracture L2
24 yr old cyclist 5 level spinal injuries
Timing of Surgery
• Optimal Conditions
usually next day
• Influence of
Associated Injuries
• Beware early Anterior
Surgery
Displaced Unstable Thoracic Fractures
• 50% have neurological deficit
• All have associated chest injury
• Chest condition deteriorates after 1st 24
hrs
• Early surgery simplifies patient care
• Displaced Sternal fracture always exclude
upper thoracic fracture
ANTERIOR INSTRUMENTATION
Indications in spinal trauma
• Anterior
compression with
progressive neuro
deficit.
• Late surgery.
• Anterior
decompression
required.
• Anterior column
support in
comminuted #
Anterior Compression with
Progressive Neurological Deficit
Late Surgery
Post traumatic kyphus + partial Neuro Deficit
Surgical Management
Thoraco-Lumbar Fractures
• Unstable
• Displaced
• Neurological
Deficit
Spinal Trauma Case 1
• 15 year old girl jumped/fell 30 feet
• Skull fracture small extradural
• Alert, orientated but irritable with
headache and minor meningism
• No neurological function below fracture
Spinal Trauma
• 50 year old woman
• Referred to spinal surgeon 3 weeks post
fracture
• Mechanism fall down 3 stairs
• Bilateral foot drops but still ambulant
• Neurological deficit apparently increased
Spinal Trauma
•
•
•
•
•
15 year old
RTA
Neurologically intact
2 Previous attempts at fixation failed
Referred for conservative treatment
Spinal Trauma
•
•
•
•
•
19 Year old Skiing Accident
Fracture L1 Treated in France
Neurologically Normal
Undisplaced A3 Fracture
Neurosurgical fixation
Spot the 7 mistakes
The 7 Errors
• Didn’t need Fixing
• Didn’t need
Decompression
• Rods too thin
• Screws too short
• Screws too thin
• Screws in fractured
vertebra
• Left L2 screw missed
Denis’ 3 columns