Pediatric dermatology
Differences in adult and neonatal skin
Adult Skin
Neonatal Skin
Surface
Dry
Vernix (gelatinous)
Full thickness
2.1 mm
1.2 mm
Epidermal
thickness
> 50um
40-50 um
20-25 um in premature
Dermoepidermal
Junction
Ridged
Flat
Dermis
Normal
Less collagen &
elastic fibers
Melanosomes
Normal
Fewer
Hair
Normal
Less
Classification of pediatric skin diseases
Infective disorders:
Bacterial, Viral, Fungal
Infestations:
Scabies, Pediculosis, Parasitic
Inflammatory/ Immunological disorders:
Eczemas, Psoriasis, Lichen planus
Genetic/Nevoid disorders :
Hemangiomas, Linear epidermal nevus,
Epidermolysis bullosa, Tuberous sclerosis,
Neurofibromatosis, etc.
Neoplastic disorders:
Langerhans cell histiocytosis, Mastocytosis
Neonatal Dermatoses
Physiological
•
Vernix caseosa
• Mongolian spot
• Physiological scaling
• Sebaceous hyperplasia
• Sucking blisters
• Physiological jaundice
• Miliaria
• Milia
• Erythema toxicum neonatorum
• Transient neonatal pustulosis
• Neonatal Acne
Mongolian spot
Single or multiple slate gray or blue macules of
size 3 to 10 cms
Seen at birth
Seen over lumbosacral region, buttocks,
shoulders
Fade within the first 3-4 years of life
Physiological scaling
Seen in 75% normal infants
Occurs within first week of life
First around the ankles, later on hands and feet
and soon becomes generalized
Maximum intensity by eighth day, subsides by
3-4 weeks
No treatment required
Sucking blister
One or two solitary blisters
Present at birth
Seen over fingertips / hands / forearm
Caused by vigorous sucking
Heals rapidly without treatment within 2 weeks
of life
Differential diagnosis: Herpes simplex, Bullous
impetigo, Epidermolysis bullosa
Miliaria
Superficial vesicles resulting from sweat retention
in stratum corneum
A. Miliaria crystallina:
Following fever, phototherapy
Tiny clear vesicles seen over forehead, neck
Erythema absent
Peels off within 24 hrs
Miliaria
B. Miliaria rubra (prickly heat)
Seen in hot weather
Non follicular papules on erythematous base
1 to 4 mm in diameter
Trunk, face
Subside in 2 to 3 days
Itching, secondary infection is common
Infantile and Childhood dermatoses
Infective and inflammatory diseases have been
discussed in respective chapters. Certain common
and genetic-naevoid conditions seen in infants and
children will be discussed including:
Cradle cap, Diaper dermatitis
Nevus depigmentosus, Linear epidermal nevus
Haemangiomas, Vascular malformations
Sturge Weber syndrome
Neurofibromatosis, Tuberous sclerosis
Epidermolysis bullosa
Ichthyosis
Cradle cap
Seborrhoeic dermatitis of scalp
Thick, greasy, adherent scales on scalp
Commonly begins in the first 3 months
Self limiting
Apply oil for few hours to soften scales, rinse, 1%
hydrocortisone cream can be used
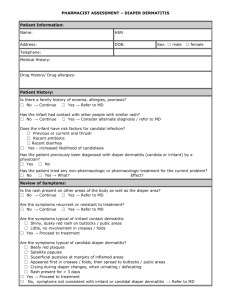
Diaper dermatitis (Napkin rash)
Irritant dermatitis in the perineal region
Due to occlusion, fricton and prolonged skin
contact with urine, faeces and fabrics
Wetness leads to maceration of skin
Secondary infection by C.albicans is common
Nevus Depigmentosus
Single, well circumscribed, hypopigmented or
depigmented macule or patch
Seen at birth
Stable in size and distribution
Seen over trunk and proximal extremities
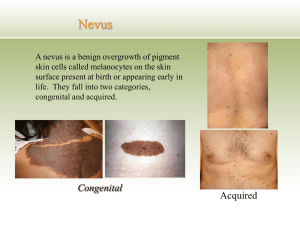
Linear epidermal nevus
Congenital hamartomas of embryonal ectodermal
origin
Seen in early childhood as a linear raised warty
lesion
Located over neck, trunk and extremities
Hemangiomas
Incidence more in preterm infants
Female predilection
Begin at one month of age
Undergo a proliferative phase followed by
stabilization and eventual spontaneous involution
Complications
Ulceration, bleeding
Secondary infection
Mutilation and scarring
Cosmetic disfigurement
Vascular malformations
Stable dilatations of superficial or deep
vasculature
Can be capillary, arterial, venous, lymphatic or
mixed
Clinical types:
Salmon patch
Portwine stain
Sturge-Weber syndrome
Klippel-Trenaunay syndrome
Salmon Patch
Present in 30 to 40% of neonates
Superficial, red or pink flat lesions
Seen over forehead, upper eyelid, glabellar area,
nape of neck
Resolution in first year of life
Portwine Stain (Nevus flammeus)
Present at birth
Common sites are face, neck and mucous
membrane
Flat pink-red lesion
Sharply unilateral in distribution
Persist in childhood and darker in adulthood
Complications
Glaucoma, Choroidal angiomas
Sturge-Weber Syndrome
Portwine stain in distribution of first branch of
trigeminal nerve
May be associated with seizures, ipsilateral
glaucoma, behavioral problems, mental
retardation
Characteristic intracranial S-shaped calcifications
Neurofibromatosis (NF)
Riccardi classified NF into eight distinct clinical
types in 1982
Autosomal dominant disorder
Affects skin, soft tissue, nervous system, bone,
other organs
Classical skin lesions are café au lait macules,
neurofibromas
Neurofibromatosis - 1
(Von Recklinghausen’s disease)
Diagnostic criteria for NF-1
Presence of two or more of the following:
Six or more café au lait macules larger than 5 mm
Two or more neurofibromas of any type or 1
plexiform neurofibroma
Axillary or inguinal freckling
Two or more Lisch nodules (brown coloured small
nodules on iris surface)
Optic glioma
A distinctive osseous lesion
A first-degree relative with NF-1
Neurofibromatosis - 2
Bilateral acoustic neuromas
Multiple CNS tumors
Few café au lait macules
Few neurofibromas
No axillary freckling
No Lisch nodules
Tuberous sclerosis (Bourneville’s disease)
Syn. EPILOIA (Epilepsy, Low IQ, Adenoma
sebaceum)
Ash leaf macules/ hypopigmented macules
Adenoma sebaceum (angiofibroma) begins at
2-5 years of age as small pink papules on midface
Shagreen’s patch (yellowish brown plaque on
lumbo - sacral area)
Koenen’s tumors (periungual fibroma)
Mental retardation
Seizures
Epidermolysis bullosa
Inherited bullous disorders characterized by
blister formation in response to mechanical
trauma
Onset at birth or shortly after
Seen on sites of trauma and friction
Types: Simple, Junctional, Dystrophic
Some subtypes, especially the milder EB forms,
improve with age
Autosomal recessive types have bad prognosis
with severe mucosal, esophageal involvement
and atrophic scarring of skin
Ichthyosis
Inherited disorder of keratinization
Characterized by the accumulation of scales on the
skin surface, dry skin
Fish like scales most prominent over the trunk,
abdomen, buttocks and legs
May be associated with ectropion, eclabion, nail
dystrophy, internal organ involvement
Types:
Ichthyosis vulgaris
X-linked ichthyosis
Lamellar ichthyosis
Collodion baby / Harlequin fetus
Adolescent Dermatoses
Acne
Dandruff
Striae
Pseudo-acanthosis nigricans
Contact dermatitis to cosmetics, perfumes,
artificial jewellery / accessories (metals)
Hyperhidrosis
Acne vulgaris
Characterized by comedones, papules, pustules
and nodules
Common in males
Seen around puberty
Sites: face, upper part of the chest, back,
shoulders
Complications
Psychological impact
Hyperpigmentation
Scarring
Dandruff (Pityriasis sicca/capitis)
Most common condition affecting the scalp
Causative organism: Malassezia species
Seen as mild, moderate or severe scaling of scalp
May or may not associated with itching
Simple dandruff does not cause hair loss
Striae (stretch marks)
Seen as pinkish white lines around knees, axillae,
outer aspect of thighs, lumbosacral region
Sudden increase in height or weight causes
rupture of connective tissue beneath an intact
epidermis
Pseudo-acanthosis nigricans
Weight gain in puberty produces dark, thick,
velvety skin in neck, axillae, groins
Asymptomatic
Side effects of cosmetic products
Cosmetic products like eye liner, ‘fairness’
creams, lipstick, nail polish, henna can produce
contact reactions
Reactions may be immediate or delayed
Types of reactions
Folliculitis
Acneiform eruptions
Contact dermatitis
Pigmentary changes
Child abuse
Includes physical abuse, neglect, sexual
exploitation
Cutaneous manifestations
Bruises
Traumatic
Thermal
alopecia
burns
Sexual
abuse: Vaginal tears, anal tears,
hematomas
Sexually
transmitted infections
Care of newborn
Gentle handling
Avoid frictional trauma
Use gentle soaps, cleansers
Too frequent bathing may lead to dryness
Maintain hygiene after feeds, diaper changes
Keep body folds dry and ventilated
Skin care in pre-terms
Gentle handling
Use adhesive tape sparingly
Avoid frictional trauma
General principles of skin care in children
Bathing, soaps and cleansers
There is no need to use special cleansing
products
Excessive cleansing, scrubbing and incomplete
rinsing lead to irritation
Shampoos
Should be isotonic to tears and less irritating to
eyes
Shampooing twice a week controls normal flaking
Care of the diaper area
Frequent diaper changes with gentle cleansing
and limiting use of plastic or rubber diaper cover
Differences in treatment of
Paediatric and Adult Patients
Conservative management is best
Surface area is more in children as compared
with adults
Percentage of absorption of topical drugs is
more
Try to use lowest effective dose of medications
Do not use treatments which may retard growth
or mental development
Avoid off-label uses of medications
Thank you