Title: Surgical management of the cutaneous
advertisement

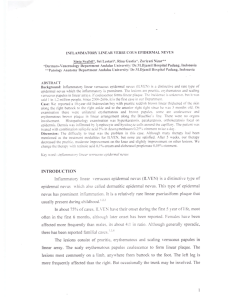
Title: Surgical management of the cutaneous manifestations of linear nevus sebaceus syndrome. Authors: Alexander Margulis, MD, Bruce S. Bauer, MD, and Julia F. Corcoran, MD. Linear nevus sebaceus syndrome (LNSS) is characterized by the association of linear nevus sebaceus with abnormalities of the central nervous system, eyes and bones, other cutaneous alterations and malignancies (1-3,16,17). The plaques of nevus sebaceus are hairless and verrucous, and the color ranges from yellow-orange in white individuals to hyperpigmented in black patients. Typically, the scalp and the face are severely involved. Patients with nevus sebaceous, whether associated with LNSS or solitary, have a 10 to 20 percent risk of the development of cutaneous neoplasia, especially basal cell carcinoma and syringocystadenoma pappiliferum (4,5). These tumors usually develop after puberty. While extensive literature describes the dermatologic, neurologic as well as ophthalmologic manifestations of LNSS, the surgical approach to these complex head and neck lesions has not been previously described. We present a cohort of 5 consecutive patients with diagnosis of linear sebaceous nevus syndrome with lesions covering extensive areas of the face and scalp, all were treated in our institution within the last 10 years. All patients were treated with expansion of the adjacent texture, color, and adnexal matched skin as the primary modality of treatment. Full thickness skin grafts, local skin flaps and prefabricated flaps were applied for reconstruction of specific areas. These techniques were based on experience gained in treating our previously published large series of congenital pigmented nevi (6). Case reports: Five consecutive patients presented in this review were diagnosed with linear nevus sebaceus syndrome based on the extensive head and neck sebaceous nevi associated with abnormalities of the central nervous system (primarily seizures and developmental delay), eyes and skeletal system. These were selected from a subset of over hundred patients treated for small, intermediate and large size sebaceous nevi of the head and neck. All of the patients were girls. The age ranged from 2 months to 3.5 years. Three patients who have been followed for 2 to 8 years are presented in detail. Discussion: Linear nevus sebaceus syndrome (LNSS) is characterized by the association of nevus sebaceus, covering extensive areas on the head and scalp, with abnormalities of the central nervous system, ophthalmologic and skeletal changes and malignancies (1,7). The incidence is approximately 1:10,000 live births, and there is no sexual predilection reported, although our series was exclusively females. Feuerstein and Mims’ original paper (8) was followed by extensive literature describing the dermatologic, neurologic and ophthalmologic manifestations of this disease. The objective of this report is to describe the surgical approach for the excision and reconstruction of giant sebaceous nevi of the face and scalp in children with LNSS. To our knowledge, this report represents the largest surgical series and suggests a reliable approach to the treatment of the cutaneous manifestations of this syndrome. Although the exact incidence and timing of malignant degeneration in giant sebaceous nevi is not known, most authors believe that patients with this condition, whether associated with LNSS or solitary, have a 10 to 20 per cent risk of development of cutaneous neoplasia, especially basal cell carcinoma and syringocystadenoma papilliferum (4,5). The malignant degeneration rarely occurs before the third decade of life, although earlier cases were described in the literature. There is little debate regarding the aesthetic deformity presented by large yellow-orange verrucous covering extensive areas of the face which become progressively verrucous over time, especially couple of years before and during the puberty. For these reasons, we strongly feel that multistage excision of as much nevus as possible and carefully planed reconstruction are indicated in children with LNSS and are not precluded by other, usually serious medical conditions associated with the syndrome. Although extensive review of the central nervous abnormalities is beyond the objectives of this review, there are few points of greater importance when caring for these patients. Seizures, either generalized or focal, occur in 76 percent of patients with LNSS. Patients with widespread involvement of the head, neck and the upper trunk are affected most frequently. Seizures begin during the neonatal period when the patient has extensive CNS involvement, but may not begin until 3 years of age with less significant CNS alterations (1). Developmental delay is found in up to 60 percent of patients and correlates with abnormal cranial CT and MRI scans. Macroencephaly, paresis, cortical atrophy and variety of tumors involving the nervous system have been noted (8-11). Thorough neurologic evaluation and control of the seizures are mandatory prior to surgery. Our practice has been to delay surgery until patients are seizure free or until seizure disorder is relatively stable for at least six months to avoid secondary neurologic damage in the perioperative period. Skeletal alterations are found in 68 percent of patients with LNSS. Kyphoscoliosis is the most common skeletal anomaly but may not become evident until late childhood. Hemihypertrophy and other deformities of the extremities, such as pas equinovarus, genu valgum, bone hypoplasia and syndactily can occur (1,13). Osteolytic lesions and fractures have developed occasionally, and vitamin D-resistant rickets has been reported (12). Tissue expansion has given surgeons the capability to harvest large flaps of color-, thickness- and texture-matched skin while simultaneously minimizing donor site defects. Since its introduction, tissue expansion has been used to solve a wide variety of reconstructive problems, with a significant increase in the refinement of its application (15). All the patients in this series were treated with an expansion of the adjacent skin as the primary treatment modality. Traditional methods such as skin grafting, although providing acceptable coverage for upper face reconstruction in the adult population, rarely provide optimal results in children, even when entire aesthetic units are grafted. Tissue expansion and flap design must be optimized to ensure that the landmarks of the facial aesthetic units will be disturbed as little as possible. In particular, emphasis is placed on brow symmetry, hairline position, hair direction and scar orientation (6,14). The incision for the expander placement may be placed along border of adjacent normal skin or adjacent area in line with planned scar. We always use the largest expander possible beneath the uninvolved skin and occasionally even carry the expander under the lesion. Expanders are typically overexpanded as well. The lesions of nevus sebaceus typically appear as one or two wide nevi on the scalp and forehead with multiple additional thin linear segments vertically positioned on the face. Midline linear lesions are common. This unique configuration allows partial or complete excision of these linear segments when expanders are being placed and again when the expanded flaps are transposed, in order to minimize the overall number of surgical procedures. Philosophically, the plan is to excise as much of the large nevus segments as possible along with many of the thinner linear areas early, leaving final excisions and grafting to ear until an older age. Simultaneous scar revisions can be completed in those procedures. Reconstruction of the entire cheek aesthetic unit is a difficult problem in pediatric population. There is a little skin laxity to allow local advancement of “face lift” type flaps. Skin grafts on the cheek often result in very poor aesthetic and functional outcome in these growing patients. In one patient in our series, reconstruction of the entire cheek unit was achieved by staged transposition of a prefabricated expanded flap from the lateral neck and shoulder area. Although technically demanding, this technique provided a large flap matched for color and texture for resurfacing of the entire cheek, that can be further reexpanded once in place. Skin grafts can be used in specific areas with aesthetically pleasing results which stand up to growth over time (15). Large expanded full thickness skin grafts are invaluable in obtaining single unit, color compatible skin coverage of the periorbital and nasal areas. Skin grafts are also frequently used to resurface the non hair bearing areas above and posterior to the auricle, after advancing expanded scalp flaps to reconstruct the hairline. The ear itself can be covered with full thickness skin graft in a staged fashion starting when the child is 5 years of age. Larger anterior surface coverage has been accomplished using a near total postauricular full thickness skin graft from the contralateral ear (for optimal color match). The postauricular donor site is closed with a full thickness skin graft harvested from the groin. While we would suspect a higher rate of infection in these patients, to date, none of the serial intralesional excisions, of either the larger nevi or linear strips, have been complicated by wound separation or delayed healing. All children are covered with a broad spectrum antibiotic at the time of expander placement and continued until drain removal (5-7 days). In these cases, in particular, our threshold for resuming antibiotic coverage if irritation or excoriation of any of the lesions occur, is low. Given the scattered distribution of these complex lesions, long term follow up is required to assure that minor areas of residual lesion are monitored to minimize risks of malignant degeneration. These small residual lesions should be of a size that later treatment under local anesthesia would be possible, but simultaneous (and medically indicated) excision may be carried out under general anesthesia along with revision of some of the scars from the prior surgeries. References: 1. Paller, A.S. Epidermal nevus Syndrome. Neurol. Clin.. 5(3): 451, 1987. 2. Charles, N.C. Linear nevus sebaceous syndrome. Ophthalmology. 106(2): 207, 1999. 3. Yu, K.C., and Lalwani, A.K. Inner ear malformations and hearing loss in linear nevus sebaceous syndrome. Int. J. Pediatr. Otorhinolaryngol. 56(3): 211, 2000. 4. Domingo, J., and Helwig, E.B. Malignant neoplasms associated with nevus sebaceus of Jadassohn. J. Am. Acad. Dermatol. 1: 545, 1979. 5. Constant, E., and Davis, D.G. The premalignant nature of the sebaceous nevus of Jadassohn. Plast. Reconstr. Surg. : 258, 1972. 6. Bauer, B.S., Few, J.W., Chavez, C.D., and Galiano, R.D. The role of tissue expansion in the management of large congenital pigmented nevi of the forehead in the pediatric patient. Plast. Reconstr. Surg. 107(3): 668, 2001. 7. Lovejoy, F.H., and Boyle, W.E. Linear nevus sebaceous syndrome: report of two cases and a review of the literature. Pediatrics. 52(3): 382, 1973. 8. Feuerstein, R.C., and Mims, L.C. Linear nevus sebaceous with convulsions and mental retardation. Amer. J. Dis. Child. 104: 675, 1962. 9. Golitz, L.E., and Weston, W.L. Inflammatory linear verrucous epidermal nevus: association with epidermal nevus syndrome. Arch. Dermatol. 115: 1208, 1979. 10. Zaremba, J. Jadassohn’s naevus phakomatosis: a study based on a review of 37 cases. J. Ment. Defic. Res. 22: 103, 1978. 11. Gurecki, P.J., Holden, K.R., Sahn, E.E., et al. Developmental neural abnormalities and seizures in epidermal nevus syndrome. Dev. Med. Child. Neurol. 38(8): 716, 1996. 12. Goldblum, J.R., and Headington, J.T. Hypophosphatemic vitamin-D resistant rickets and multiple spindle and epitheloid nevi associated with linear nevus sebaceus syndrome. J. Am. Acad. Dermatol. 29(1): 109, 1993. 13. Muhle, C., Brinkmann, G., Muhle, K., and Heller, M. Skeletal involvement and follow up in linear nevus sebaceous syndrome. Eur. Radiol. 8(4): 606, 1998. 14. Gur, E., and Zuker, R.M. Complex facial nevi: a surgical algorithm. Plast. Reconstr. Surg. 106: 25, 2000. 15. Bauer, B.S., Vicari, F.A., Richard, M.E., and Schwed, R. Expanded fullthickness skin grafts in children: case selection, planning, and management. Plast. Reconstr. Surg. 92(1): 59, 1993. 16. Solomon, L.M., Fretzin, D.F., and Dewald, R.L. The epidermal nevus syndrome. Arch. Derm. 97: 273, 1968. 17. Solomon, L.M., and Esterly, N.B. epidermal and other congenital organic nevi. Curr. Probl. Pediatr. 6: 56, 1975.